1. Case and Methods
A 76-year-old man presented with 12 months history of worsening shortness of breath and malaise at minimal exertion. He had also developed orthopnoea and paroxysmal nocturnal dyspnoea. Although he had had some response to medical therapy, he still remained occasionally breathless at rest. More recently he had been admitted to the emergency department with acute pulmonary oedema and bilateral pleural effusions. A loud crescendo-decrescendo ejection systolic murmur in the aortic area prompted an echocardiogram, which revealed severe aortic valve stenosis with a transvalvular gradient of 55mmHg with poor left ventricular systolic function but the right ventricular function was good. Henceforth he was referred for urgent aortic valve replacement surgery. While inpatient, he also developed atrial fibrillation (AF), which was successfully treated with intravenous Amiodarone.
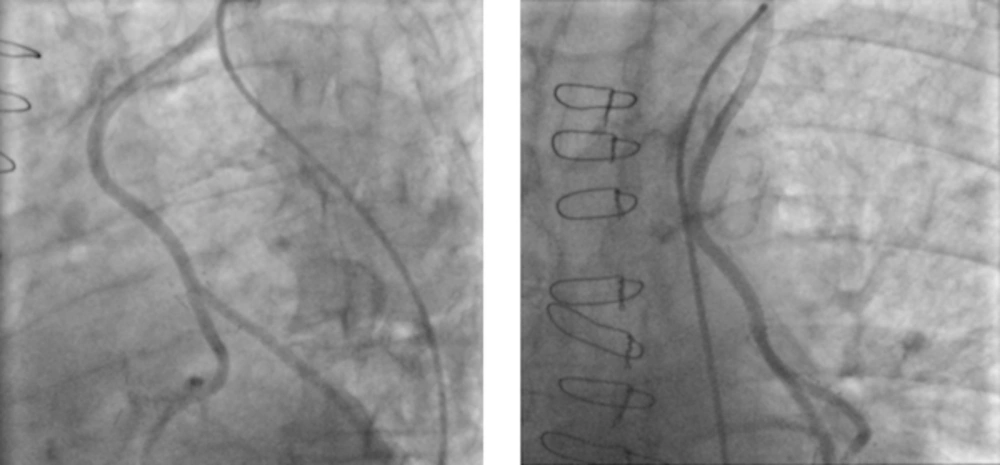
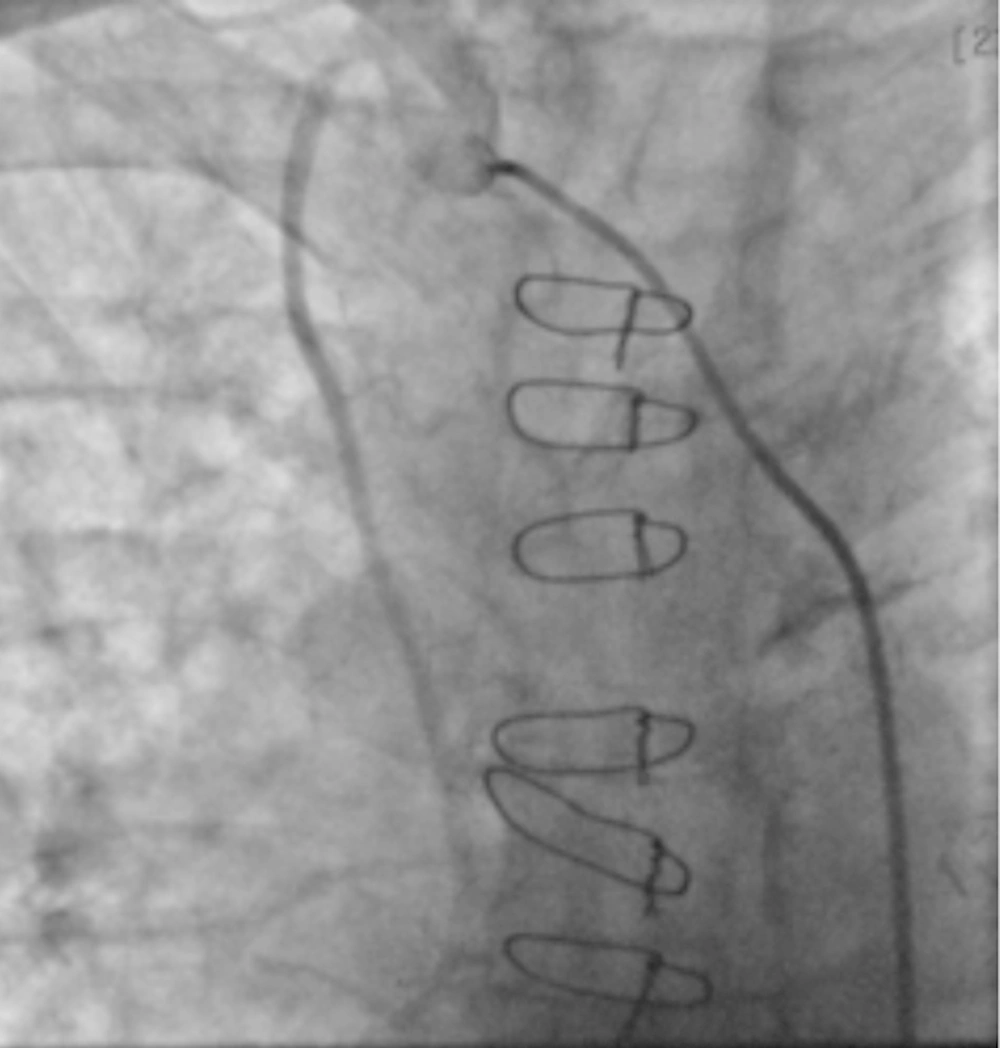
The past medical history of note included; coronary artery bypass grafting (CABG) in 2003 using the left internal mammary artery (LIMA) and radial artery, joined as a Y-graft and anastomosed to the left anterior descending (LAD) and obtuse marginal 1 (OM1) respectively. Furthermore his right internal mammary artery (RIMA) had been extended with a short length of right radial artery graft and anastomosed to distal right coronary artery (RCA). A recent coronary angiogram had demonstrated that all bypass grafts were patent and that there was no residual native coronary flow to his myocardium (Figures 1 and 2). The patient also had type II diabetes mellitus, hypercholesterolemia and hypertension. He was an ex-heavy smoker and had given up smoking following his CABG surgery in 2003. He also had significant peripheral vascular disease (PVD) and had undergone a left femoral endarterectomy and profundaplasty in 2006. Pre-operative haematology and biochemistry were satisfactory.
