1. Case Presentation
We report a 30-year-old male with a history of deep vein thrombosis (DVT) the previous year who referred to us for further evaluation one week after an acute episode of right sided sensorimotor hemiparesis and dizziness. The symptoms disappeared over a 24-hour period without any sequelae. He had another episode of transient ischemic attack (TIA) in which he experienced speech disturbance. He has also had cigarette smoking in his habitual history.
No pathological finding was detected on physical examination. Blood pressure was 121/76 mmHg on admission and blood pressure monitoring during hospital stay was within normal values. Laboratory tests including red and white cell blood count, blood sugar, cholesterol, and coagulation factors (protein C and S, anthithrombin III, prothrombin mutation) and antiphospholipid antibodies revealed no pathological findings, however homocysteine level was 16 micromoles/liter which is considered high (normal levels between 5 - 15 micromoles/liter).
Twenty-four-hour ECG Holter monitoring showed no evidence of atrial fibrillation. Brain magnetic resonance imaging showed neither cerebral hemorrhage nor evidence of ischemic stroke and or atherosclerosis of the brain arteries. Color and pulse duplex study of carotid and vertebral arteries showed normal flow without evidence of significant atherosclerotic plaque.
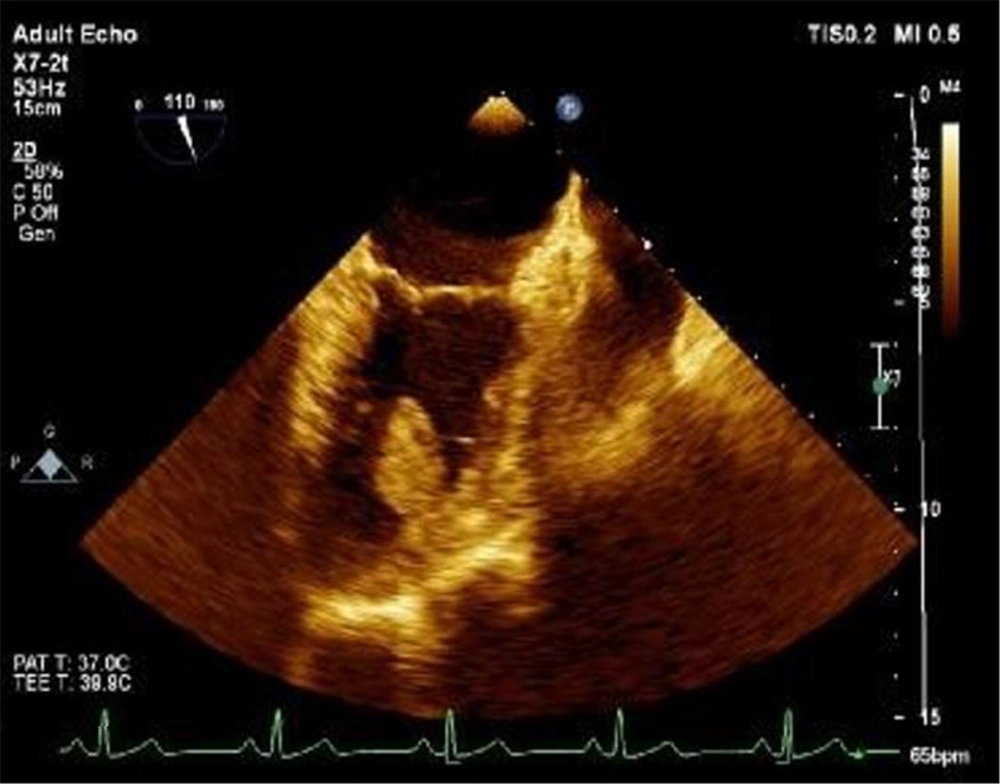
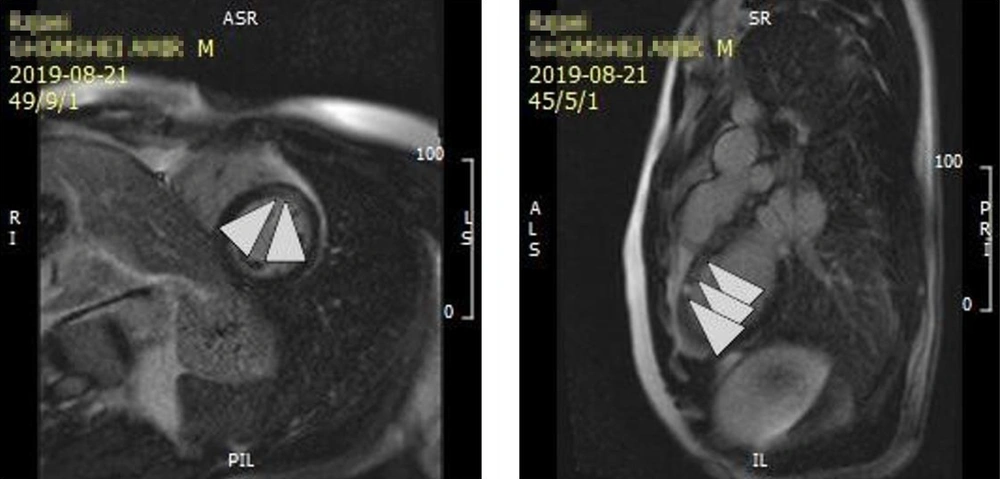
Interestingly, transthoracic and transesophageal echocardiography revealed normal LV size with mild LV dysfunction (GEF = 50%), no significant RWMA at rest, no LVH, normal RV size and function, a large pedunculated, hypermobile, hyperechoic LV mass measuring 2.7 cm in length and 1.39 cm in width attached to anteroseptal segment with a narrow stalk (Figures 1 and 2). Cardiac magnetic resonance (CMR) imaging showed normal LV size without LVH and with mild to moderate LV dysfunction (LVEF = 45%) and normal RV size and function (RVEF = 51%). Based on MRI criteria, no obvious finding of myocardial edema was found. The presence of a tiny thick linear strip of mid myocardial scar at basal and mid anteroseptal segments, according to CMR tissue characterization criteria, post myocardial fibrosis in basal and mid anteroseptal segments suggested (Figure 3).
