1. Background
Anxiety is a well-known phenomenon in a society that is manifested in different stages of people’s lives with its positive and negative outcomes (1). Anxiety is a consciously perceived feeling of tension that is associated with the stimulation of the autonomic nervous system (2). It is characterized by impaired social and occupational activities (3). Practitioners of specific jobs like healthcare workers, including physicians and nurses, are at a high risk of anxiety (4). Previous studies have illustrated that, in general, the prevalence of anxiety is higher in nurses than in the general population (5). In particular, nurses working in Intensive Care units (ICUs) tend to experience more anxiety and tension than other nurses due to the constant experience of critical situations (6, 7). Zandi et al. (8) showed that nurses in the ICU, kidney transplantation unit, and Emergency Department (ED), among other hospital units, experience severe and highly severe stress. Given the relatively high prevalence and the negative effects of anxiety on nurses, it is imperative to find and implement efficient coping methods.
Resilience is a coping strategy that helps individuals to face stressful conditions and saves them from pathogenic disorders and life problems (9-11). Resilience skills can empower nurses to sustain themselves in difficult and challenging work settings (12). Mealer et al. (6), in a national survey showed that the presence of resilience is associated with a healthier psychological profile in ICU nurses. Magtibay et al. (13) conducted a study on the efficiency of stress management and resilience programs on anxiety and depression of nurses. The results confirmed a notable improvement in anxiety, personal depression, and job burnout.
Another efficient therapeutic method to control the symptoms of anxiety is metacognitive therapy (MCT) (14). The term “metacognitive” was first used by Flavell (15) to refer to the process of “thinking about thinking” and the knowledge of what one knows and does not know. In other words, metacognitive is a multifaceted concept that refers to the knowledge and beliefs about thinking and approaches used by individuals to regulate thought processes and eliminate the mechanisms that cause maladaptive self-control (14-16). Previous studies have supported the efficiency of MCT in some of the psychological problems such as anxiety and depression (17, 18).
Overall, evidence has demonstrated that there are high incidence rates of anxiety (approximately 40% - 46% prevalence rates) among Iranian nurses (19, 20). However, a few studies have been conducted on nurses’ anxiety to determine proper interventions to manage it and/or introduce the most effective intervention. To compare the resilience training and MCT in Iran, the results of a study by Zamirinejad et al. (18) showed that among female students, there was no significant difference in the depression score between resilience and MCT groups after the intervention. Nevertheless, there is no research, yet, to compare the effects of these two programs on the anxiety of nurses in Iran.
2. Objectives
The present study is an attempt to compare the effects of resilience skills training and MCT on the anxiety of intensive care and ED nurses.
3. Methods
3.1. Design and Participants
A randomized controlled field trial was conducted with a pretest/posttest/follow-up design performed on ICU, PICU, NICU, and ED nurses in Valiasr Hospital, Birjand City, Iran.
The sample size was calculated as 21 subjects per group according to a similar previous study (21) using the following formula with the confidence level of 95%, power of 90%, and attrition rate of 15%.
Out of 90 nurses working in the units under study, 63 were selected through convenience sampling. The inclusion criteria included at least one year of work experience in ED or ICUs, not using psychiatric medications over the past month, no history of psychological problems or physical disease, and no participation in anxiety management workshops over the past six months. The exclusion criteria included missing two intervention sessions, going on vacation, changing the work unit, and reluctance to participate.
After briefing the participants about the objectives of the study and asking them to sign an informed letter of consent, the participants were asked to fill out a demographics form and the Spielberger anxiety inventory. Then, the participants were randomly allocated to three groups of resilience, MCT, and control (21 members in each group) using the permutation blocking method.
3.2. Interventions
The resilience group received resilience skills in eight sessions (45 min, twice a week) by the researcher. The education program was based on the Henderson resilience protocol (22) introduced in 1996 to create safe schools in the USA. The content, based on a literature review, was confirmed by experienced nursing professors.
