1. Background
SARS-CoV-2 is responsible for the current epidemic of COVID-19, which is causing catastrophic respiratory problems and multi-organ infections, as well as increased mortality. Infections or medicines prescribed to patients cause these impacts. Compared to those without any underlying disease, patients with underlying diseases have higher mortality rates. Patients suffering from cardiovascular disease (CVD) are at a higher risk of mortality from COVID-19 due to their fragility and susceptibility to myocardial infections (1-3).
In 2020, Clerkin et al. confirmed that most deaths were caused by CVD. Infection by coronavirus can cause myocarditis or trigger an inflammatory response (4). Electrocardiogram (ECG) and echocardiography may also be altered by direct infection of the myocardium. Mehra et al. confirmed that coronary artery disease (CAD) may also increase the risk of inpatient mortality in 2020 (5). Another study showed that cardiac comorbidities, CAD, and chronic obstructive pulmonary disease (COPD) are positively related to hospital reported mortality (6). A person's age or cancer status do not significantly affect it. In 2020, Loffi et al. reported an excessively higher mortality rate in patients with COVID-19 and CAD, which was associated with comorbidities rather than CAD's immediate effects (7). In 2020, Aggarwal et al. did not find a strong association between prior cardiovascular disorder and mortality in intense COVID-19 ailment (odds ratio [OR] = 1.72; 95% CI: 0.97 - 3.06, I2 = 0 %, P = 0.46) (8). Pre-existing CVD in COVID-19 sufferers is associated with worse outcomes. When implementing chance stratification models, clinicians and policymakers should consider these findings. In 2021, Amini et al. concluded that CVD incidence and mortality rates were declining, while CVD survival rates were stable (9). In general, these results show that global efforts have been successful in controlling CVD burdens. Yet, more efforts are needed to improve survival rates and lower the burden of this disease. A rising trend in either incidence or mortality is especially evident in some areas. Petermann et al found that eating fish rather than meat or poultry was correlated with lower cardiovascular risks in 2021 (10). In addition, vegetarianism was only associated with a lower CVD incidence risk. Gao et al. identified dietary patterns associated with CVD and all-cause mortality in 2021 (11). It will provide evidence for underpinning food-based dietary advice to reduce health risks by identifying specific foods and beverages that contribute to unhealthy dietary patterns.
Across a range of CVDs, Cannata et al. examined the excess in-hospital mortality unrelated to COVID-19 infection. In-hospital mortality among patients with CVDs was higher than outside the pandemic, independent of COVID-19 co-infection (12). Studies with the largest declines in admission rates showed a sicker cohort of patients. To establish the full extent of mortality not directly related to COVID-19 infection, further well-designed studies are needed. According to Jovani et al, several significant associations have been observed between circulating biomarkers of CVD and cancer (13). This supports the hypothesis that both diseases are caused by similar biological pathways. Further investigations of specific mechanisms leading to both CVD and cancer are warranted. In 2022, Chieng et al. concluded that 2-3 cups/day of decaffeinated, ground, and instant coffee were associated with significant reductions in CVD and mortality (14). Additionally, decaffeinated coffee was associated with reduced arrhythmia, but not ground or instant. Xi et al found that short-term ambient PM2.5 exposure was positively correlated with CVD events and mortality among hemodialysis patients (15). Older hemodialysis patients appeared to be more susceptible to PM2.5-related CVD events.
In 2022, Tian et al. found that early TyG index accumulation significantly increased CVD and all-cause mortality rates, emphasizing the importance of controlling TyG index early in life (16). Giosue et al. attempted to synthesize knowledge regarding the links between fatty fish intake and cardiovascular events and all-cause mortality in 2022 (17). There was an inverse association between fatty fish and CHD incidence (0.92; 95% CI: 0.86, 0.97), CHD mortality (0.83; 95% CI: 0.70, 0.98), and total mortality (0.97; 95% CI: 0.94, 0.99). Unlike lean fish only, both fatty fish and lean fish consumption did not show significant associations with CVD incidence and mortality. Fish consumption benefits are, in fact, driven by fatty fish, according to the study findings. Hernandez-Hernandez et al. examined the association between preexisting CVD and COVID-19 mortality in hospitalized Latin Americans in 2022 (18). Mortality in hospital was the main outcome. The adjusted OR with 95% CI was calculated using multivariable regression analyses. A total of 28,929 (35.54%) hospitalized patients with SARS-CoV-2 infection were evaluated. Women made up 35.41% (10,243). Men died more in hospitals than women. Compared to men, women had a higher CVD incidence (4.69% vs 3.93%, P = 0.0023). As a result of the adjusted logistic regression analysis, women were significantly more likely to die from COVID-19 than men.
