1. Context
Cardiovascular diseases (CVDs) encompass a range of conditions, including hypertension, coronary artery disease (CAD), arrhythmias, heart failure, valvular abnormalities, and congenital heart defects (1, 2). With advances in medical therapies, many patients with CVDs now live longer, necessitating comprehensive management during dental treatments (3).
Dental procedures can pose risks for these patients due to systemic interactions, such as stress-induced cardiovascular events or bleeding complications from anticoagulant therapy (4). Consequently, a thorough understanding of cardiovascular conditions, associated medications, and procedural modifications is vital for safe dental care (5, 6).
This review focuses on the critical considerations that dentists must take into account when treating patients with cardiovascular conditions. By providing an evidence-based framework, it aims to guide clinicians in delivering safe and effective care while minimizing risks associated with these prevalent and complex diseases.
2. Evidence Acquisition
The evidence was gathered from clinical guidelines, such as those provided by the American Heart Association (AHA), and peer-reviewed studies focusing on the interplay between cardiovascular health and dental procedures. The review addressed key aspects such as antibiotic prophylaxis, anticoagulation management, stress reduction, and emergency preparedness. Articles from reputable medical and dental journals were included, and the latest advancements in care strategies were emphasized.
3. Results
Effective dental care for patients with cardiovascular conditions requires careful attention to the specifics of each disease and the patient’s medical history. The following are key considerations for managing these patients in the dental office:
3.1. Antibiotic Prophylaxis
To prevent infective endocarditis (IE), antibiotic prophylaxis is often recommended for patients at high risk, including those with prosthetic heart valves, previous episodes of IE, or specific congenital heart defects. The AHA provides guidelines on prophylaxis, with amoxicillin being the first-line antibiotic. For patients with penicillin allergies, alternatives such as clindamycin or azithromycin are recommended. Timing is crucial for prophylaxis, with antibiotics typically administered one hour before invasive dental procedures. While minor dental procedures may not require prophylaxis, invasive procedures, such as extractions, root canal treatments, and periodontal surgeries, necessitate adherence to these guidelines to prevent bacteremia and subsequent endocarditis (4).
3.2. Management of Bleeding Risks
Patients on anticoagulant therapy, including warfarin, direct oral anticoagulants (DOACs), and antiplatelet agents, present a particular challenge due to the increased risk of bleeding. Dentists must carefully assess the need to modify anticoagulant regimens based on the invasiveness of the planned procedure. For minor procedures, such as routine cleanings or restorations, patients may continue their anticoagulants without modification. However, for more complex surgeries (e.g., extractions or periodontal surgery), collaboration with the patient’s cardiologist is essential to determine whether to temporarily adjust or pause anticoagulant therapy. Local hemostatic measures, such as sutures, tranexamic acid mouthwashes, or hemostatic sponges, are invaluable tools to manage bleeding during and after dental procedures. It is important to note that switching anticoagulants or altering dosages should only be done with physician consultation to avoid thromboembolic events (7, 8).
3.3. Local Anesthetics and Drug Interactions
The use of local anesthetics containing vasoconstrictors, such as epinephrine, must be carefully considered in patients with cardiovascular conditions like arrhythmias, poorly controlled hypertension, and those with pacemakers or defibrillators. In these cases, it is prudent to either limit the amount of vasoconstrictor used or opt for epinephrine-free local anesthetics to avoid cardiovascular complications. Additionally, the interaction between NSAIDs and cardiovascular medications, such as aspirin and certain antihypertensive drugs, should guide postoperative pain management. NSAIDs can exacerbate hypertension and interact negatively with anticoagulant therapy, so acetaminophen or opioids may be preferable for postoperative pain relief. Dentists should also be aware of other medications the patient is taking (e.g., beta-blockers, diuretics), as these can influence the choice of local anesthetic and sedative agents (9, 10).