The MCT group participated in eight sessions (45 min, twice a week) to receive MCT interventions. The content of the sessions was based on the Wells guideline (23) about anxiety disorders and all individual therapies were implemented on the participants. The sessions were held in the conference center of Valiasr Hospital. The contents of the sessions are summarized in Table 1.
| Resilience Skills Training | MCT | |
|---|---|---|
| First and second sessions | Orientation, goal statement, rules, concepts of resilience, self-confidence, self-reliance, self-awareness and its elements, techniques to identify the strengths and weaknesses, the importance of self-confidence in the life, and methods to improve it | Orientation, goal statement, rules, introducing anxiety, symptoms, MCT and metacognition, the relationship between metacognitive beliefs, social metacognitive patterns and detached mindfulness. The participants helped in codifying their own personal case formulation. |
| Third and fourth sessions | The concept of anxiety, ways to control and cope it, the concept of anger, causes and outcomes of anger, and methods to control and attenuate anger | Metacognitive beliefs about the uncontrollability of worries, loss of control in the face of excessive worries, and challenging them. To clarify contradictory and inefficient metacognitions, the participants were asked to discuss controlling worry or uncontrollability of worry. |
| Fifth and sixth sessions | The process of communication and proper relationship with colleagues and clients, problem-solving and implementation of problem-solving methods | The main objectives of MCT and decreasing negative beliefs about the risks of worry, verbal and non-verbal approaches to challenge metacognitions. |
| Seventh and eighths sessions | Decision-making, the right criteria, and predicting the outcomes of decisions. | Positive beliefs about challenged worries and approaches to modify them. |
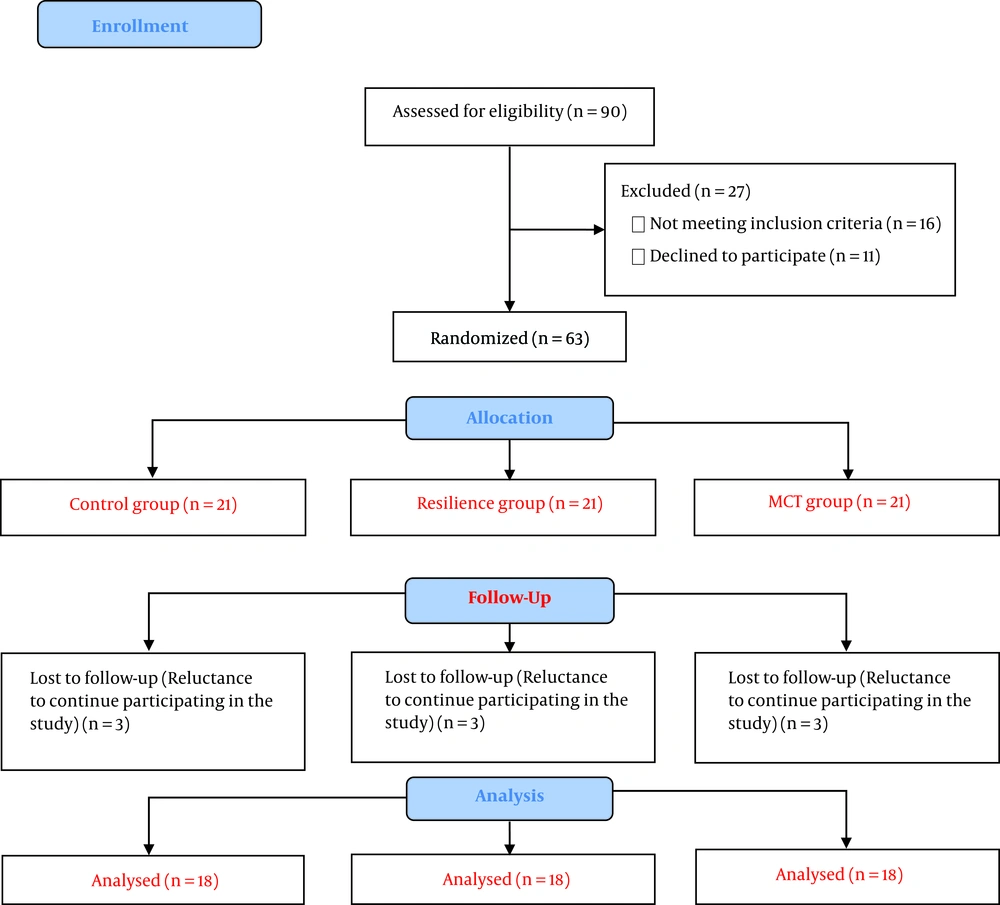
Both interventions included discussion, lecturing, problem-solving, and answering questions. For each skill, a pamphlet was prepared and presented to the participants. The content was based on a literature review and confirmed by six faculty board members of the Nursing School. Each session consisted of reviewing the previous session and teaching the next step. The sessions were summarized by asking questions from the participants. For each topic, a compensatory session was held in the same week so that the participants who failed to attend the session could catch up. The control group received no intervention. However, after completing the intervention, an educational package was presented to them. Immediately and one month after the intervention, the Spielberger anxiety inventory was filled out by the participants. The CONSORT flow diagram shows the flow of research (Figure 1).
