1. Introduction
A trace-to-mild degree of tricuspid regurgitation (TR) is a common finding on echocardiography in individuals with an anatomically normal tricuspid valve (TV). Pathologic TR is divided into primary (organic) and secondary (functional) TR.
The primary involvement of the TV may result in significant TR; it can be seen in acquired heart diseases (e.g., endocarditis, trauma, carcinoid heart disease, rheumatic heart disease, TV prolapse, radiation, drugs, myocardial biopsy, and intracardiac device lead) or in the congenital involvement of the TV.
Nonetheless, most of the secondary or functional cases of significant TR, are related to tricuspid annular dilation associated with leaflet tethering due to volume and/or pressure overload, and it often occurs in the setting of left-heart valve disease (1-7).
In contrast to mitral regurgitation, TR was ignored as a significant disorder for a relatively long time. Latest studies have, however, shown the progressive prevalence of TR especially in association with left-heart valve disease.
It has been suggested that a rise in TR severity begets worse survival (1, 2, 4, 7-9). Whenever TR severity is more than mild, a comprehensive assessment of TV morphology and the mechanisms of the underlying disease besides an evaluation of TR severity based on the latest guidelines should be considered.
Limited data regarding the natural history of severe TR show that it is well-tolerated for years, but the prognosis is poor. The optimal time of surgery, technical choices, and the best medical treatments are still a matter of debate (6, 9-15). Accordingly, we designed a cohort study in the main referral heart center in Iran to assess the survival rates and predictors of the clinical outcomes of medical versus surgical treatment in patients with significant TR.
2. Methods
2.1. Patients
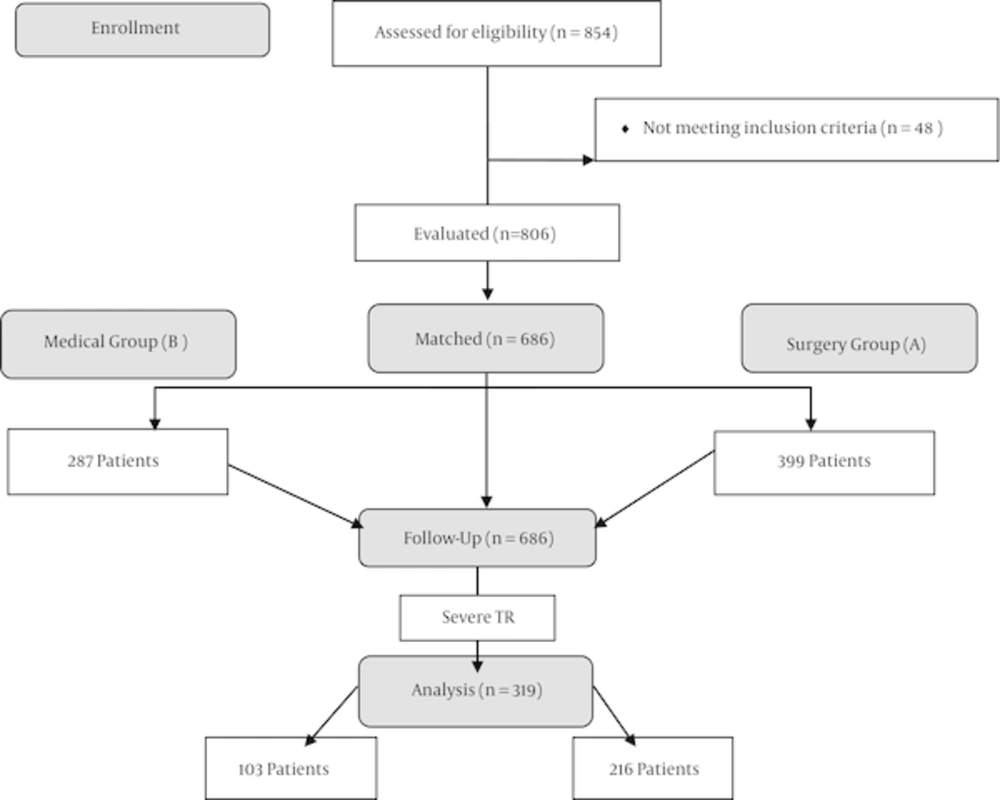
The current 7-year retrospective cohort study, conducted in 2014 at Rajaie cardiovascular, medical, and research center in Tehran, Iran, recruited 806 consecutive patients with significant TR. The study population was divided into 2 groups of surgery and medical treatment. After matching the 2 groups, we selected 686 patients including 319 (46.5%) patients with severe TR. Then based on the patients’ clinical, echocardiographic, and demographic data, we analyzed and compared mortality, cause of death, hospitalization data, and signs and symptoms between the 2 study groups. The mean follow-up time for the medically treated patients was 4.47 ± 3.6 years (1 - 20 y) at a median of 3 years, whereas the mean follow-up for the surgically treated patients was 3.61 ± 1.65 years (0.92 - 7.08 y) at a median of 3.4 years.
