1. Introduction
The aberrant right subclavian artery, clinically known as Arteria Lusoria, is the most common embryologic abnormality of the aortic arch (1). It was first described in 1735 by Hunauld (2). It is considered to be caused by an abnormality of the right fourth pharyngeal arch that is responsible for the development of the innominate artery and the persistence of the seventh intersegmental artery (3).
Symptomatology is essentially related to aneurysmal disease development that mostly occurs at the level of its origin. It occurs in 60% of aberrant right subclavian artery cases, known as the Kommerell diverticulum (4, 5).
The natural history of aberrant right subclavian artery aneurysms is similar to aneurysms in other locations, with continuous expansion and risk of rupture and death (6).
Open surgical repair of these aneurysms is usually performed under a thoracotomy and requires aortic clamping, which can be a source of increased morbi-mortality in high-risk patients. Endovascular repair of ARSA aneurysms has been reported and represents a less invasive approach (7, 8).
We present the case of endovascular repair of an aberrant right subclavian artery aneurysm.
2. Case Presentation
A 75-year-old female treated for COPD consulted a pneumologist for increasing dyspnea for several months. A CT scan showed a retro-esophageal aberrant right subclavian artery aneurysm, and the patient was transferred to our unit for further examination and eventual treatment. Physical examination was perfectly normal; there was no palpable cervical nor thoracic mass, and blood pressure was normal and symmetrical in both arms.
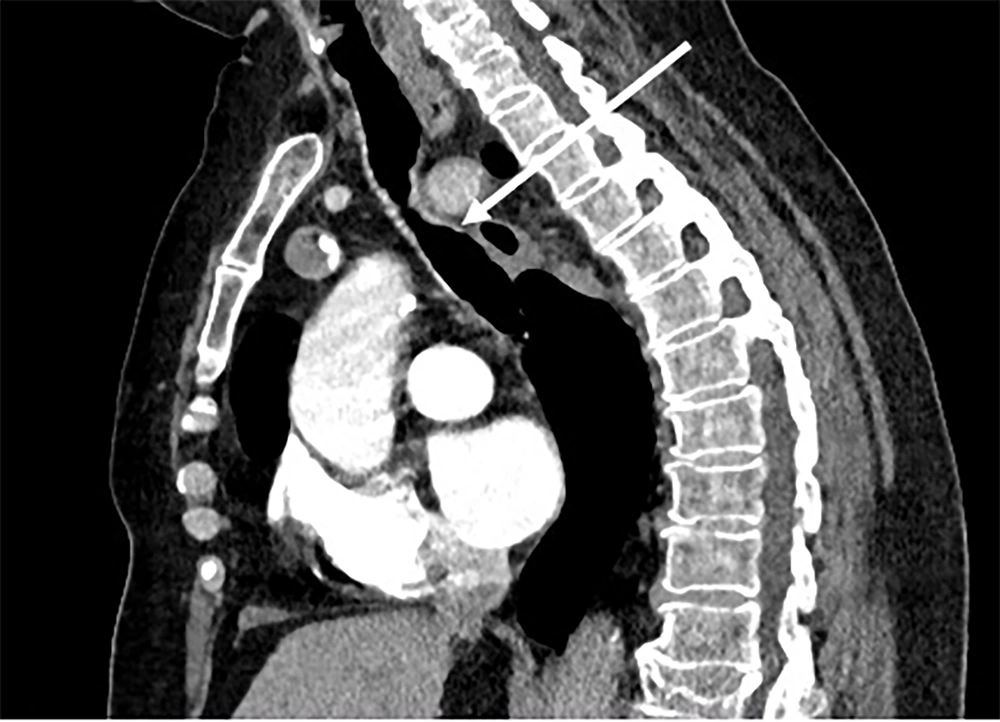
Dedicated CT angiography was made and showed that the ARSA arose a few centimeters after emerging from the aorta. It passed through the posterior mediastinum to attend to the right arm, slightly compressing the esophagus (Figure 1).