3.3. Measures
The tools used in the study were a demographics form (age, gender, marital status, education, employment type, work shift, work experience, overtime work condition, and domicile) and the state-trait anxiety inventory (STAI).
The STAI was developed by Spielberger (2) to measure anxiety. This scale includes 40 items (20 items for trait anxiety and 20 items for state anxiety) graded on a Likert scale from one (never) to four (always). The total score ranges from 20 to 80 for each state and trait section. The higher the score, the higher the anxiety level (2, 24). The validity of the Persian version was confirmed by Aghamohamadi et al. (cited in Kalkhoran and Karimollahi article), and the test-retest reliability reported r = 0.97 (25). In the present study, Cronbach’s α coefficients for state and trait anxiety were 0.78 and 0.75, respectively.
3.4. Ethical Consideration
The study was approved by the Ethics Committee of Birjand University of Medical Sciences, Birjand, Iran (code: IR.BUMS.REC.1397.193). The study objectives and confidentiality of data management were explained to all participants and their informed consent was obtained.
3.5. Statistical Analysis
Data analyses were done in SPSS (V. 19). Before doing analyses, the normal distribution of the data was ensured using the Kolmogorov-Smirnov (KS) test, which supported the normal distribution of the data (P > 0.05). Repeated-measures ANOVA, Tukey’s post hoc test, ANOVA, Bonferonni test, chi-square test, and Fisher’s exact test were used for data analyses.
4. Results
Out of a total of 63 nurses participating in the study, three nurses were excluded from each group (reluctance to continue participating in the study), and finally, 54 nurses entered into the final analysis (18 participants in each group). There was no significant difference between the three groups in terms of demographic information (P > 0.05) (Table 2).
| Variable | Resilience | MCT | Control | P Value |
|---|---|---|---|---|
| Gender | 0.24b | |||
| Female | 16 (88.9) | 17 (94.4) | 13 (72.2) | |
| Male | 2 (11.1) | 1 (5.6) | 5 (27.8) | |
| Marital status | 0.54c | |||
| Single | 4 (22.2) | 5 (27.8) | 7 (38.8) | |
| Married | 14 (77.8) | 13 (72.2) | 11 (61.1) | |
| Education | 0.32b | |||
| Bachelor of nursing | 18 (100) | 16 (88.9) | 18 (100) | |
| Master of nursing | 0 (0) | 2 (11.1) | 0 (0) | |
| Work shift | 0.32b | |||
| Rotating | 18 (100) | 16 (88.9) | 18 (100) | |
| Fixed | 0 (0) | 2 (11.1) | 0 (0) | |
| Employment status | 0.12b | |||
| Permanent | 6 (33.3) | 6 (33.3) | 5 (27.8) | |
| Conditioned permanent | 12 (66.7) | 12 (66.7) | 9 (50) | |
| Short-term conditioned | 0 (0) | 0 (0) | 4 (22.2) | |
| Units | 0.30b | |||
| ED | 5 (27.8) | 7 (38.9) | 10 (55.6) | |
| PICU | 2 (11.1) | 2 (11.1) | 2 (11.1) | |
| ICU | 7 (38.9) | 5 (27.8) | 2 (11.1) | |
| NICU | 4 (22.2) | 4 (22.2) | 4 (22.2) | |
| Domicile | 0.93c | |||
| Personal house | 11 (91.1) | 10 (55.6) | 10 (55.6) | |
| Rental house | 7 (38.9) | 8 (44.4) | 8 (44.4) | |
| Age, y | 31.6 ± 5.4 | 31 ± 5.9 | 31.5 ± 6 | 0.94d |
| Work experience, y | 7.6 ± 5.4 | 7.2 ± 4.9 | 7.1 ± 5.1 | 0.95d |
aValues are expressed as mean ± SD or No. (%).
bFisher’s exact test.
cChi-square.
dOne-way ANOVA.
