1. Background
The term "athlete's heart" refers to the structural, functional, and electrical adaptations of the heart that occur as a result of regular sports training (1)
High-level exercise is associated with morphological changes, including an increase in the size of the left ventricle, thickness of the interventricular septum, and overall chamber volume (2).
Endurance-trained athletes often experience enlargement of the left ventricle (LV) and increased wall thickness, known as eccentric left ventricle hypertrophy. In contrast, resistance-trained athletes typically show increased wall thickness without changes in LV chamber size, referred to as concentric left ventricle hypertrophy (3, 4).
Floorball is a team sport with two teams of six players each. The goal is to score by hitting the ball into the opposing team's net using a stick. The game consists of three 20-minute periods, with a 10-minute break between each (5).
This sport is similar to hockey and falls under mixed endurance and resistance sports. In previous studies, athletes in this sport have demonstrated an increased LV dimension without a corresponding increase in the thickness of their ventricular walls. Additionally, there has been an observed increase in both end-diastolic and systolic volumes of the left ventricle in these athletes (5, 6).
2. Objectives
Despite the considerable research conducted in floorball, no studies have yet examined the structures and functions of the hearts of professional athletes in this sport. However, most of the exercises performed by athletes, such as floorball, are a combination of endurance and resistance exercises, and the echocardiographic characteristics of these athletes are less known.
3. Methods
Twenty athletes from the national floorball team, each with over five years of experience, participated in our research, approved by the ethics committee (IR.RHC.REC.1402.077). Eligibility criteria included: (1) No specific diseases, (2) at least 180 minutes of professional floorball per week for five years, with no involvement in other sports, (3) no injuries requiring absence from sports in the last six months.
First, participants provided written consent to join the study. They filled out a questionnaire covering personal and sports characteristics, health status, and weekly training hours. In this single-session study, participants' height and weight were measured to calculate body surface area (BSA), and trans-thoracic echocardiography was performed by a specialist on the same day. Body surface area was calculated using the Mosteller formula.
The echocardiogram device measured the diameter and volume of the heart chambers and Doppler variables. We used the affinity 70 ultrasound machine (version 7C, release 1.8.6) from Philips medical systems with a 3.5 MHz probe. Left atrial (LA) and right ventricle (RV) strain were assessed offline using TOMTEC software, while LV global and circumferential strains were measured by the device. A fellowship-trained cardiologist reviewed all stored images.
Statistical analysis was carried out using IBM SPSS Statistics 24. Quantitative data are presented as mean ± standard deviation, and qualitative data as percentages.
4. Results
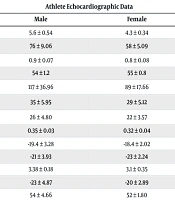
In our study of professional athletes, the average left ventricle end-diastolic diameter (LVEDD) was 5.6 ± 0.54 cm for males and 4.3 ± 0.34 cm for females, both lower than in previous studies. The left ventricle end-diastolic volume indexed to BSA (LVEDVI) averaged 76 ± 9.06 mL in men and 58 ± 5.09 mL in women.
The inter-ventricular septum thickness (IVS) averaged 0.9 ± 0.07 cm in male athletes and 0.8 ± 0.08 cm in female athletes. The left ventricular ejection fraction (LVEF) was 54 ± 1.2% for men and 55 ± 0.8% for women. Left ventricular mass indexed by BSA averaged 117 ± 36.96 g/m2 for men and 89 ± 17.66 g/m2 for women.
For atrial volumes, male athletes had a Left Atrial Volume Index (LAVI) of 35 ± 5.95 cc/m2 and a right Right Atrial Volume Index (RAVI) of 26 ± 4.80 cc/m2, while female athletes had LAVI = 29 ± 5.12 cc/m2 and RAVI = 22 ± 3.57 cc/m2. Relative wall thickness (RWT) averaged 0.35 ± 0.03 for males and 0.32 ± 0.04 for females
In professional athletes, the average global longitudinal strain (GLS) was -19.4% ± 3.28 in men and -18.4% ± 2.02 in women, while the global circumferential strain (GCS) was -21% ± 3.93 in men and -23% ± 2.24 in women.
The average diameter of the RV is 3.38 ± 0.18 cm in men and 3.1 ± 0.35 cm in women. In terms of RV function, RV strain is -23 ± 4.87in male athletes and -20% ± 2.89 in female athletes.
