1. Introduction
Congenital malformation of mitral valve could encounter in isolation or with other congenital heart diseases. This would occur at any valvular level (1). Here, we report a case of congenital hypoplastic anterior mitral valve leaflet (AMVL).
2. Case Presentation
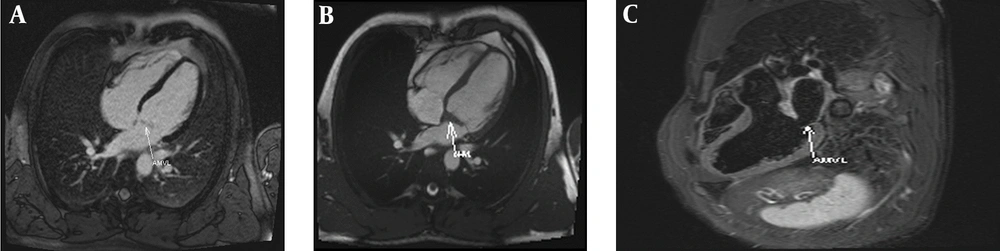
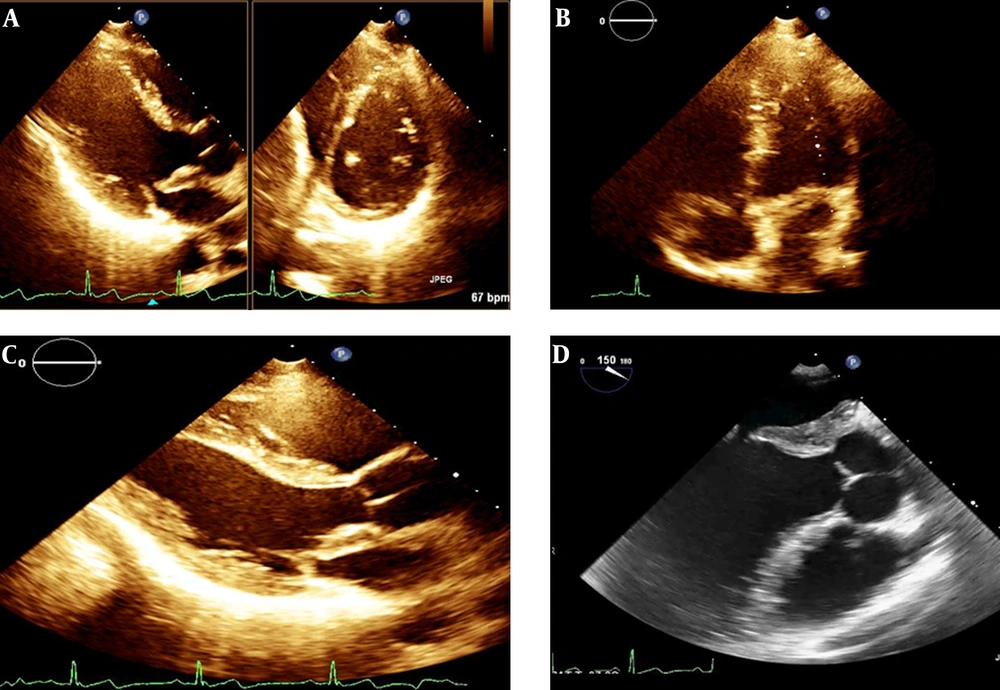
A 30-year-old male with past medical history of diabetes mellitus referred with pleuritic chest pain since a day before. He was admitted with impression of pericarditis. He was under treatment with insulin injection. He declared no previous complaints. Electrocardiography showed typical changes compatible with pericarditis. Lab data demonstrated leukocytosis with neutrophil predominance. Cardiac troponin was twice negative. Trans thoracic echocardiography (TTE) showed no pericardial effusion. By administration of non-steroid anti-inflammatory drug, the chest pain was subsided. Incidental finding in TTE was lipomatous change of mitral valve annulus and hypoplastic AMVL with mild to moderate mitral regurgitation which was confirmed by trans-esophageal echocardiography (Figure 1). Cardiac magnetic resonance imaging (CMR) showed thickening and fibrosis replacement of inter valvular fibrosa which extended to AMVL and resulted in restricted MV annulus (12.4 mm) with subsequent restricted MV opening without significant mitral stenosis or regurgitation (Figure 2). These data were in favor of congenital hypoplastic MV annulus. The patient is under close observation without any complaints.
A, Orthogonal trans thoracic echocardiography (TTE) view; B, apical 4 chamber TTE view; C, para sternal long axis TTE view ;and D, parasternal trans esophageal echocardiography view which demonstrates lipomatous change of mitral valve annulus and hypoplastic anterior mitral valve leaflet without significant stenosis. The arrow points to hypoplastic anterior mitral valve leaflet.
A, Late gadolinium enhancement cardiac magnetic resonance (CMR) imaging showed thickening and fibrosis replacement of intervalvular fibrosa which extended to anterior mitral valve leaflet; B, 4 chamber CMR image demonstrated restricted mitral valve annulus with subsequent restricted MV opening without significant mitral stenosis or regurgitation; C, 3 chamber STIR CMR image confirms these findings.
3. Discussion
Unileaflet mitral valve is the rarest kind of congenital mitral valve anomalies (2). This anomaly, which is mostly due to hypoplastic PMVL, is often fatal in infancy without any surgical intervention due to severe mitral regurgitation (2, 3). There are some adult case reports regarding unileaflet mitral valve due to hypoplasia of posterior mitral leaflet without severe MR who were identified just after auscultation of systolic murmur during check-up physical examination (4, 5).
Hypoplastic AMVL could be considered as a subtype of unileaflet mitral valve but there is lack of available reports compared with hypoplastic PMVL. Our case was an asymptomatic male with hypoplastic AMVL and restricted annulus. This is different from hypoplastic mitral annulus which is also a rare mitral valve anomaly in which the whole mitral valve appears hypoplastic and would be part of Shone complex (6). Theoretically, the same with hypoplastic PMVL, hypoplastic AMVL might be associated with severe MR, but our case was an adult case with lipomatous change of mitral valve annulus with hypoplastic AMVL without severe MR. To diagnose this congenital mitral anomaly, a combination of TTE and CMR are helpful. Periodic echocardiographic surveillance is recommended to detect worsening of MR severity in these cases but still there is no available guideline recommendations.
3.1. Conclusions
Hypoplastic AMVL with restricted mitral valve annulus is a rare cause of mitral valve malformation and could be well tolerated since adulthood with good prognosis.