1. Background
Dysphagia is one of the most common morbidities after a wide range of diseases such as stroke, Parkinson’s disease, multiple sclerosis, amyotrophic lateral sclerosis, or traumatic brain injury (1). Swallowing disorder is also a common problem in the elderly due to physiological changes and age-related diseases in the elderly (2). Oropharyngeal dysphagia can lead to aspiration, malnutrition, dehydration, and negative impacts on the quality of life (QOL) (3-5). Patients with dysphagia have reported social and psychological consequences that affect their daily and personal lives, including feelings of anxiety, depression, reduced self-esteem, and social isolation (6).
Although traditional clinician-driven assessments such as videofluoroscopy and fiber optic endoscopic evaluation of swallowing are the gold standards for assessment of swallowing function, they do not consider the patients’ view about the problem (7). Thus, Multidimensional dysphagia assessment, including patient-based and objective instruments has been recommended for evaluating dysphagia (8). In recent years, researchers have attempted to create new tools such as self-report questionnaires to do a comprehensive self-assessment of dysphagia (9).
Several validated questionnaires have been developed to assess the quality of life in patients with dysphagia to date: the M.D. Anderson Dysphagia inventory (10), the Swallowing Quality of Life questionnaire (11), the eating assessment tool (EAT-10) (12) and the deglutition handicap index (13).
Silbergleit et al. (9), in 2012, created and validated the dysphagia handicap index (DHI). dysphagia handicap index (DHI) has several advantages over other quality of life assessment tools in dysphagia patients, including Easy completion by most patient populations, use clear sentences that indicate patients’ complaints and easy daily use to evaluate the effect of dysphagia on three physical, emotional and functional factors of quality of life of dysphagia patient. It is a relatively new self-administered questionnaire that includes 25 items (9). The DHI has been translated into several languages such as Arabic (14), Persian (15), Japanese (16), and Hebrew (17). Factor structure analysis is a statistical method for investigating variable relationships for complex concepts such as socioeconomic status, quality of life, or psychological scales. Quality of life is a multidimensional concept that is measured by the original three factors structure including physical, emotional, and functional of the instruments (3). The original version of the DHI identified three main factors as indicators for determining the effect of dysphagia on patients’ quality of life. The validity of the Persian version of the Dysphagia Handicap Index (DHI) has been evaluated in a study (15) but the factor analysis of the Persian version has not been investigated in any study. Also, its reliability is determined only in neurogenic oropharyngeal dysphagia (15). The P-DHI showed good internal consistency (Cronbach’s α = 0.88) and strong test-retest reliability (ICC = 0.98) (15).
2. Objectives
Thus the purposes of this study were to investigate the factor structure of the P-DHI and to assess its consistency and reliability in patients with a wide variety of oropharyngeal dysphagia.
3. Methods
3.1. Participants and Study Design
This study was approved by the Ethical Committee of Tehran University of Medical Sciences (code: 93/d/260/683). Before any examination, the informed consent form was completed by the patients to participate in this study. Patients were recruited from neurology and ear, nose, and throat clinics of Tehran University of Medical Sciences by convenient sampling. All patients with oropharyngeal dysphagia; either mechanical or neurogenic, were assessed by a speech-language pathologist using the Persian Northwestern dysphagia patient check sheet (P-NDPCS) to enter the study (18). The P-NDPCS is composed of 28 items and five medical histories, behavioral, gross motor function, oral motor evaluation, and evaluation of swallowing sections. The P-NDPCS showed good internal consistency (Cronbach’s α = 0.955) and strong test-retest reliability (ICC = 0.956) (18). Also, patients who understood written or spoken Persian were included. We used the Mini-Mental State examination (MMSE) test to evaluate cognitive abilities and we excluded patients with cognitive impairments (a score of < 23). The MMSE is a brief test to measure cognitive impairments, including memory, calculation, orientation, language, and attention (19). Finally, patients who met the inclusion criteria filled out P-DHI. To evaluate the test-retest reliability, the P-DHI was administered to 20 patients twice with an interval of 2 weeks.