The follow-up rate of the patients in the surgical group was 90.6% (406/448), while it was 100% (358/358) among the patients in the medical treatment group.
After matching the patients according to their demographic data in 2 groups of surgery and medical treatment, we chose patients with severe TR and analyzed their outcomes and survival rates from the first admission in the medically treated group and the surgery date in the surgically treated group until death or the last follow-up (See Figure 1) (Flow diagram).
Patients with insignificant TR (less than moderate), severe left-sided heart valve disease, significant complex congenital heart disorders, Ebstein’s anomaly, coronary artery bypass graft surgery, pericardial disease, and all severe comorbidities such as malignancies, severe lung disorders, cirrhosis, recent myocardial infarction (< 3 mon), and end-stage renal disease were excluded.
The protocol of the present study was approved by the ethics committee and the review board of Iran University of Medical Sciences, Tehran, Iran. Informed consent was obtained from all the patients in accordance with the ethical terms of retrospective studies.
2.2. Surgical Techniques
The TR surgery techniques were done according to the surgical findings and the surgeon’s discretion. Totally, 383 patients underwent TV repair. Standard bi-caval cannulation was done for the median sternotomy approach. Those undergoing right thoracotomy had peripheral and superior vena cava cannulation. The surgery was performed via the on-pump beating-heart method or cardioplegic arrest. The surgical techniques consisted of suture annuloplasty (DeVega annuloplasty and suture bicuspidization) in 306 (79.7%) patients, ring annuloplasty in 58 (15.1%) and pericardial patch technique in 19 (4.9%). The types of repair in detail comprised DeVega annuloplasty in 111 (28.9%) patients, suture bicuspidization in 158 (48.2%), commissuroplasty in 9 (2.3%), pericardial patch (MC3, Edwards Lifesciences, Irvine, CA, USA) in 19 (4.9%), replacement in 1 (0.3%), and other types in 1 (0.3%). In the ring annuloplasty surgery, the used rings consisted of rigid MC3 rings (Edwards Lifesciences, Irvine, CA, USA) for 7 (14%) patients, semirigid Carpentier–Edwards annuloplasty rings (Edwards Lifesciences, Irvine, CA, USA) for 6 (12%) patients, and flexible rings (Duran Band, Medtronic, Minneapolis, MN, USA and Sovering Sorin Biomedica, Saluggia, Italy) for 37 (74%) patients. The rings were chosen according to the etiology of TR and the patients’ condition.
The patients in the medical treatment group were treated based on their general condition and the etiology of TR, and loop diuretics and aldosterone antagonists were used to decrease their systemic congestion (ascites and peripheral edema). Digoxin, angiotensin-converting enzyme inhibitors, beta-blockers, anticoagulants, and antiarrhythmics were drawn upon in special situations.
Severe TR was defined based on recent guidelines (1) and either of the following criteria: inadequate cusp coaptation or systolic flow reversal in the hepatic vein (8). In addition, 2D echocardiography was performed using a GE Vivid 3 (Norway) with a 2.5-MHz transducer.
2.3. Statistical Analysis
The statistical analyses were performed using SPSS, version 22 (IBM Inc. Chicago, Illinois, USA), and a P value < 0.05 was considered statistically significant. The descriptive results are reported and compared as means ± SDs (range). The Student unpaired t-test or the Mann–Whitney U-test was employed to compare the quantitative variables, and percentages (frequencies) and the χ2 test or the Fisher exact test were used to compare the qualitative variables. The Kaplan–Meier survival analysis was performed to assess the survival rate of the patients with severe TR, and the log-rank test was applied to compare the 2 groups of surgery and medical treatment. Additionally, the univariate Cox proportional hazards model was utilized to determine the independent risk factors of mortality.