Patel et al. reported pathogenic variants associated with inherited cardiomyopathy in 2022 (19). A pathogenic variant associated with inherited cardiomyopathy was found in approximately 0.7% of participants. Clinically, variant carriers are difficult to identify without genetic testing, but they are at increased cardiovascular and all-cause mortality risk. The association between folate intake and CVD-mortality and all-cause mortality was examined by Xu et al. in 2022 (20). US adults at high risk for CVD may suffer adverse effects from excessive folic acid supplementation, according to the study. In 2022, Yerramalla et al. investigated associations between total duration and pattern of accumulation of objectively measured sedentary behavior (SB) with incident CVD and all-cause mortality (21). Once MVPA was taken into account, the study found no association between overall sedentary time and sedentary accumulation patterns and CVD and all-cause mortality. To support the recent recommendations to reduce and fragment SB, our findings of decreased mortality risk with less total and more fragmented SB should be replicated. According to Alizadehsani et al.'s findings in 2022, fever, cough, diarrhea, chest pain, nausea, chills, abdominal pain, vomiting, myalgia, and anorexia had no impact on mortality (22). The mortality rate of COVID-19 cardiovascular patients was significantly correlated with symptoms such as headache, loss of consciousness, oxygen saturation less than 93%, and the need for mechanical ventilation.
In summary, these research studies have demonstrated that CAD can increase the risk of mortality and the need for renal substitution therapy. This is due to the burden of comorbidities rather than to an instantaneous effect of CAD.
2. Objectives
In this article, we are attempting to investigate whether or not cardiac-related ailments cause an increased risk of mortality.
3. Methods
3.1. Study Population
During the course of the present study, all consecutive patients at Shariati hospital, a large tertiary center in Iran, were recruited retrospectively. In order to obtain demographic and clinical information from the medical records, a review was conducted. Shariati hospital's ethical committee has approved the study and has given its approval to the study.
3.2. Demographic and Clinical Features
In the present study, patients with a history of CVD, hypertension, diabetes mellitus, dyslipidemia, hypothyroidism, chronic kidney disease, and a positive chest computed tomography (CT) scan compatible with coronavirus, who were administered in the intensive care unit under mechanical support, were included. It is critical to note that all the risk factors have been examined in this study in order to find out if they have any effect on mortality.
3.3. Statistical Analysis
We used the software package SPSS 24 (SPSS Inc, Chicago, IL) for data analysis and statistical calculations in this study as part of the software package SPSS 24. By applying the Kolmogorov-Smirnov Z-test, we assessed the normal distribution of numerical variables. Frequency and percentage are methods to express categorical variables. Continuous variables are presented as mean x standard deviation. Results were reported using a univariate adjusted analysis. A P-value below 0.05 was considered statistically significant.
4. Results
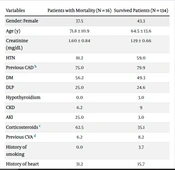
The data from 150 selected patients were included in this study. Table 1 provides demographic information.
| Variables | Patients with Mortality (N = 16) | Survived Patients (N = 134) |
|---|---|---|
| Gender: Female | 37.5 | 43.3 |
| Age (y) | 71.8 ± 10.9 | 64.5 ± 13.6 |
| Creatinine (mg/dL) | 1.60 ± 0.84 | 1.19 ± 0.66 |
| HTN | 81.2 | 59.0 |
| Previous CAD b | 75.0 | 79.9 |
| DM | 56.2 | 49.3 |
| DLP | 25.0 | 24.6 |
| Hypothyroidism | 0.0 | 3.0 |
| CKD | 6.2 | 9 |
| AKI | 25.0 | 3.0 |
| Corticosteroids c | 62.5 | 35.1 |
| Previous CVA d | 6.2 | 8.2 |
| History of smoking | 0.0 | 3.7 |
| History of heart failure | 31.2 | 15.7 |
| Dialysis e | 7.1 | 0.8 |
| COPD | 6.2 | 1.5 |
| Complications of MI | 18.8 | 3.7 |
Abbreviations: HTN, hypertension; CAD, coronary artery disease; DM, diabetes mellitus; DLP, dyslipidemia; CKD, chronic kidney disease; AKI, acute kidney injury; CVA, cerebrovascular disease; COPD, chronic obstructive pulmonary disease.
a Values are expressed as percentage unless otherwise indicated or mean ± SD.
b CAD: Previous PCI, CABG, MI.
c History of use of corticosteroids.
d Cerebrovascular disease and transient ischemic attack.
e Need of dialysis during admission.
