1. Introduction
Classic fever of unknown origin (FUO) is defined as fever with a minimum measured temperature of 38.3ºC (101ºF) on several occasions, persisting without a diagnosis for at least three weeks without a definite diagnosis despite three days of hospitalization or three outpatient visits (1, 2).
Fever of unknown origin is a diagnostic problem, and about 30 - 50% of patients remained undiagnosed despite extensive workup (3, 4). The most important causes of classic FUO are infectious diseases, cancers, and non-infectious inflammatory diseases (2, 4, 5).
The most important cardiogenic causes of fever are myocardial infarction, pericarditis, endocarditis, and postcardiac injury, which should be given special attention when investigating the cause of FUO (6).
In this case, we evaluated a patient with a cardiogenic cause of FUO; despite all the studies, no definite cause was found for it, but it responded to empiric treatment.
2. Case Presentation
A 42-year-old man presented with intermittent fever, chills, loss of appetite, and fatigue for 2 years prior to admission. The patient underwent numerous examinations that did not reach a definitive diagnosis. During these two years, he was treated with empiric antibacterial drugs and corticosteroids occasionally but did not respond dramatically to the treatment.
Two years ago, the patient also had a mild COVID-19, which improved without obvious complication. He was a farmer, and there was no significant point in his past medical history. His social history was negative for smoking, intravenous (IV) drug use, high-risk sexual behavior, and recent travel to endemic areas. He had performed numerous tests and examinations for rheumatic and infectious diseases, none of which were in favor of diagnosing a particular disease.
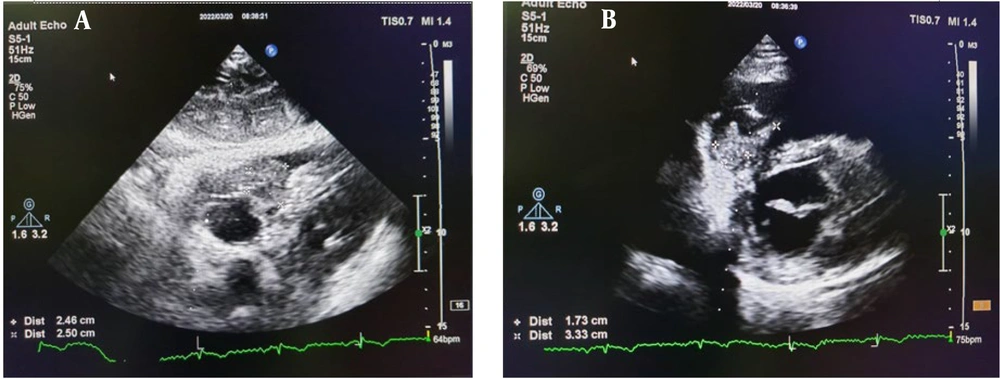
The patient had only hypochromic microcytic anemia (HB: 10 g/dL) and high C-reactive protein (CRP; 18 mg/L) in lab tests. Other laboratory findings were normal. According to the occasional findings observed in echocardiography, the patient was referred to our center for further evaluation and was admitted. Transthoracic echocardiography (TTE) showed normal LV size and function, normal RV size and function, no significant valvular heart disease, and TTE revealed an echo dense mass in RV (3.1 × 1.8 cm) that attached to the right ventricular side of the interventricular septum with a small semi mobile component (1 × 1 cm) that suggested thrombus (Figure 1).
The patient developed pleuretic chest pain during hospitalization. Spiral chest computed tomography (CT) scan showed peripheral pulmonary infarct, but pulmonary CT angiography showed no feeling defect in segmental, sub-segmental, and lobar vessels but confirmed peripheral pulmonary infarct. Infectious disease and oncology counseling were requested. None of the studies, including screening tests for malignancy, endoscopy, and colonoscopy, found evidence of malignancy.
