1. Introduction
Living with a single ventricle has numerous restrictions and the natural history of a univentricular heart without cardiac surgery is calamity (1). In July 1971, for the first time, the Krutzer procedure was done by Dr Guillemo. O. Krutzer in Ricardo Gutierrez Children Hospital at Buenos Aires, Argentina. The patient was a 3-year-old boy with tricuspid atresia, and the procedure was atriopulmonary anastomosis (APA). A homograft was inserted between the main pulmonary artery and right atrium appendage, and a 6 mm fenestration was created in interatrial septum. In the December of the same year for another patient with similar condition, the surgical team performed APA by direct connection of right atrial appendage to pulmonary valve and pulmonary root of patient. In the above procedure right atrium works just as a pathway and never functions as a pump (2). Survival of patients with tricuspid atresia associated with normally related great arteries, small ventricular septal defect (VSD), and pulmonary stenosis (type 1b) depends on a balance between systemic flow and pulmonary flow. At birth, pulmonary blood flow may be through antegrade pathway i.e. right ventricle or through retrograde pathway or patent ductus arteriosus, or it may be through both pathways. Circulatory changes after birth include decreased pulmonary resistance, PDA closure, and increased right ventricular outflow tract obstruction which may change the balance between systemic blood flow and pulmonary blood flow. Providing an appropriate pulmonary blood flow requires a suitable surgical procedure. Systemic to pulmonary shunts, or connection of superior vena cava to pulmonary artery produces increased pulmonary blood flow. Procedures like PDA closure or PA banding decreases pulmonary blood flow. Several previous reports (3, 4) showed that prior B-T shunt is a risk factor for death in univentricular patients. B-T shunt may be a predisposing factor for decreased cardiac output and increased morbidity at perioperative period. Patients with previous B-T shunt, at the time of superior cavopulmonary connection require more pulmonary artery arterioplasty than patients with previous PA banding.
Long-term outcomes of Fontan circulation include: increased pulmonary vascular resistance, increased systemic venous pressure, chronic low-cardiac output state, right ventricular dysfunction and failure of single ventricle repair. Increased systemic venous pressure has negative effects on renal and hepatic function (5).
2. Case Presentation
A 28-year-old man was admitted in pediatric cardiology ward due to puffiness of face and feet, and mild cyanosis since 2 months ago. In the past medical history, the first admission of patient was at the age of 18 due to severe cyanosis, and fatigability. Complete cardiologic evaluation at that time revealed congenital heart disease of tricuspid atresia, ventricular septal defect, and pulmonary atresia. Under diagnosis of univentricular heart, Fontan/Krutzer procedure had been performed for patient successfully. Cyanosis and other clinical symptoms were abolished. The patient was discharged with administration of warfarin and regular out-patient follow-up. The patient was lost to follow-up after discharge from hospital i.e. since 10 years ago. He stopped taking warfarin since 6 years ago. He is a heavy smoker and consumes alcohol. He is married and has a 6-year old daughter. The patient is living in a remote village of Sanandage in Kurdistan Province.
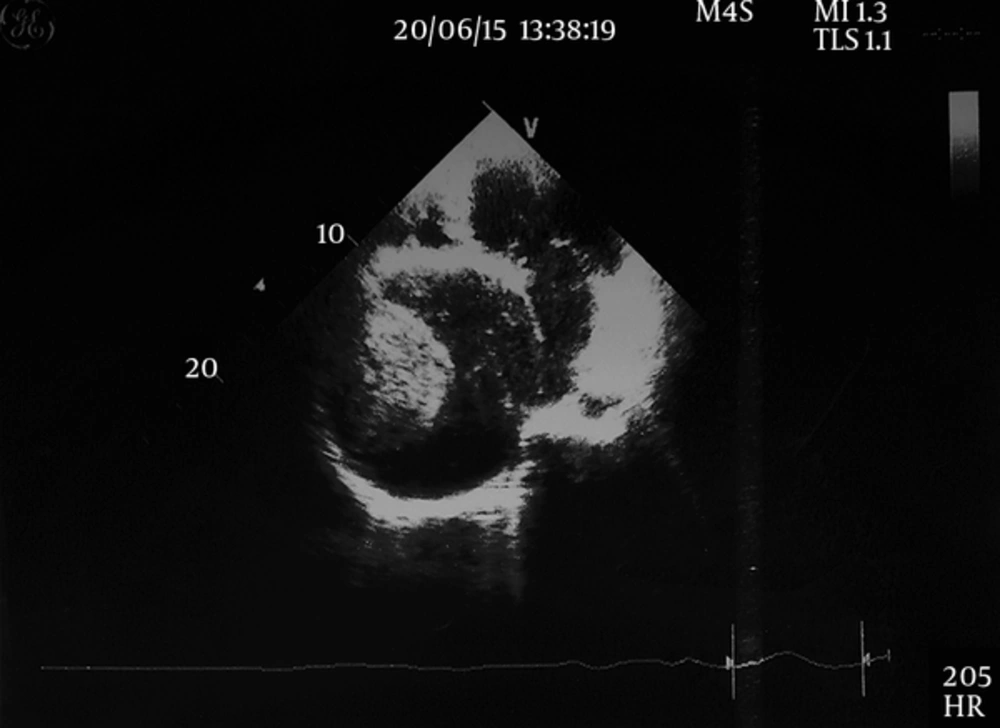
In physical examination the patient was pale and puffy. A grade 3/6 systolic murmur was audible at subxiphoid area. The liver was 6 cm below costal margin. Pitting edema was detected at lower extremities. Chest X-ray revealed massive cardiomegaly with right atrial and ventricular enlargement. ECG showed atrial flutter with variable ventricular response. Echocardiography showed dilated right atrium and right ventricle (Figure 1). A large clot measuring 7 × 7 cm was observed in right atrium and a massive right pleural effusion measuring 6 cm was evident. Laboratory tests showed normal values of electrolytes. Liver function tests were normal. Creatinine was 1.86 mg/dlL. Blood culture was negative for three times. Urinalysis was normal. Abdominal sonography showed right hydroureteronephrosis, enlargement of spleen, cirrhotic changes