1. Introduction
Endovascular aortic aneurysm repair (EVAR) is widely regarded as a less invasive alternative to conventional surgery (1). However, anatomical limitations and aneurysm location may limit the number of patients who can be effectively treated with standard EVAR. It is estimated that 40% of patients are ineligible for conventional EVAR due to unfavorable neck anatomy (2).
In recent years, innovative techniques have been developed to treat patients with hostile proximal necks and aneurysms that extend beyond the renal arteries. These techniques include the use of fenestrated endografts (FEVAR), chimneys, snorkels, and other methods to create new landing zones and extend existing seal zones.
In cases with extremely hostile proximal landing zones, it may be necessary to cover the celiac trunk or the superior mesenteric artery (SMA), even in the presence of a patent collateral circulation network, to protect the patient from potential ischemic complications (3). However, unexpected events can still occur despite the presence of collateral circulation.
To our knowledge, we report the second case in the literature (4) of gallbladder necrosis following FEVAR.
2. Case Presentation
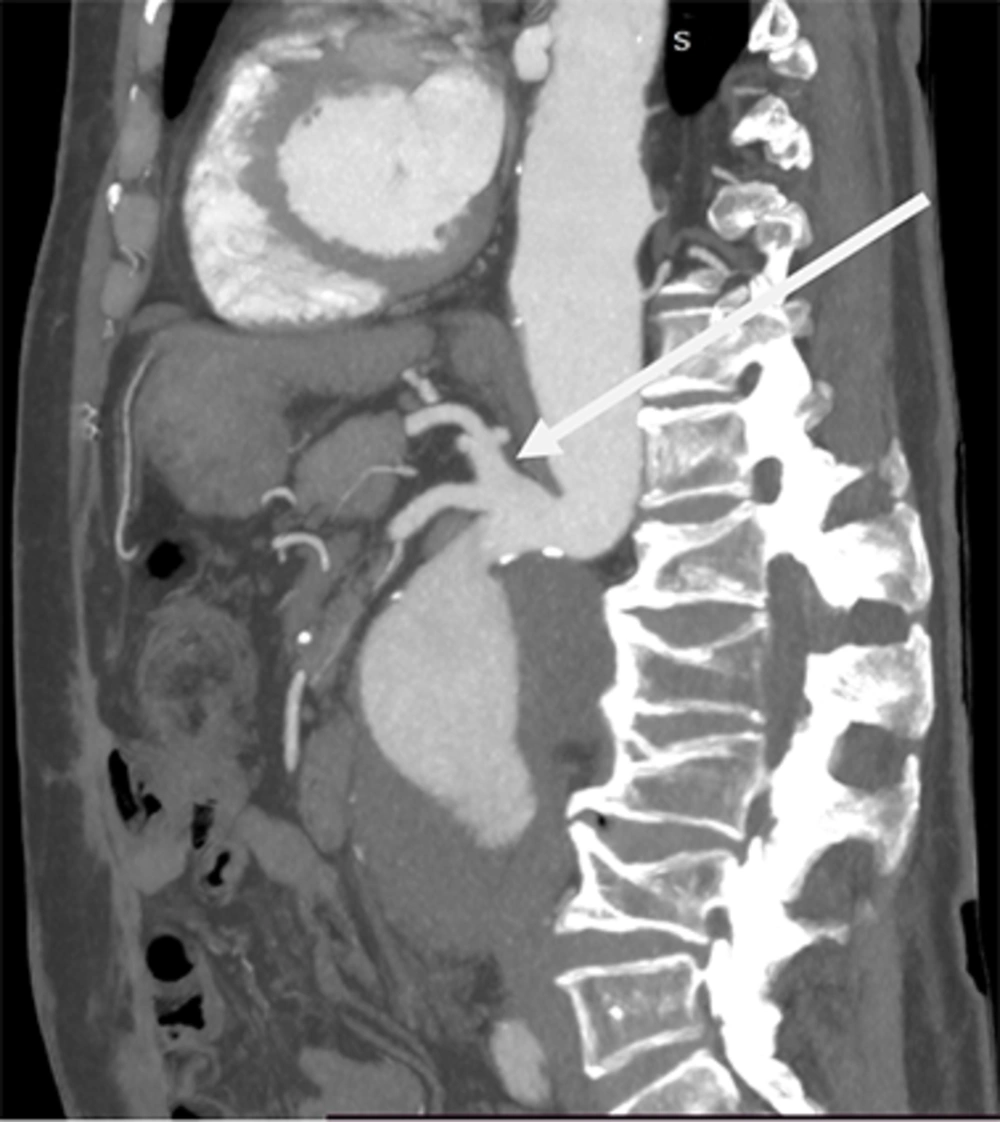
A 77-year-old male patient with a history of multiple abdominal surgeries, COPD, renal cysts, and global heart failure (with a left ventricular ejection fraction of 26%) consulted for abdominal pain that had persisted for 3 days. Physical examination revealed a pulsatile and expansive abdominal mass but no other symptoms. The patient was hemodynamically stable, and blood tests were normal. A computed tomography (CT) scan revealed a 70 mm juxtarenal aneurysm with an extremely hostile proximal neck due to an almost vertical aortic angulation (Figure 1). Both the celiac artery (CA) and the SMA originated from the same trunk (Figure 2). The CT also highlighted a large right kidney cyst.