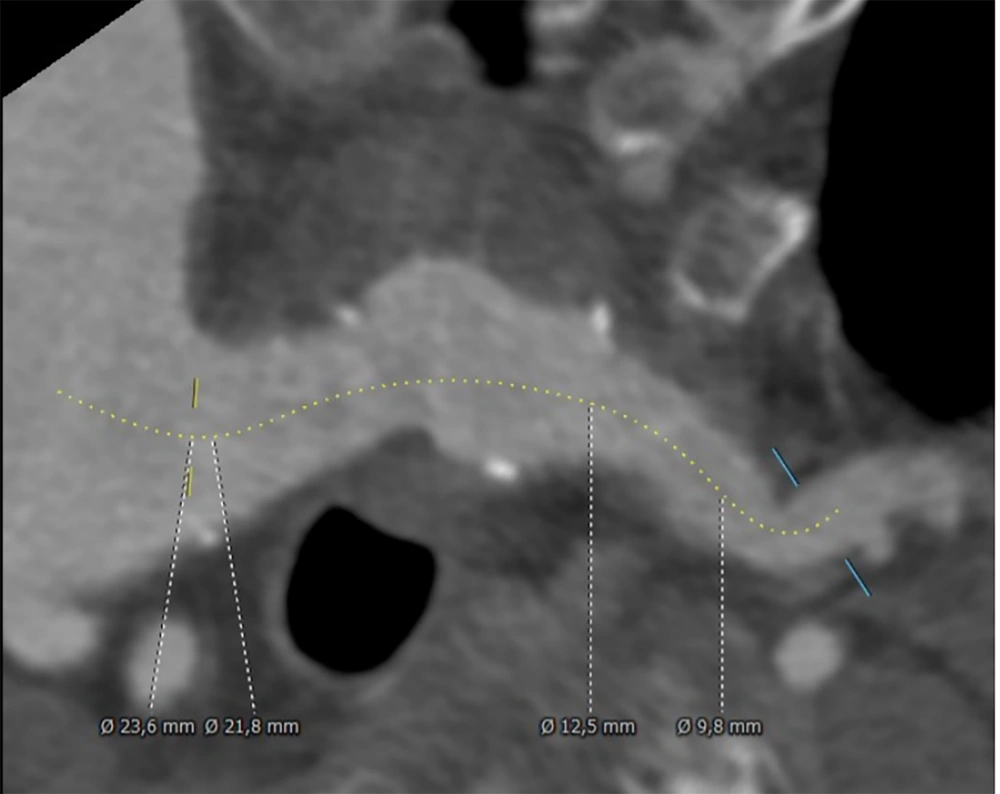
Vertebral and mammary arteries were issued from subclavian arteries and spared from aneurysm dilation. The maximum aneurysm diameter was 46 mm, the proximal neck diameter was 23.6 mm, and the distal neck diameter was 9.8 mm (Figure 2).
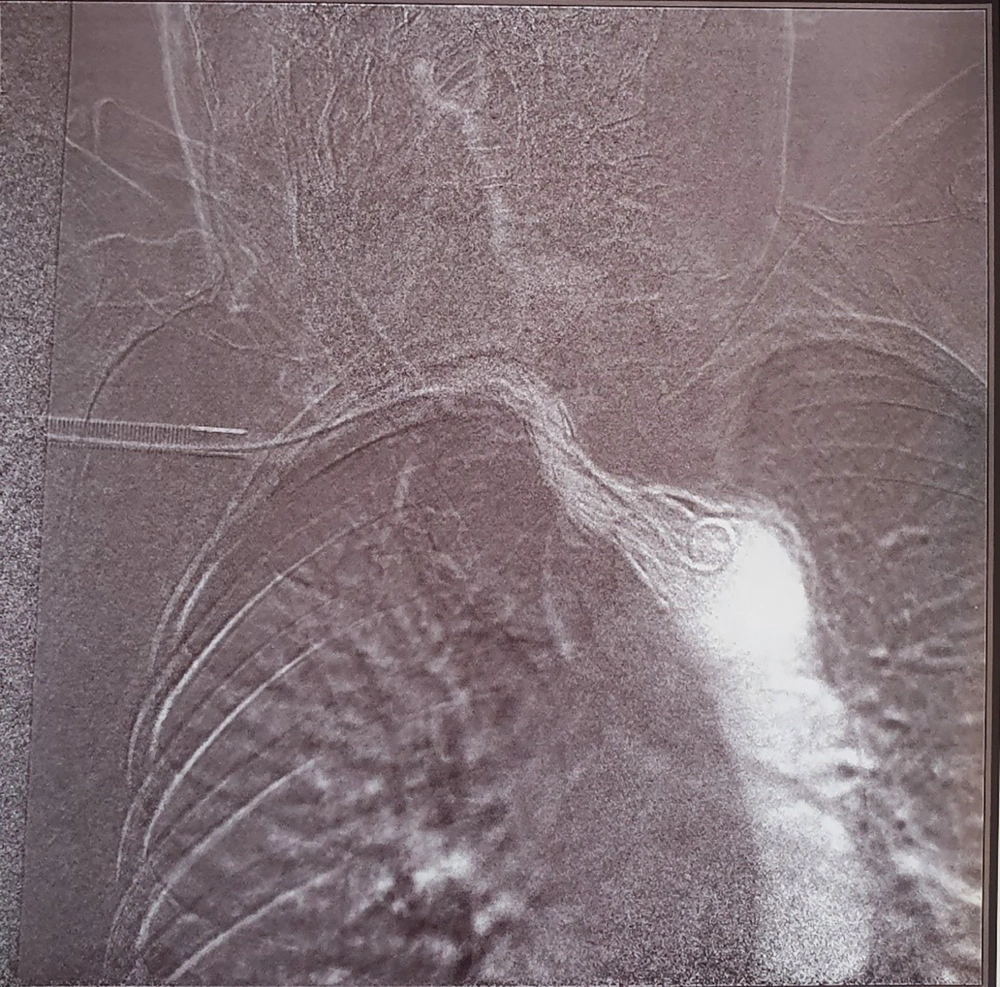
Even though no alarming symptoms concerning aneurysm size drove us to treat the patient using an endovascular approach, it was done after a deep discussion with the patient about the risks, benefits, and alternatives, such as