Patients were 43% female and 57% male, with an average age of 65 ± 13.5 years. Those who died had a mean creatinine level of 1.60 ± 0.84 mg/dL compared with those who didn't. Hypertension was the most common risk factor (60.9%). There were 16 deaths out of 150 patients, or 10.6%. Acute kidney injury during admission (P = 0.005), previous use of corticosteroids (P = 0.016), and dialysis (P = 0.052) all had significant effects on mortality. As shown in Table 2, there was a significant difference in creatinine levels between the two groups (P = 0.044).
| Variables | Patients with Mortality (N = 16) | Survived Patients (N = 134) | P-Value |
|---|---|---|---|
| Creatinine (mg/dL) | 1.60 ± 0.84 | 1.19 ± 0.66 | 0.044 |
| AKI | 25.0 | 3.0 | < 0.005 |
| Corticosteroids | 62.5 | 35.1 | 0.016 |
| Dialysis | 7.1 | 0.8 | 0.052 |
| Complications of MI | 18.8 | 3.7 | 0.012 |
a Values are expressed as percentage unless otherwise indicated or mean ± SD.
Mortality was not affected by other factors. In addition, CAD and other cardiac diseases and risk factors were associated with an increased risk of mortality. Rather than being directly correlated with each comorbidity, it is largely attributable to the burden of comorbidities.
5. Discussion
A key issue in 2020 is coronavirus pandemic, which causes catastrophic respiratory and multi-organ problems. It may be the virus itself or the drugs used to treat the patients that cause these effects. Mortality rates were significantly higher in patients with underlying diseases. Cardiovascular patients are particularly vulnerable to COVID-19 mortality due to their frailty and susceptibility to myocardial involvement (1-3). According to Fei Zhou et al in April 2020, coronary heart disease is associated with acute cardiac events and poor outcomes in influenza and respiratory viral infections (23, 24). More than half of those who died had increased high-sensitivity cardiac troponin I during hospitalization.
In another study in 2020, Ganatra et al. concluded that patients with pre-existing cardiovascular risk factors and CVD are among those most vulnerable with potentially increased risk of acquiring SARS-CoV-2 infection, developing cardiovascular complications related to COVID-19, and having adverse outcomes (25). Clerkin et al. showed in 2020 that most deaths occur in patients with CVD (4). Coronavirus can directly infect myocardium or cause an auto-inflammatory reaction, causing myocarditis. Direct infection of myocardium may lead to a rise in cardiac troponin and changes in ECG and echocardiography. In a study published in 2020, Mehra et al. showed that a previous history of CAD may lead to a higher rate of inpatient mortality (5). In the other study, Shmushkevich et al. showed that hospital mortality was significantly and positively correlated with cardiac comorbidities, CAD, and COPD (6). However, it was not being significantly associated with patient age or cancer. In a study in 2021, Peterson et al discovered that patients with CAD and COVID-19 had more comorbidities, need for renal replacement therapy and inpatient mortality compared to their non-CAD counterparts (24, 26). However, after adjusting for other covariates, CAD itself was not associated with mortality. This suggests that other factors may play a larger role in the increased mortality and poor outcomes in these patients.
A study published in 2020 by Loffi et al. showed that patients with COVID-19 and CAD had high risk of mortality, which they believe is primarily due to the comorbidities, rather than a direct effect of CAD itself (7). According to Aggarval et al. in 2020, there was no significant association between previous history of CVD and mortality in severe COVID-19 disease (OR = 1.72; 95% CI: 0.97 - 3.06, I2 = 0%, P = 0.46) (8). The presence of pre-existing CVDs is associated with poorer outcomes among patients with COVID-19. The findings from this study need to be taken into account when implementing risk stratification models by clinicians and policymakers. In these studies, CAD was found to increase the risk of mortality and renal replacement therapy mainly due to comorbidities. This is more than a direct effect of CAD itself. The most common risk factor in our study was hypertension (60.9% of the patients). There was a mortality rate of 10.6% (16 of 150 patients) in the study. One of these factors was the occurrence of acute kidney injury during admission (P = 0.005), previous use of corticosteroids (P = 0.016) had a significant effect on mortality, while the need for dialysis (P = 0.052) did not have a significant effect on mortality. In Table 2, it was shown that there was a significant difference between the two groups in terms of the mean concentration of creatinine (P = 0.044). Other factors did not have a major impact on mortality in terms of the other factors.
5.1. Conclusions
It can be concluded from the results of our study that CAD, other cardiac diseases, and other risk factors may cause an increased risk of mortality and an increase in the need for renal replacement therapy. There is a connection between this and the burden of comorbidities rather than each of them having a direct effect on the outcome on its own.