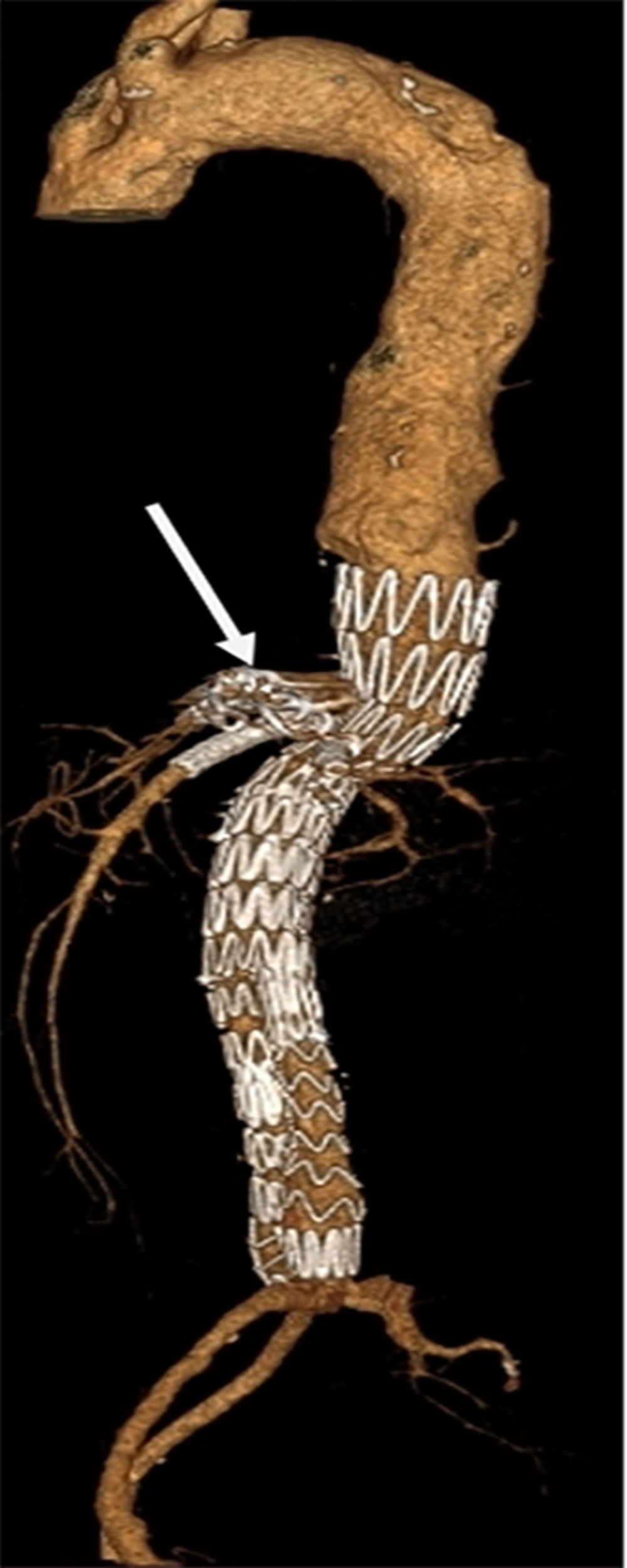
Due to the high surgical risk, we opted for an endovascular approach. We decided to exclude the aneurysm using a fenestrated endograft with three fenestrations (two for the renal arteries and one for the common trunk between the celiac trunk and the SMA). The procedure was performed under general anesthesia and entirely percutaneously. After initial aortography, we confirmed that collateral circulation between the CA and the SMA was well developed, and proceeded to occlude the CA using Amplatzers. We then deployed the endografts and fenestration stents, achieving a satisfactory final result on angiography (Figure 3).