3.4. Stress and Anxiety Management
Stress during dental procedures can significantly affect cardiovascular function, elevating blood pressure, heart rate, and triggering arrhythmias in vulnerable patients. Dentists must adopt strategies to reduce patient anxiety and manage stress. This can include scheduling shorter, less invasive appointments and providing a calm, reassuring environment. Sedation options, such as nitrous oxide (often used for mild sedation) or oral anxiolytics, can be considered for more anxious patients, but care must be taken to monitor respiratory and cardiovascular function throughout the procedure. In cases of extreme anxiety or fear, general anesthesia may be an option, though this requires careful preoperative planning and consultation with the patient’s cardiologist. The use of non-invasive stress-reduction techniques, such as deep breathing exercises or guided relaxation, should also be incorporated into practice (11, 12).
3.5. Emergency Preparedness
Cardiovascular patients are at an elevated risk for emergencies during dental procedures, including angina, arrhythmias, or even cardiac arrest. It is essential that dental practices are well-equipped to handle such emergencies. Key equipment, such as an automated external defibrillator (AED), oxygen delivery systems, and emergency medications, should be available in all dental offices. Staff must be trained in basic life support (BLS) and advanced cardiac life support (ACLS), especially in practices with a high volume of patients with known cardiovascular conditions. Preparation includes developing emergency protocols that cover common cardiovascular events, ensuring that all staff members understand their roles in case of an emergency, and regularly reviewing these protocols through drills and training (13).
4. Conclusions
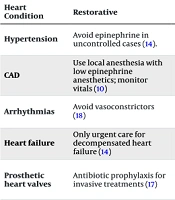
The dental management of patients with cardiovascular conditions requires meticulous planning, adherence to evolving guidelines, and interdisciplinary collaboration. By considering patient-specific risks, optimizing stress management strategies, and preparing for emergencies, dentists can ensure safe and effective care. This proactive approach not only minimizes complications but also contributes to improving overall patient health and quality of life (Table 1).
| Heart Condition | Restorative | Endodontics | Orthodontics | Periodontics | Pediatrics | Extraction/Surgery |
|---|---|---|---|---|---|---|
| Hypertension | Avoid epinephrine in uncontrolled cases (14). | Minimize stress; reduce vasoconstrictors (15) | Delay if poorly controlled (14) | Avoid invasive procedures if blood pressure > 180/110 (14) | Monitor sedation; stress-free environment (16) | Delay for uncontrolled hypertension; monitor blood pressure (11) |
| CAD | Use local anesthesia with low epinephrine anesthetics; monitor vitals (10) | Avoid stress and excessive bleeding (15) | Proceed in stable CAD; avoid excessive forces (16) | Prophylaxis for invasive procedures (17) | Short appointments with minimal stress (16) | Avoid procedures during active CAD; ensure stress-free environment (11) |
| Arrhythmias | Avoid vasoconstrictors (18) | Avoid electrical equipment (15) | Evaluate devices for pacemaker safety (15) | Avoid bacteremia-inducing treatments (12) | Non-invasive treatments preferred (16) | Use non-epinephrine anesthetics; shield pacemakers from interference (11) |
| Heart failure | Only urgent care for decompensated heart failure (14) | Avoid supine positions for extended periods (13) | Postponed until heart failure is stabilized (16) | Monitor oxygen saturation during scaling (18) | Consult pediatric cardiologist (16) | Defer non-essential surgeries in decompensated heart failure; manage oxygen (11) |
| Prosthetic heart valves | Antibiotic prophylaxis for invasive treatments (17) | Prophylaxis for risk of bacteremia (15) | Generally safe; consider prophylaxis (10) | Aggressive plaque control; scaling and root planning with prophylaxis (13) | Prophylaxis for invasive treatments (16) | Adhere to prophylaxis guidelines; ensure hemostasis (11). |
| Congenital heart defects | Tailored care; antibiotic prophylaxis (17) | Avoid bacteremia-inducing procedures (18) | Monitor systemic risks; low-risk cases (10) | Emphasize oral hygiene education (16) | Collaboration with pediatric cardiologist (16) | Prophylaxis may be necessary; assess stabilization needs (11) |
| IE | Strict adherence to prophylaxis guidelines (17) | Antimicrobial rinse before procedures (15) | Consult cardiologist for gingival health (10) | Prophylaxis for all surgical treatments (13) | Focus on preventive care (16) | Prophylaxis and preoperative stabilization (11) |
Abbreviation: CAD, coronary artery disease; IE, infective endocarditis.