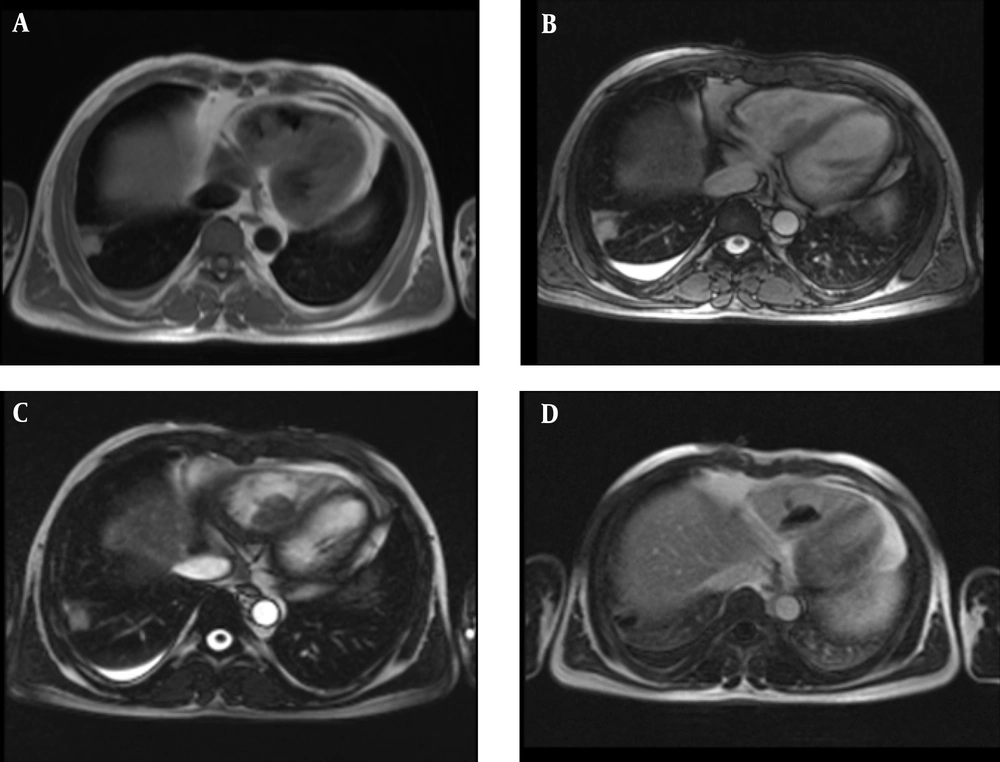
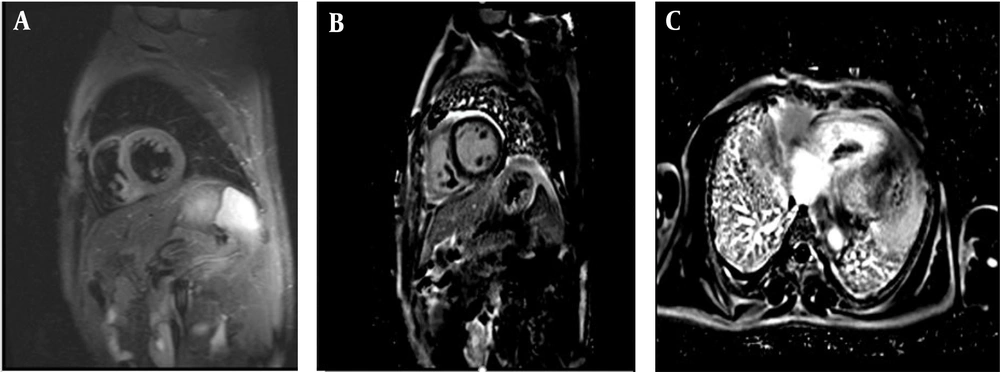
Multiple blood cultures, brucellosis antibodies, and COVID-19 polymerase chain reaction (PCR) were negative. Cardiac magnetic resonance imaging (MRI) was performed, and it showed a large lobulated heterogeneous mass with a size of 34 × 23 mm in the RV cavity attached to the septal wall and another 8 × 5 mm and 7 × 4 mm mobile masses attached to the surface of a large mass in favor of thrombus (Figures 2 and 3).
Therapeutic anticoagulants and broad-spectrum empiric antibiotics were started with the possibility of infected thrombosis in the patient.
Due to the lack of response to treatment after two weeks and the continuation of fever, and no change in cardiac mass, the patient underwent open cardiac surgery. The pathology result was fibrinous material with some RBC and severe PMN infiltration with abscess formation; no micro-organisms were seen. Culture obtained from tissue in the operating room was negative for fungus and bacteria. The patient's fever recurred after surgery. Infectious disease counseling was requested. Blood cultures for bacteria were negative again. A chest CT scan was done and showed no new change.