3. Results
3.1. Baseline Characteristics
A total of 806 consecutive patients with TR consisting of surgically and medically treated patients were included in the current study. After matching the 2 groups, we analyzed 686 patients (399 (58.2%) patients in the surgical group), consisting of 216 (31.5%) male and 470 (68.5%) female patients at a mean age of 53.0 ± 13.4 years.
3.2. Characteristics of the Patients with Severe Tricuspid Regurgitation
Out of 686 patients with TR, 319 (46.5%) patients (225 (70.5%) females) at a mean age of 52 ± 13 years had severe TR. Among these patients, 111 (50.2%) patients had New York Heart Association (NYHA) functional classes (FCs) of I and II and 110 (49.8%) patients had NYHA FCs of III and IV. There were no significant differences between the surgically and medically treated patients regarding left ventricular ejection fraction (%) (P = 0.377) and right ventricular function based on tricuspid annular plane systolic excursion (TAPSE) (P = 0.396). Rehospitalization was more common in the medically treated patients than in the surgically treated ones (P = 0.005).
Tables 1 and 2 summarize the baseline demographic and clinical characteristics as well as the echocardiographic data of the patients with severe TR.
| Group | Mortality | Sex | NYHA | Cause of Death | TR Etiology |
|---|---|---|---|---|---|
| Surgery | 17 (7.9) | Male/female 67/149 | I & II: 72 (47.1) | Noncardiac: 7 (46.7) | Primary: 167 (79.1) |
| III & IV: 81 (52.9) | Cardiac (non-HF): 5 (33.3) | Secondary: 44 (20.9) | |||
| Cardiac (right HF): 3 (20) | |||||
| Medical | 4 (3.9) | Male/female 27/76 | I & II: 39 (57.4) | Noncardiac: 1 (25) | Primary: 21 (21.6) |
| III & IV: 29 (42.6) | Cardiac non-HF: 1 (25) | Secondary: 76 (78.4) | |||
| Cardiac right HF: 2 (50) | |||||
| P Value | 0.23b | 0.37 | 0.15 | 0.47 | < 0.001 |
Abbreviations: HF, Heart failure; NYHA, New York Heart Association functional class; TR, Tricuspid regurgitation.
aValues are expressed as No. (%).
bP value shows the difference between the surgical and medical groups.
| Variable | Medical Group | Surgery Group | P Valueb | |
|---|---|---|---|---|
| RV Function | Normal | 9 (8.7) | 7 (3.3) | 0.10 |
| Mild dysfunction | 22 (21.4) | 31 (14.6) | ||
| Moderate | 53 (51.4) | 132 (62.2) | ||
| Severe | 19 (18.4 ) | 42 (19.8) | ||
| IVC Diameter | < 1.5 | 16 (15.7) | 10 (9.4) | 0.03 |
| 1.5 - 2.5 | 75 (73.5) | 71 (67.0) | ||
| > 2.5 | 11 (10.8) | 25 (23.6) | ||
| IVC Collapse | > 50% | 42 (40.8) | 26 (23.4) | 0.006 |
| < 50% | 61 (59.2) | 85 (76.6) |
Abbreviations: IVC, inferior vena cava; RV, right ventricle; TR, tricuspid regurgitation.
aValues are expressed as No. (%).
bP value demonstrates the difference in variables between the medical and surgical treatment groups.