of liver, and gall bladder stones. The patient underwent cardiac surgery to remove right atrial clot and for the drainage of pleural effusion. The large clot was removed successfully (Figure 2). Culture of removed clot showed mycelium of fungous. The patient was suffering from fever. Amphotericin-B was started via intravenous route. There was no substantial response to treatment and after 2 weeks the patient began to complain of headache. Brain MRI revealed a small subcortical mass possibly with fungal origin and medical therapy was recommended. Antifungal treatment was changed to intravenous voriconazole. After 1 week of treatment the headache disappeared and the general condition of patient was improved dramatically. After 2 weeks the patient was discharged with oral voriconazole for 4 weeks, daily warfarin and outpatient follow-up. One month after discharge the patient was readmitted for Conversion surgery. A fenestrated extracardiac conduit was inserted between inferior vena cava and right pulmonary artery (modified Fontan operation). Two days after the surgery the patient died due to intractable heart failure and multiple organ dysfunctions.
3. Discussion
Irrespective of chronic impairment in cardiac output, atriopulmonary anastomosis (APA) or Fontan/Krutzer (F/K) procedure dramatically improves the quality of life and prognosis in patients with tricuspid atresia type 1b. After surgery approximately 70 percent of patients had 25 years survival. Seventy-five percents of survivors are in NYHA functional class1 and have exercise tolerance up to 60% of predicted values. Several of progressive side effects included: edema secondary to increased systemic venous pressure, congestive heart failure, arrhythmia, thromboembolia, protein losing enteropathy, hypoalbuminemia, sudden death, etc. Patients with several episodes of arrhythmia, irrespective of treatment with amiodarone, and those with right atrial thrombosis needed reoperation. Central tunnel technique or conversion is considered for failing APA (1). Our patient was lost to follow-up and did not use warfarin. Large thrombosis in right atrium and atrial flutter were the consequences of his negligence as well as the side effects of surgery.
Survival after 40 years of age is difficult for a patient with tricuspid atresia and F/K palliation. The longest duration of survival after F/K operation has been reported for a 53-year- old female with tricuspid atresia (type b1). At the age of 49 years, the patient became symptomatic due to a large interatrial thrombosis, atrial flutter, and severe hydrothorax. She underwent Conversion (modified Fontan) surgery. Three years after conversion, she is in good clinical condition, sinusal rhythm, and acceptable exercise test (6). Gradual decline in functional class is observed in patients with the following complications: congestive heart failure, arrhythmia, thromboembolia, protein losing enteropathy, plastic bronchitis. At the present time, 80 percent of patients with univentricular heart can survive 20 years, after, at least three cardiac surgeries. Hepatic and renal dysfunctions have important prognostic roles. The results of cardiac transplantation are not ideal in univentricular heart. Sometimes, progressive increase in pulmonary vascular resistance occurs after cardiac transplantation. Patients with end stage renal failure are exempted from conversion and are candidate for heart transplantation. Progressive increased pulmonary vascular resistance has been reported after heart transplantation (2). Renal and hepatic functions were compromised in our patient and he was not a good candidate for heart transplantation. Fontan circulation is poorly tolerated in pregnant female patients. Decline in cardiovascular condition is common in the third trimester. Common complications include: premature labor, intrauterine growth retardation, increased risk of Cesarean section, and fetal anomalies due to anticoagulants (7). Our patient was male and had a 6-years old healthy daughter.
3.1. Conclusion
The future efforts should be finding a better technique for improving the outcomes in univentricular-heart patients. This can be achieved by finding a new device or improving heart transplantation procedure. At the present time F/K surgery, irrespective of its long-term complications is a good palliative operation in congenital heart diseases.