Abdominopelvic sonography and paranasal CT were normal. During the second episode of fever skin lesions, erythema nodosum appeared on distal upper and lower limbs. Before the biopsy of these lesions, they disappeared quickly. On echocardiography after surgery, a small residue of the mass was observed. Treatment with antibacterial and antithrombotic drugs was continued, and in addition to them, empiric antifungal therapy with caspofungin was added to the treatment according to infectious disease counseling. After starting antifungal treatment, the patient's fever stopped, and the patient's appetite and other symptoms improved. Finally, the patient was discharged in good general condition.
3. Discussion
The prognosis of patients with FUO who remain undiagnosed is not well known, but some studies reported a mortality of 2.4% in undiagnosed patients. Spontaneous resolution of FUO was reported in 43 to 75% of undiagnosed cases. Patients with undiagnosed FUO are usually empirically treated with antibiotics, corticosteroids, or other anti-inflammatory drugs. Our patient has been treated with various empiric drugs for two years, but the intermittent fevers recurred. The effects of these treatments are largely unknown. Efficacy of treatment of FUO patients in one study is 70.6% with empiric antibiotics, 84.6% with corticosteroids, 66.7% with immunosuppressive drugs, and 65.0% with nonsteroidal anti-inflammatory drugs (NSAIDs)/acetaminophen (3).
Persistent fever of unknown cause is rarely of cardiac origin, but heart disease must be considered in the differential diagnosis, and a thorough evaluation is performed. As our patient would have been diagnosed with endocarditis sooner if he had undergone echocardiography earlier (6).
The patient also reported a history of COVID-19 infection, but he was unaware of the medications received at the time of the disease. Due to the new nature of the disease and its many complications, it is not possible to make a definite statement as a predisposing factor for the patient (7).
Fungal endocarditis is a rare but fatal disease with a poor prognosis. Most patients have a predisposing factor such as immunodeficiency, prosthetic valve, or IV drug use, but rare cases develop fungal endocarditis without an underlying risk factor (8). Because this patient did not have a predisposing factor, his disease was diagnosed with delay, and we were less suspicious of fungal diseases.
Prolonged fever is usually the most common manifestation of fungal endocarditis. However, sometimes the onset of the disease is in the form of heart murmurs, chest pain, shortness of breath, weakness and lethargy, body aches, and skin lesions. Blood cultures are negative in many cases. Due to the challenging diagnosis of fungal endocarditis, it is usually diagnosed late, which worsens the prognosis.
Echocardiography is a good diagnostic tool for diagnosing cardiac masses, although it does not provide histopathology for definitive diagnosis. Large, bulky, and highly mobile masses are more suggestive of fungal vegetations than bacterial endocarditis. Fungal endocarditis also risks embolic events due to the large and mobile mass, and many cases require cardiac surgery. Differential diagnoses of heart mass in addition to fungal endocarditis can be benign or malignant primary cardiac tumors, cardiac metastasis, or thrombosis. Cardiac MRI is very helpful in diagnosing different types of cardiac masses (9-13).
Prompt diagnosis and immediate initiation of appropriate treatment for fungal endocarditis improve survival. Fungal endocarditis is more common than bacterial endocarditis can cause embolic phenomena, and the most common organs involved are the brain, kidneys, spleen, and lungs. Our patient had a pulmonary embolism event that resulted in a pulmonary infarction and caused pleuritic chest pain for the patient, which fortunately was not a major or fatal embolic event. In high-risk patients, including immunocompromised patients with prolonged fever who do not respond to antibacterial therapy, it is recommended to start empiric antifungal therapy with sufficient term and dose (14, 15).
3.1. Conclusions
Finally, in this patient, since we did not have a positive blood culture or a definite pathology result in favor of the fungus, we cannot definitively make a diagnosis of fungal endocarditis. However, considering that the patient did not respond to experimental antibacterial and antithrombotic therapies and symptomatic therapies, but the patient's symptoms disappeared with antifungal treatment, it seems reasonable to start experimental antifungal therapy in these cases.
Based on this case, it can be recommended that cardiac causes, including endocarditis, should be considered in cases of prolonged fever. In case of non-response to routine treatments, antifungal treatment should be considered even in patients without risk factors of fungal infection.