3.3. Survival and Risk Analysis
At a follow-up time of 3.2 ± 1.6 (0.91 - 7) years, the rate of death was 6.6% for the patients with severe TR (n =319): 5.32% in the surgical treatment group and 1.25% in the medical treatment group. The 5-year survival rate in patients with severe TR was 87% in the surgical treatment group and 90.4% in the medical treatment group (Table 2). In patients with severe TR in the NYHA FCs of III and IV, the 5-year survival rate was 78.6% in the surgical treatment group and 60.6% in the medical treatment group (Table 3, Figure 2). In the patients with severe TR, the Cox regression analysis for assessing the risk factors of mortality showed that in the surgical treatment group, age at surgery (HR = 1.06), preoperative NYHA FC (HR = 2.13), inferior vena cava (IVC) size (HR = 4.33), length of admission (HR = 1.02), ICU stay days (HR = 1.04), postoperative complications (HR = 7.79), and ICU intubation hours (HR = 1.002) were the significant independent risk factors of mortality, whereas in the medical treatment group, age (HR = 1.07), NYHA FC (HR = 4.52), symptoms–including chest pain (HR = 4.55), ascites (HR = 11.50), and peripheral edema (HR = 13.66), TR etiology (secondary/primary: HR = 0.26), and IVC size (HR = 2.97) comprised the significant independent risk factors of mortality (Tables 4 and 5). There was a significant correlation between overall mortality and the NYHA FC (P = 0.009), patients’ symptoms–including chest pain (P = 0.014), ascites (P < 0.001), and peripheral edema (P < 0.001), TR etiology (P = 0.016), and IVC size (P = 0.002).
| Group | Surgery | Medical | Surgery | Medical | Surgery | Medical |
|---|---|---|---|---|---|---|
| NYHA FC I and II | NYHA FC III and IV | |||||
| 1 year | 100 | 99 | 100 | 100 | 100 | 96.6 |
| 2 years | 99 | 97.7 | 98.1 | 100 | 97.2 | 90.9 |
| 3 years | 94.4 | 95.4 | 96.1 | 94.7 | 90.4 | 90.9 |
| 5 years | 87 | 90.4 | 96.1 | 94.7 | 78.6 | 60.6 |
Abbreviations: NYHA FC, New York Heart Association functional class; TR, Tricuspid regurgitation.
| Risk Factors | HRa | 95%CI | P Value |
|---|---|---|---|
| Age at surgery | 1.06 | 1.03 - 1.10 | < 0.001 |
| Length of admission | 1.02 | 1.009 - 1.04 | 0.003 |
| ICU stay days | 1.04 | 1.02 - 1.06 | < 0.001 |
| Postoperative bleeding | 10.62 | 3.80 - 29.60 | < 0.001 |
| Postoperative mediastinitis | 7.79 | 1.013 - 60.06 | 0.04 |
| Mechanical ventilation time, h | 1.002 | 1.001 - 1.003 | < 0.001 |
| Preoperative NYHA FC | 3.13 | 1.47 - 6.63 | 0.003 |
| IVC size | 4.33 | 1.59 - 11.79 | 0.004 |
Abbreviations: HR, hazard ratio; IVC, inferior vena cava; NYHA FC, New York heart association functional class.
aThe ratio of the hazard rates corresponding to the conditions described by 2 levels of an explanatory variable.
| Risk Factors | HRa | 95%CI | P Value |
|---|---|---|---|
| Age | 1.07 | 1.03 - 1.11 | < 0.001 |
| NYHA FC | 4.52 | 1.29 - 15.88 | 0.01 |
| Chest pain | 4.55 | 1.26 - 16.41 | 0.02 |
| Ascites | 11.50 | 2.31 - 57.27 | 0.003 |
| Peripheral edema | 13.66 | 1.72 - 108.10 | 0.01 |
| TR etiology | 0.26 | 0.07 - 0.91 | 0.03 |
| IVC size | 2.97 | 1.54 - 5.71 | 0.001 |
Abbreviations: HR, hazard ratio; IVC, inferior vena cava; NYHA FC, New York heart association functional class; TR, Tricuspid regurgitation.
aThe ratio of the hazard rates corresponding to the conditions described by 2 levels of an explanatory variable.
4. Discussion
The optimal timing for TR surgery and determination of the risk factors of increased mortality in patients with severe TR have yet to be fully elucidated. Delayed surgery may result in irreversible right ventricular function and poor surgical outcomes.
In the present study, we sought to determine the predictors of a poor outcome and increased mortality in patients with severe TR who underwent medical and surgical treatment.
Our findings showed that overall mortality in the patients with severe TR had a significant correlation with the patients’ NYHA FC, symptoms (ascites, peripheral edema, and chest pain), and IVC size. In patients with severe TR and NYHA FCs of III and IV, the 5-year survival rate was more desirable in the surgically treated patients than in patients in the medical treatment group. However, surgical mortality increased with a higher NYHA FC, which may suggest earlier surgery before reaching NYHA FCs of III and VI.