2. Preoperative Strategy
Percutaneous implantation of an intra-aortic balloon pump (IABP) was attempted via the right common femoral artery. Unfortunately this route proved difficult; because cardiovascular support was so critical in this operation, the right common femoral artery was exposed surgically and the balloon inserted under direct vision.
3. Operative Strategy
The previous sternotomy was opened and substantial adhesions were taken down. The LIMA and the RIMA pedicles were dissected free in order to provide the potential for clamping them should cardioplegic arrest of the heart be required. Intraoperatively, the heart showed poor contractility despite IABP support.
The cardiopulmonary bypass was commenced using aorto-bicaval cannulation and a trans-mitral left ventricular vent. The patient’s temperature was allowed to drift. Carbon dioxide was insufflated across the operative field. The cross clamp was slowly applied across the ascending aorta. No electrocardiographic (ECG) changes indicating acute ischaemia, were observed. Aortic valve replacement (AVR) was then carried out on a beating heart using a size 23 mm Carpentier-Edwards SAV valve. De-airing was carried out through the trans-mitral and root vents and the cross-clamp released. Protamine was administered and the patient de-cannulated.
IABP was removed the following day and the patient was well enough to be discharged home on the seventh post-operative day. During his recovery, the patient experienced a brief period of AF, which was treated by amiodarone therapy, reverting to sinus rhythm on discharge.
At the 6-week clinic review he was free of symptoms.
4. Discussion
Traditionally re-do sternotomy and AVR surgery has been performed under cardioplegic arrest (1). In re-do cardiac surgery, especially in the context of previous coronary artery surgery, poor residual cardiac reserve and multiple cardiovascular and respiratory comorbidities, there are two additional challenges a surgeon faces (1, 2); first, the difficulty in the dissection of adhesions and dissecting out the previous coronary grafts with the potential risk of damage to patent grafts, secondly, is the provision of adequate myocardial protection (1-4). Cardioplegia delivery in the setting of previous coronary grafting may not adequately protect all areas of the heart (1-5).
Beating heart AVR has been reported as a safe operation and an alternative for the patients with pervious CABG (1-5). This case highlights the importance of total arterial revascularisation using both LIMA and RIMA and the Y graft technique in the group of patients who may later require AVR surgery. Additionally our case highlights a surgical strategy in order to increase the margin of safety of the procedure. Since the pre-operative coronary angiography had demonstrated that the native circulation to the myocardium was almost non-existent, the operation was planned such that we would be in a position to clamp both arterial grafts and deliver cardioplegia retrogradely if there was significant ischaemic changes on the ECG upon aortic cross-clamping. Bi-caval cannulation was used because it would have been critical to deliver cardioplegia retrogradely via the coronary sinus as the coronary ostia were not sufficiently patent for the delivery of antegrade cardioplegia in the event of intra-operative myocardial ischaemia. Should clamping of the LIMA and the RIMA be required, the heart could be effectively protected from ischaemic damage using retrograde delivery methods. We therefore used bi-caval cannulation in case the retrograde cardioplegia catheter could not be inserted via the right atrium and direct placement of the coronary sinus cardioplegia catheter became necessary. We elected to perform beating heart AVR surgery to avoid potential myocardial stunning from cardioplegic arrest in a patient with an already poor left ventricular contractility. Mechanical assistance was also provided by intra-operative IABP support.
5. Conclusion
Beating heart AVR can be performed safely in the setting of good bilateral arterial conduits and absence of the native coronary circulation. However, careful forward planning by prophylactic insertion of IABP and bi-caval cannulation allowing the option of delivering cardioplegia directly into the coronary sinus in case myocardial ischaemia was encountered during cross-clamping, would allow for beating heart AVR to be performed safely.