open surgery. The procedure took place under local anesthesia with light sedation. The vascular access was provided by a 16 French sheath introduced after a surgical control of the axillary artery in the armpit. After catheterizing the aneurysm, we deployed a Cook degressive endograft 28 - 12/60 mm with good angiographic control at the end of the procedure (Figure 3).
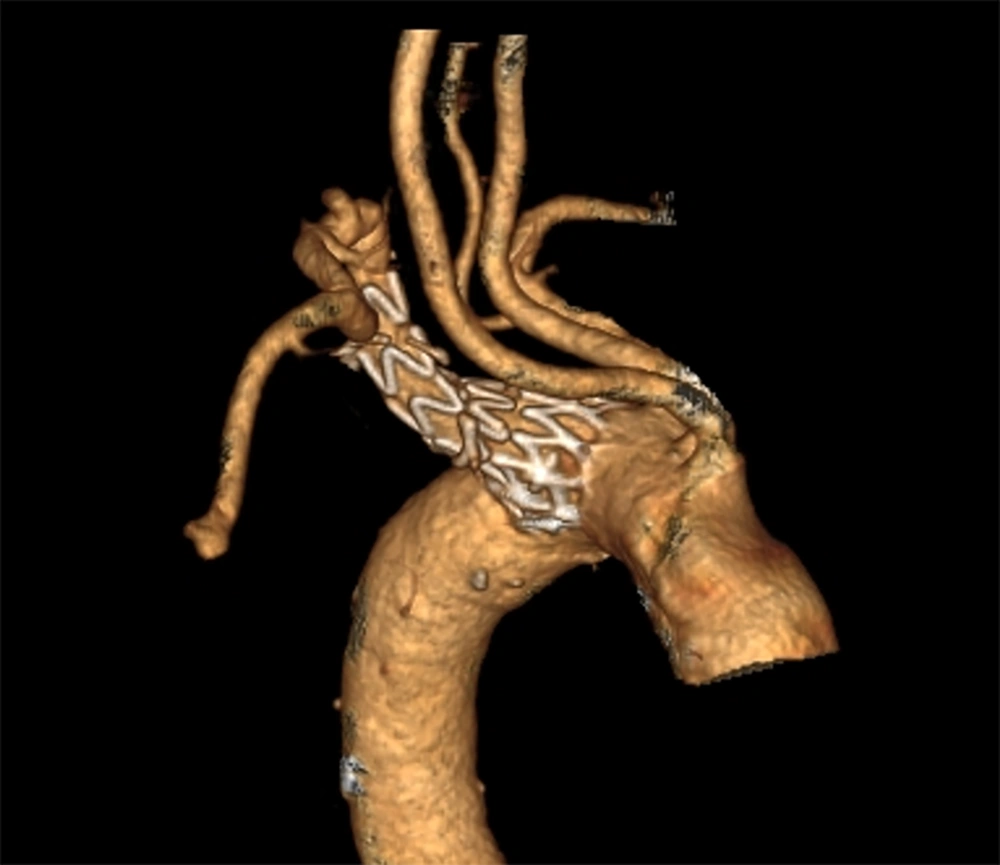
The patient was discharged on day 2 and was seen at 01 and 06 months with a satisfying CT angiography control at 01 months (Figure 4).