In a study by Kim et al. (11), the 5- and 10-year survival rates of patients who underwent surgery were 82.4 ± 1.9% and 71.7 ± 2.8%, which are very similar to those in our study, in which the 5-year survival rate of the surgically treated patients was 87%. Other studies have reported different surgical outcomes and event-free survival rates. For instance, Kim et al. (9) reported 9.8% mortality and 75% event-free survival rates at a median of 32 months follow-up and Staab et al. (16) demonstrated 8.8% early mortality with a 5-year event-free survival rate of 41.6% in 34 patients, who suffered from severe TR after left-side valve surgery.
A cohort study on 92 patients undergoing isolated TV surgery demonstrated 30-day, 3-month, 5-year, and 10-year mortality rates of 7.9%, 15.2%, 25.7%, and 53.7% respectively (14). In a study by Topilsky et al. (10) on 353 patients with isolated TR from 1995 to 2005, 144 (40.8%) patients were diagnosed to have severe isolated TR; however, the 10- year survival rate was 63 ± 5%. In our study, age, NYHA FC, symptoms (chest pain, ascites, and peripheral edema), TR etiology, and IVC size were the significant independent predictors of a poor outcome for both groups, while age at the time of surgery, length of admission, ICU stay days, postoperative complications, ICU intubation period, preoperative NYHA FC, and IVC size were the significant independent risk factors of mortality in the surgical treatment group. In a study by Kim et al. (9), the level of hemoglobin before surgery and echocardiographically assessed right ventricular function were found to be the independent predictive factors of a postoperative outcome.
Kim et al. (11) reported that the risk factors of mortality were comprised of age, NYHA FC, sex (male), cirrhosis, preoperative levels of hemoglobin, albumin level, and estimated glomerular filtration rate. The type of the TR procedure was not a significant predictor of death, which chimes in with our results.
Yiu et al. (17) showed that the diameter of right ventricular mid-cavity and the area of tethering in the TV before TV annuloplasty were the essential predictive factors of survival after surgery. Likewise, De Meester et al. (14) demonstrated that age, extracardiac vascular disease, glomerular filtration rate , NYHA FC, and mean pulmonary artery pressure were the predictive factors of death. A cohort study by Kim et al. (15) found that preoperative anemia, renal or hepatic dysfunction, right ventricular dilation, and postoperative TR were the risk factors of a poor prognosis.
All these findings underscore the notion that the survival rate after TR surgery is affected by preoperative factors such as advanced right-sided heart failure symptoms, comorbidities, and end-organ failure more than the type of the surgery.
Since TR is diagnosed when patients are in advanced stages, the disease is usually in tandem with other complications such as right-heart dilation, atrial fibrillation, and congestive heart failure (4).
Given the substantial effect of TR on patients’ quality of life and survival, optimal timing of surgery would confer a better prognosis (8, 15, 18-21). Surgical treatment may yield more optimal results in the long term. Moreover, the surgical repair of TR may confer more desirable results in early stages before the occurrence of ascites and peripheral edema, severe right ventricular enlargement, and right ventricular dysfunction as the longer clinical course of TR cause greater degree of right ventricular failure and increases operative mortality.
Limitations of the Study: The main limitations of our study are its retrospective design and limited follow-up period. In this study most of the patients underwent suture annuloplasty (DeVega annuloplasty and suture bicuspidization) and just 15.1% of the patients underwent ring annuloplasty. Other comprehensive prospective studies with longer follow-up periods are, therefore, needed.
![Survival Functions of Patients with Severe Tricuspid Regurgitation (New York Heart Association [NYHA] Functional Classes III and IV) in the Medical and Surgical Treatment Groups. Survival Functions of Patients with Severe Tricuspid Regurgitation (New York Heart Association [NYHA] Functional Classes III and IV) in the Medical and Surgical Treatment Groups.](https://services.brieflands.com/cdn/serve/3170b/9b5276c35e0b7a4f2c047cf39a271ded96bf10e1/mca-In_Press-In_Press-9469-i002-preview-preview.webp)