1. Introduction
Kawasaki disease (KD) is a systemic vasculitis syndrome usually presented with acute fever which occurs primarily in children younger than 5 years of age. This condition was first described by Dr. Tomisaku Kawasaki in 1967 (1). Clinical criteria play an important role in the diagnosis of KD mainly because specific laboratory tests are unavailable (2). Diagnosis of KD needs the presence of 5 from the 6 clinical criteria (3) including typical Kawazaki fever, mucosae involvement of lips tongue and pharynges, bilateral conjunctivitis, polymorphous exanthema, peeling of toes and fingers and also significant cervical lymph node enlargement.
Currently KD is known as the most common etiology of acquired cardiac disease in children in developed countries (4). The disease occurs throughout the year although it is more common in spring and winter (5). Heart involvement in Kawazaki disease can present with myocarditis, pericarditis, thrombosis or stenotic lesions of coronary artery aneurysm that are at risk of MI (6), congestive heart failure and sudden cardiac death. Early recognition and treatment with IVIG (7) and high dose aspirin (8) will significantly reduce the incidence of this complication.
2. Case Presentation
A 25-year-old man was referred to our center with resting chest pain and anterior ST-segment elevation myocardial infarction (STEMI) 10 days ago. He had a history of Kawasaki disease in about 17 years ago. His coronary angiography in the previous center showed ectasia in proximal part of left anterior descending artery (LAD) followed by totally cut off at mid part and also a large aneurysm at proximal part of right coronary artery (RCA) with chronic dissection. Primary percutaneous coronary intervention (PCI) attempts in acute phase failed due to unsuccessful wiring of LAD and concerns about LAD dissection as a complication. The patient was then referred to our tertiary center for further evaluation and treatment.
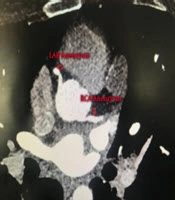
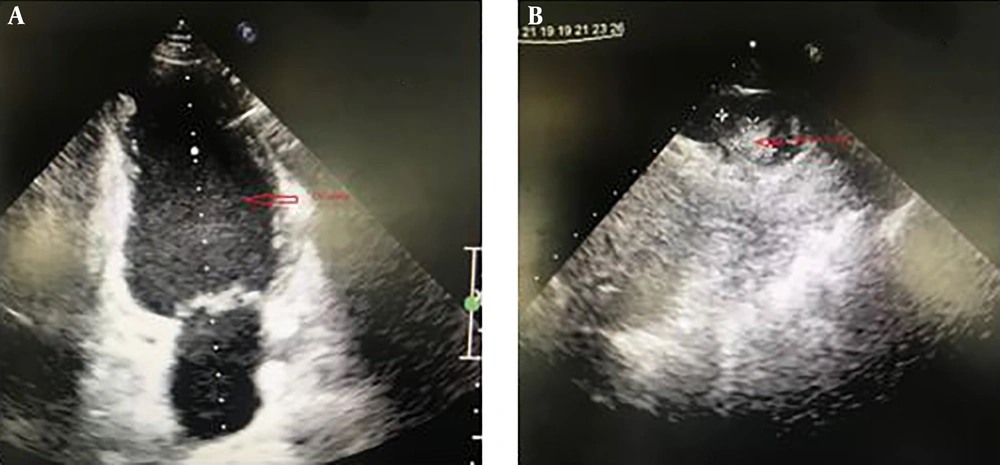
Echocardiogram in our center showed mild left ventricle (LV) enlargement with left ventricle ejection fraction (LVEF) of 20% - 25% and fixed apical clot (9 × 18 mm) (Figure 1). The coronary CT angiography was performed to obtain more detailed information about LAD territory. Aneurysmal dilation at proximal part of LAD with total stenosis at mid part and aneurysmal dilation of RCA at proximal part with thrombotic stenosis was revealed in this study (Figure 2). Also, cardiac MRI showed moderate enlargement of left ventricle and severe systolic dysfunction (LVEF = 25%) with moderate viability in LAD territory. Also, it showed a 20 × 6 mm mural clot attached to LV apex.
His laboratory data showed no important abnormalities (troponin = 0.35, creatine kinase myocardial band (CKMB) = 18, hemoglobin = 15, white blood cell count = 6500, platelet count = 246000, BUN = 13, creatinine = 1, Na = 136, K = 4.3).
The patient underwent successful CABG and closure of coronary aneurysms, and 7 days after the surgery, the patient was discharged with good condition.
3. Discussion
The two most common vasculitis are Kawasaki disease and Henoch-Schonlein purpura (9). No specific agent has yet been identified as a standard laboratory marker. It has been shown that infiltrative inflammation consists of macrophages and also IgA plasma cells and CD8 T-lymphocytes in involved coronary arteries.
The cardiovascular system involvement of KD includes myocarditis, coronary arteritis, pericarditis, congestive heart failure and sudden cardiac death. Although coronary artery disease is the most common complication, the need for revascularization in such patients is quite rare (10). The incidence of coronary aneurysm is 20% in untreated cases. The diagnosis of KD is clinical with a few non confirmatory supportive investigations (11). Treatment with IVIG relieves the acute inflammation and reduces the rate of coronary aneurysms.
Maximal benefits can be achieved when IVIG is administered within the first 10 days of the disease. In acute phases high dose aspirin can be given because of its anti-inflammatory effect. Low dose aspirin can also be administered for its antiplatelet activity function if the patient could remain afebrile for 2 - 3 days. This type of management results in good prognosis and most relapses may happen within 2 years from the first episode.
Our patient with history of Kawasaki disease 17 years ago now at 25 years of age suffers from one of the rare complications of Kawasaki disease, anterior STEMI with LAD and RCA aneurysm and stenosis and also severe LV dysfunction who underwent surgical repair of coronary aneurysm and CABG at our center due to a recent history of unsuccessful coronary artery revascularization with PCI. The patient post-operative course was uneventful and was discharged 7 days after the surgery without any complications. One month after surgery patient visited in outpatient clinic without chest pain or any other problem, he was in functional class I. His transthoracic echocardiography showed moderate LV enlargement with LVEF = 25% without LV clot and significant valvular dysfunction. We conclude that the surgical management of cardiac disease in Kawasaki patients could be safe and effective.