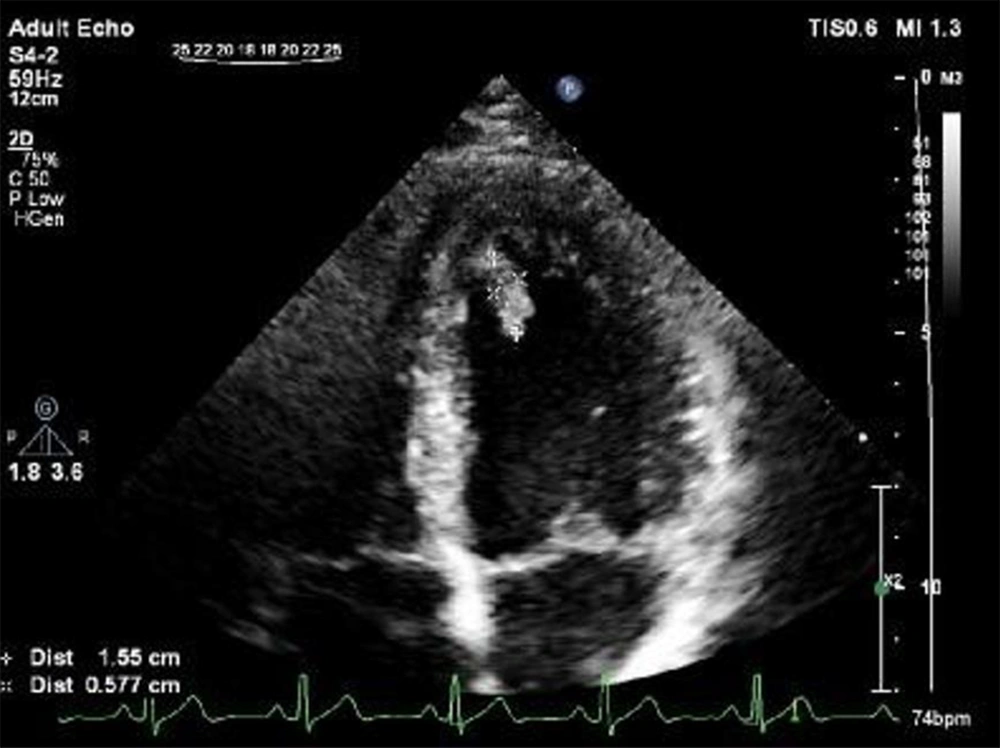
The patient was placed on Enoxaparin 80 mg BID. After two weeks of follow up, echocardiography revealed significant resolving thrombus measured 1.55 cm in length and 0.57cm in width during 2 weeks (Figure 4). He was discharged after we were satisfied that the repeated international normalized ratio (INR) values were within the therapeutic range (1, 2). Folic acid and vitamin B12 (100 - 500 mg/day) was prescribed.
2. Discussion
LV thrombus is a serious diagnosis that can be reported in myocardial infarction (3), various types of cardiomyopathies (1, 2), and myocarditis (4). It can also be presented in case of systemic inflammation and hypercoagulable state (5). Left ventricular thrombus is commonly observed in patients with myocardial infarction with systolic dysfunction, but it is difficult to diagnose when such situation occurs in a patient without a history of coronary artery disease and normal ventricular function (6).
There is an increased risk of thrombus formation in myocarditis due to inflammation and stasis secondary to the decreased systolic function. Viral myocarditis leads to a hypercoagulable state due to an increase in myocardial tissue factor. In myocarditis thrombophilia is the cause of thrombus formation and the most important risk factors are MTFHR (C677T) gene mutation and hyperhomocystenemia (7). The incidence of homocystinuria all over the world varies between 1 in 50000 and 1 in 200000 (8). Ucar et al. (9) reported that hypercoagulable state such as FV Leiden, prothrombin 20210 and MTHFR gene mutations play no role in left ventricular thrombus formation in myocardial infarction. However, in another study hyperhomocysteinemia is an independent risk factor for myocardial thrombosis in myocardial infarction (10). It is essential to consider homocysteinemia as an important differential diagnosis in patients with cardiac thrombosis. Left ventricular thrombus formation has also been reported in patients with normal left ventricular dimensions and systolic function due to hypercoagulable states such as raised homocysteine level (11). Studies have shown that increased levels of homocysteine are associated with increased risk of heart attack and stroke (12). High levels of homocysteine are associated with low levels of vitamins B6, B12 and folate and also in chronic renal diseases (12). Hyperhomocysteinemia leads to endothelial cell damage, reduction in flexibility of vessels, and alters the process of hemostasis (11). It is suggested to perform thrombectomy in order to reduce cardiovascular risk along with proper anticoagulation and administration of vitamin B12, vitamin B6 and folate regardless of the levels before treatment.
2.1. Conclusions
In this case report thrombus formation can be explained by previous inflammation (myocarditis) and hypercoagulable state due to hyperhomocysteinemia. So, high degree of suspicion of cardiac source is essential in any patient referred with repeated episodes of TIA or cerebrovascular accident even with normal ventricular function.
.jpg)