3. Discussion
An aberrant subclavian artery represents the most common anomaly of the aortic arch, with an
Incidence of around 1 to 2% (9). It is associated with a higher incidence of trisomy 21 (19 - 35%) and other congenital syndromes (10). In 60% of cases, it originates from a saccular dilation of the aorta, known as “Kommerell’s diverticulum” (11). Ninety percent of patients are asymptomatic, but compression of the esophagus or the trachea can cause symptoms like dysphagia (71%), dyspnea (19%), or coughing (8%) (12).
In 1956, 20 years after Kommerell’s first description of the vessel’s diverticulum, McCallen described an aneurysmal aberrant right subclavian artery (13). Ninety percent of these aneurysms are secondary to atherosclerosis, and 25% are associated with other locations of aneurysms, most frequently in the aorta (6).
Although the natural history of an aberrant right subclavian artery aneurysm is not precisely known because of its rarity, rupture and dissection have been reported. Austin and Wolfe, in their publication, reported a rupture rate of 19% among 32 patients (6). Cinà and his team observed a rupture or dissection rate of 53% among 32 patients with aberrant subclavian artery and right aortic arch (5).
The limit to considering whether the diverticulum at the vessel’s origin is normal or aneurysmal was not clear until 1989 when Felson established a classification containing three groups: The normal diverticulum, aneurysmal dilatation of the diverticulum, and aneurysm of the distal vessel separated from the diverticulum or aorta by a normal segment of the subclavian artery (14).
For aberrant subclavian artery aneurysm management, the threshold size above which aneurysm repair should be indicated in asymptomatic or mildly symptomatic patients is not precisely determined. Cinà et al. recommended surgical repair for 3 cm aneurysms or above (5). However, Ota and his team recommended treatment for symptomatic aneurysms of 5 cm or greater (15). Other series recommended early intervention (16, 17).
The gold standard treatment had been open surgery until endovascular and hybrid techniques emerged (18, 19). Nevertheless, surgical management for this pathology requires thoracotomy or sternotomy and even circulatory arrest in some cases, which is responsible for a high rate of mortality (18 - 25%) (6, 20).
Yang et al. in their study (21), compared surgical and endovascular techniques and found that in endovascular/ hybrid techniques groups, the mortality rate was (6.5%) and was significantly lower than reported by Kieffer et al. (18) (P = 0.043) and Austin and Wolfe (6) (P = 0.030), so was the complication rate (17.9%) compared to Austin and Wolfe (6) (P = 0.032) and Esposito et al. (20) (P = 0.001) and concluded that endovascular approach might be a good choice, especially for older patients with multiple comorbidities.
Davidian et al. (22) were the first to report an endovascular repair for an aberrant right subclavian artery aneurysm using a 24/13/110 mm PTFE-covered stent graft with a successful result; studies began then to emerge to report cases with hybrid techniques such as carotid-subclavian bypass associated with TEVAR and in some cases fenestrated fully percutaneous procedures (21, 23).
3.1. Conclusions
The presented case shows that aberrant right subclavian artery aneurysm repair with the appropriate anatomy can be successfully treated with an endovascular approach using a covered stent, which allows avoiding invasive surgery and subsequent high mortality and morbidity rates.