The repeated-measures ANOVA test showed a significant decrease in trait and state anxiety in the resilience group immediately and one month after the intervention (P < 0.001). However, there was no significant difference in the MCT group in terms of the mean score of trait anxiety (P = 0.17) and state anxiety (P = 0.37) at the three stages of the study.
The ANOVA test revealed that the mean score of trait anxiety immediately (P = 0.049) and one month (P = 0.01) after the intervention was significantly different between the three groups. Tukey’s post hoc test showed that the difference was significant between the resilience and control groups (P = 0.04). In addition, ANOVA showed that the mean score of state anxiety one month after the intervention was significantly different between the three groups (P = 0.04). Tukey’s post hoc test showed that the difference was significant between the resilience and control groups (P = 0.009) (Table 3).
| Variable | Group | Stage | |||
|---|---|---|---|---|---|
| Before Intervention (A) | Immediately After Intervention (B) | One Month After Intervention (C) | P Value of Repeated-Measures ANOVA | ||
| Trait anxiety | Resilience | 42.7 ± 8.7 | 35 ± 6.7A | 35.3 ± 6.2A | < 0.001 |
| MCT | 40.9 ± 9.1 | 37.9 ± 2.8 | 39 ± 6.2 | 0.17 | |
| Control | 40.9 ± 10 | 42.9 ± 3.5 | 42.7 ± 8.7 | 0.10 | |
| P value of ANVOA | 0.81 | 0.049 | 0.01 | ||
| State anxiety | Resilience | 43.2 ± 8.5 | 36.2 ± 6.7A | 36.4 ± 6.7A | < 0.001 |
| MCT | 40.4 ± 8.6 | 37.2 ± 10.2 | 38.6 ± 6.4 | 0.37 | |
| Control | 41.5 ± 12 | 42.5 ± 8.8 | 43.2 ± 9.8 | 0.21 | |
| P value of ANVOA | 0.69 | 0.07 | 0.04 | - | |
aValues are expressed as mean ± SD.
As listed in Table 4, there was a significant difference between the three groups in terms of the changes in the trait anxiety mean score before and immediately after the intervention (P < 0.001). Tukey’s post hoc test showed that the difference was significant between the resilience and control groups (P < 0.001) and between the MCT and control groups (P = 0.02). In addition, the changes in the trait anxiety mean score before and one month after the intervention in the resilience group were significantly higher than those in the MCT (P = 0.04) and control groups (P = 0.001).
The changes in the state anxiety mean score in the resilience group was significantly higher than those in the control group before and immediately after the intervention (P = 0.001) and between before and one month after the intervention (P = 0.005).
| Variable | Group | Stage | |||
|---|---|---|---|---|---|
| Resilience (A) | MCT (B) | Control (C) | P Value of ANOVA | ||
| Trait anxiety | Before and immediately after intervention | -7.6 ± 4.3C | -3.7 ± 6.1C | 1.3 ± 4.2 | < 0.001 |
| Before and one month after intervention | -7.3 ± 6.5B, C | -1.9 ± 9.3 | 1.7 ± 2.9 | 0.001 | |
| Immediately and one month after intervention | 0.2 ± 2.9 | 1.7 ± 8.9 | 0.3 ± 3.1 | 0.68 | |
| State anxiety | Before and immediately after intervention | -7.1 ± 5.7C | -3.2 ± 8.3 | 1.00 ± 5.02 | 0.002 |
| Before and one month after intervention | -6.8 ± 6.5C | -1.8 ± 11.9 | 1.6 ± 2.8 | 0.005 | |
| Immediately and one month after intervention | 0.2 ± 5.2 | 1.3 ± 8.8 | 0.6 ± 3.7 | 0.86 | |
aValues are expressed as mean ± SD.