Immediate outcomes were uncomplicated, with no incidents until the third day, when the patient became agitated and reported mild pain in the right hypochondriac region. There was no defensive tenderness, but a biological inflammatory syndrome with impaired liver function was observed.
An abdominal CT scan revealed small necrotic areas in the tail of the pancreas and the inferior lobe of the left kidney, as well as gallbladder necrosis. Due to the presence of a large kidney cyst, the patient underwent surgery via a subcostal approach to remove the gallbladder. The patient was admitted to the intensive care unit for one week and discharged after a total of two weeks.
At the one-month and three-month follow-up appointments, the patient showed good clinical progress and satisfactory scan results (Figure 3).
3. Discussion
Endovascular aortic aneurysm repair has continuously evolved over the last three decades and is now widely accepted as the treatment of choice for patients with suitable anatomy. Unfortunately, anatomical limitations may reduce the number of patients who can be effectively treated with EVAR. Almost 40% of patients are not eligible for standard EVAR due to unsuitable anatomy. Most of these limitations involve a hostile proximal aneurysm neck. Traditional aortic endografts require a 10 - 15mm infrarenal proximal neck for safe deployment. The neck is evaluated based on several factors, such as length, diameter, morphology, and character. These factors are crucial for adequate graft fixation and sealing and are essential for achieving both immediate and long-term durable EVAR results.
For patients with challenging proximal necks, such as in our case, several innovative techniques have been developed to extend the length of the proximal aortic seal, such as fenestrated endografts. This technique allows for proximal sealing zone expansion beyond the renal arteries and requires only a 4 mm proximal neck for deployment (2).
In our case, the proximal sealing zone extended beyond the renal arteries to include the celiac aorta. Additionally, we dealt with a common celieomesenteric trunk, which made fenestration of the common trunk and both branches challenging. To avoid endoleaks, we had to occlude the celiac trunk after assessing collateral circulation between both branches.
Studies with short-term outcomes have shown that CA’s coverage is an acceptable approach for treating patients with insufficient sealing zones when the collateral network between the CA and the SMA can be individualized (5). Multiple collateral pathways connect the SMA to the CA origin, such as pancreaticoduodenal arcades and dorsal pancreatic arteries. Branches of the gastroduodenal artery connect with the inferior pancreaticoduodenal arteries that originate from the SMA to create the anterior and posterior pancreaticoduodenal arcades. The dorsal pancreatic artery is commonly the first large pancreatic branch of the splenic artery that connects with the pancreaticoduodenal arcades (6).
Grabenwoger et al. (7) suggested in their study that abdominal ischemia and mortality in the postoperative period were essentially linked to partial coverage of the CA. Others have suggested that embolic events resulting from aortic manipulation and ballooning during graft deployment might contribute to ischemia (6). Complete coverage of the CA is preferred over partial coverage because partial coverage may increase the risk of embolic phenomena (5).
Regarding gallbladder necrosis following fenestrated endovascular aortic repair (FEVAR), particularly after CA coverage, there are two major theories. Pol et al. (8) and Ng et al. (4) reported that gallbladder necrosis after EVAR and FEVAR is associated with a right replaced hepatic artery (RRHA) originating from the SMA, which is the most common hepatic artery anatomical variation. A systematic review conducted by Shukla et al. (9) reported this variation in 11 to 21% of cases. The authors highlighted that significant mural thrombus in the SMA, as well as aortic and iliac artery calcification, could contribute to significant micro-embolic phenomena affecting organs supplied by the SMA.
Another plausible theory is that micro-embolic phenomena might have occurred during the occlusion of the CA using amplatzers.
5.1. Conclusions
Gallbladder necrosis is an extremely rare complication that may occur after FEVAR, especially with celiac trunk coverage. Although it may not be preventable, it should be suspected early when suggestive symptoms are present to ensure proper treatment.