The average LA strain in different phases is as follows:
- In the reservoir phase, it is 54% ± 4.66 in men and 52% ± 1.80 in women;
- In the contractile phase, the strain is -14% ± 2.32 in men and -13% ± 1.44 in women;
- For the conduit phase, the average strain is -38% ± 1.11 in men and -36% ± 1.62 in women (Table 1).
| Variables | Athlete Echocardiographic Data | |
|---|---|---|
| Male | Female | |
| Left ventricle end-diastolic diameter (cm) | 5.6 ± 0.54 | 4.3 ± 0.34 |
| Left Ventricle end-diastolic volume (cc/m2) | 76 ± 9.06 | 58 ± 5.09 |
| IVS (cm) | 0.9 ± 0.07 | 0.8 ± 0.08 |
| Left Ventricle Ejection Fraction (%) | 54 ± 1.2 | 55 ± 0.8 |
| Left ventricular mass (g/m2) | 117 ± 36.96 | 89 ± 17.66 |
| LA Volume (cc/m2) | 35 ± 5.95 | 29 ± 5.12 |
| Right Atrium Volume (cc/m2) | 26 ± 4.80 | 22 ± 3.57 |
| RWT (cm) | 0.35 ± 0.03 | 0.32 ± 0.04 |
| GLS (%) | -19.4 ± 3.28 | -18.4 ± 2.02 |
| GCS (%) | -21 ± 3.93 | -23 ± 2.24 |
| RV diameter (cm) | 3.38 ± 0.18 | 3.1 ± 0.35 |
| RV strain (%) | -23 ± 4.87 | -20 ± 2.89 |
| LA reservoir phase strain (%) | 54 ± 4.66 | 52 ± 1.80 |
| LA contractile phase strain (%) | -14 ± 2.32 | -13 ± 1.44 |
| LA conduit phase strain (%) | -38 ± 1.11 | -36 ± 1.62 |
Echocardiographic Variable Results in Floorball Players
5. Discussion
Existing sports are classified based on two hemodynamic mechanisms: Isotonic and isometric (7). Currently, the modern athlete is a combination of resistance and endurance physiology, which is a combination of isotonic and isometric movement and for this reason, the absolute classification of resistance and endurance, is less applicable (8, 9).
The Floorball sport has many similarities with the Hockey and the studies conducted on the sport of hockey have introduced it as a combination of endurance and strength sports (10, 11), in this study, we tried investigate this modern sport considering that it is less investigated in studies.
In previous study, long-term physical training causes two patterns of cardiac remodeling: First, eccentric hypertrophy, which is seen in endurance sports, and second, concentric hypertrophy, which is seen in strength sports (12).
Eccentric LVH is associated with increased LV mass, LVEDV and normal LVWT, but concentric LVH is associated with increased LVWT and LV mass but normal LVEDV (12, 13).
In our study, men's mean LV diastolic diameter was 5.6 cm/m² ± 0.54, which is at the upper limit of the normal range for non-athletes (14). The Left Ventricular End-Diastolic Volume Index (LVEDVI) in athletes was 76 cc/m2 ± 9.06, exceeding the maximum value of 74 cc/m² found in male non-athletes. All values were within the normal range for women (14).
Endurance sports are linked to increased LV measurements. A study by D’Ascenzi and Oxborough found a strong relationship between endurance exercise and heart chamber enlargement in athletes (15). In a study of Italian athletes participating in 38 different sports, LV end-diastolic diameter (LVEDD) was greater than 55 mm in 45% of the cases, while only 14% exceeded 60 mm (14, 16).
In a study of 500 American athletes, 25% had a LVEDD larger than the normal limit for their sex. However, most athletes showed dilation within the normal range. Thus, establishing a cutoff for LVEDD and LVEDV to diagnose pathological cardiomyopathy is not recommended (17).
In our study, the average LV wall thickness was 9 ± 0.07 mm for male athletes and 8 ± 0.08 mm for female athletes, both within the normal range. The average RWT was 0.35 for males and 0.32 for females. Research shows that LV wall thickness rarely exceeds 12 to 13 mm, whether eccentric (common in endurance sports) or concentric (typical in strength sports) (18-20).
In our study, the average LVEF in male athletes was 54 ± 1.2%, and in female athletes, it was 55 ± 0.8%. Our findings align with previous studies, which have shown that LVEF in competitive athletes is typically preserved or enhanced, generally ranging from 50% to over 55% (21-23).