5. Discussion
The effects of resilience skills training and MCT interventions were examined on the anxiety of nurses working in the ICUs and ED of Valiasr Hospital, Birjand, in 2018. The mean score of trait and state anxiety in the resilience group showed a significant decrease after the intervention. Magtibay et al. (13) supported the effectiveness of resilience and stress management programs in decreasing anxiety in nurses. Liu et al. (26), in a study, showed that the resilience and anxiety scores were significantly negatively correlated in obstetric nurses. In this regard, Wang et al. (27) argued that good adaptation ability can enhance the resilience score of nurses, especially the ability to deal with problems, and can reduce the degree of depression and anxiety. Inzlicht et al. (28) believe that resilient individuals can overcome the negative effects of physical and emotional fatigue caused by heavy work and preserve their mental health. Mealer et al. (29) assessed the effects of resilience training programs on anxiety, post-traumatic stress syndrome, and job burnout in ICU nurses. They reported that the resilience skills training program did not affect anxiety in the nurses (24). These inconsistent results can be explained based on different educational programs and periods of implementation.
To elaborate on the effect of resilience skills training on the alleviation of anxiety, the main elements of resilience (self-confidence, optimism, personal competency, trust in instincts, positive acceptance of change, control, and spiritual effects in the face of stressors) act as a shield and prevent the anxiety increase (30). Steinhardt and Dolbier (31) found that resilience improvement programs improved different factors like positive emotions, self-confidence, and self-leadership and attenuated negative emotions. Indeed, the capabilities rooted in resilience enable resilient individuals to manage the harsh and stressful conditions in life and the work environment. It is reasonable that resilience training can affect the attenuation of anxiety in ICU and ED nurses.
The results also showed that the change in the trait anxiety mean score immediately after the intervention compared to before the intervention was significantly lower in the MCT group than in the control group. Ashoori (21) conducted a study titled “The effects of group MCT on the alleviation of generalized anxiety symptoms and improvement of quality of life”, and showed that MCT significantly decreased the symptoms of generalized anxiety and improved the quality of lives of nurses. Wells and King (32) studied patients with generalized anxiety disorder and showed that MCT had a significant effect on anxiety symptoms. Sadeghi et al. (33) systematically assessed MCT and its effects on anxiety disorders and showed its efficiency in controlling psychological and anxiety problems. Normann and Morina (34) conducted a systematic assessment of MCT and its effect on anxiety and depression and showed that the intervention was efficient. These findings are consistent with the present study findings.
From the metacognitive viewpoint, anxiety is not a pathological outcome. But also is an active and motivated way to assess and deal with the threats caused by one’s beliefs. Anxiety disorders are the outcomes of metacognitive abnormal beliefs (35). Nordahl et al. (36) showed that metacognitive beliefs might be a basic mechanism of developing vulnerability to damages of trait anxiety. This could be due to that the metacognitive model informs the conceptualization of psychological vulnerability. They argued that MCT programs could improve psychological resilience and trait anxiety in individuals (36).
In terms of changes in the mean score of trait and state anxiety, the resilience group was significantly different from the MCT and control groups immediately and one month after the intervention. This difference indicates that the anxiety level decreases were higher in the resilience group than in other groups, and the resilience skills training was more efficient in alleviating anxiety in ICU and ED nurses. Contrary to this finding, the results of a study by Zamirinejad et al. (18) showed that after the intervention, there was no significant difference between the two groups of resilience training and MCT in depression scores. To explain this finding, it is notable that the efficiency of MCT depends on the length of the education course (37). In many cases, individuals face conflicts or even may resist during the early phases of MCT when they realize how abnormal have been their metacognitive beliefs. In addition, leaving inefficient metacognitive approaches might create anxiety. However, by practicing and self-observation, individuals can enjoy lower anxiety levels in long enough periods and have a better adaptation to their environment.
5.1. Conclusions
Taking into account the undeniable role of ICU and ED nurses in the provision of health and treatment services, the utilization of strategies to alleviate anxiety and remove the ground factors can have a notable effect on the efficiency of the health system and the quality of care. Given the results, resilience skills training was more effective than MCT both immediately and one month after the intervention. Nursing managers and policy-makers need to hold resilience skills training courses to alleviate the anxiety of nurses in the work environment.
5.2. Study Limitation
The research samples were selected from a single center. Therefore, the dissemination of information between the groups may have occurred. Additional research to compare the long-term effects of MCT and resilience skills training on anxiety or other psychological disorders may also be helpful, especially considering the issues of dissemination.