Research indicates that athletes often have increased LV mass. In concentric hypertrophy, LV mass exceeds 95 g/m2 in women and 115 g/m2 in men, with a RWT over 0.42. In contrast, eccentric hypertrophy shows LV mass above 115 g/m2 in men and 95 g/m2 in women, but with an RWT below 0.42 (14).
In our study, the LV mass was found to be 117 g/m² for men and 89 g/m2 for women, indicating that men had a higher average LV mass. Additionally, the RWT of 0.35 suggested an eccentric hypertrophy pattern in men. In contrast, both the LV mass and RWT in women fell within the normal range.
In some studies, GLS and GCS showed no significant differences between athletes and sedentary control groups. Another study found that GLS and basal circumferential strain were lower in the resistance exercise group compared to the endurance exercise group (24, 25). In our study, the mean GLS was -19.4% for men and -18.4% for women, while the mean GCS was -21% for men and -23% for women. A previous meta-analysis reported average LV strain values of -16.7% for men and -17.8% for women, with GCS values of -22.3% for men and -23.6% for women. These results indicate that our findings are within the normal range (24).
The average diameter of the RV at mid-cavity was found to be 3.38 cm in men and 3.1 cm in women. Among the male athletes studied, three had an RVID measurement exceeding 3.5 cm. However, previous studies reported that the normal range for RV diameter at mid-cavity is below 3.5 cm (14).
In endurance exercise, previous studies have shown an increase in RV cavity size. However, in sports that involve more resistance components, RV sizes are comparable to those of sedentary individuals (26-28). Therefore, since floorball combines elements of both endurance and resistance training, the normal average RV diameter can be understood in relation to this factor
Some studies indicate that RV strain in athletes is lower than the normal level, while other studies suggest that RV strain in athletes is similar to that of sedentary individuals (29). Our study found that the RV strain values were -23% in men and -20% in women, both of which fall within the normal range.
The average of LAVI and RAVI in male athletes was LAVI = 35 ± 5.95 cc/m2 and RAVI = 26 ± 4.80 cc/m2 and in women, LAVI = 29 ± 5.12 cc/m2 and RAVI = 22 ± 3.57 cc/m2, respectively.
Most studies in athletes have confirmed the increase in LA size during endurance exercise, so that in a meta-analysis that examined 54 studies, 13% of athletes showed an increase in LA diameter and up to 30% of athletes showed an increase in LA volume indexed (30). In our study, men had mean LAVI higher than normal (LAVI = 34 cc/m2) but their RAVI was the maximum normal level(RAVI = 28 cc/m2) (31).
The LA has three distinct phases in its function concerning blood flow:
1. Reservoir phase: In this initial phase, the LA stores blood returning from the pulmonary veins while the LV is contracting and undergoing is volumetric relaxation.
2. Conduit phase: During this phase, the LA passively transfers blood into the LV.
3. Contractile phase: In this final phase, the LA actively contracts to transfer blood to the LV during the last part of diastole (32, 33).
Previous studies on LA strain reported reference values of 38% - 41% for the reservoir phase, -38% to -41% for the conduit phase, and -16% to -19% for the contractile phase (34).
In our study, the average LA strain was as follows: Fifty-four percent for men and 52% for women in the reservoir phase; -14% for men and -13% for women in the contractile phase; and -38% for men and -36% for women in the conduit phase. There were no significant differences in reservoir and conduit phase strain between athletes and non-athletes, though athletes showed slightly lower contractile phase strain.
In previous studies, unlike our study LA reservoir function was lower in athletes compared to control groups and such as our study the contractile phase was also lower in athletes (35).
The significance of the LA strain is highlighted by a study showing that the reservoir function of the LA was the most reliable predictor of atrial fibrillation (AF) rhythm in men with a long history of endurance sports (36, 37).
5.1. Conclusions
Our study found that the diameter, volume, and mass of the LV in men were slightly above the upper limits reported in previous studies, while measurements in women were within normal ranges. Both men and women showed normal wall thickness and RWT, indicating a trend toward eccentric hypertrophy.
We observed normal LA strain during the reservoir and conduit phases, with slightly reduced strain in the contractile phase. This represents a new area of research in understanding sports-related physiology and predicting future arrhythmias.
Our study's findings, which differ from those of other research, may be attributed to several factors: The small sample size, the varying levels of exercise, and the different intensities among the athletes. Therefore, we recommend conducting larger studies to better evaluate the effects of combined exercise on the cardiac system