In this study, The P-DHI was administered to 100 patients (47 men and 53 women) with oropharyngeal dysphagia. The mean age was 55.69 ± 15.04 years (range: 24 - 84 years), mean education level was 8.64 ± 4.92 years (range: 1 - 18 years), and mean disease duration was 14.07 ± 17.45 months (range: 1 - 120 months). Of the patients, 57% had neurological diseases (cerebrovascular diseases, Parkinson’s disease, amyotrophic lateral sclerosis, multiple sclerosis, and myasthenia gravis) and 43% had head and neck disorders (head and neck cancer, vocal fold paralysis and phono surgery). The distribution of the patients according to self-reported severity of dysphagia was as follows: normal (11%), mild (17%), moderate (60%), and severe (12%).
3.2. Persian Dysphagia Handicap Index
The P-DHI items are scored on a 3-point Likert scale (never = 0, sometimes = 2, and always = 4). Total score and subscales scores can range as follows: P-DHI total (25 items, 0 - 100), physical (9 items, 0 - 36), functional (9 items, 0 - 36), and emotional (7 items, 0 - 28), with lower scores indicating greater levels of QoL. At the end of the P-DHI scale there is a question about the severity of dysphagia, 1 as normal,2 and 3 as mild,4 and 5 as moderate, and finally 6 and 7 as severe (9).
3.3. Data Analysis
The factor structure of the P-DHI was investigated using Confirmatory Factor Analysis. To assess model fit, we used the chi-square statistic (χ2), relative/normed chi-square (χ2/df), the comparative fit index (CFI), the root mean square error of approximation (RMSEA), and the standardized root means square residual (SRMR). Typically, a non-significant chi-square value represents a good model fit. However, the chi-square statistic is highly sensitive to sample size. An alternative evaluation of the χ2 statistic is to examine the relative/normed chi-square (χ2/df) for the model. A χ2/df ratio of 3 or less is suggestive of a good model fit (20). Values greater than 0.90 for CFI and less than .08 for RMSEA indicate reasonably good fit (21), whereas SRMR should be below 0.10 (20). Cronbach’s alpha and ICC were used to examine internal consistency and test-retest reliability, respectively. A Cronbach’s alpha value of 0.7 - 0.8, 0.8 - 0.9, and > 0.9 are considered as acceptable, good, and excellent internal consistency, respectively (22). For ICC, values of < 0.5, 0.5 - 0.75, 0.75 - 0.9 and > 0.9 are considered as poor, moderate, good, and excellent reliability, respectively (23).
Moreover, the relationship between P-DHI and demographic/clinical characteristics was investigated using Pearson’s correlation coefficient, independent samples t-test, and one-way ANOVA followed by the Tukey post-hoc test. All statistical analyses were carried out using SPSS version 17.0 for windows, except for the CFA, which was conducted using Lisrel 8.80. The level of significance was set at 0.05, and all statistical tests were two-sided.
4. Results
4.1. Descriptive Statistics
The mean total P-DHI score and the subscales’ scores are presented in Table 1. According to scoring instruction, lower scores indicating better QoL. The mean total score was 33.93 ± 18.05. The lowest and highest scores were observed for Emotional (9.40 ± 5.75) and Physical (13.29 ± 7.12) subscales, respectively. The correlation coefficient between total score and its subscales were high, as well as between the subscales (ranging from 0.542 to 0.909, all P = 0.0001).
Abbreviation: SD, standard deviation.
aValues are expressed as mean ± SD.
bP < 0.001.
4.2. Reliability Analysis
For test-retest reliability, The P-DHI was readministered to 20 subjects of this study group one or two weeks later. The internal consistency (Cronbach’s alpha) of the P-DHI were as follows: Physical subscale (9 items, 0.751), Functional subscale (9 items, 0.836), Emotional subscale (7 items, 0.773), and the total score (25 items, 0.900). The test-retest reliability of the P-DHI in 20 patients using ICC was 0.984 for the total score, 0.952 for Physical 0.988 for Functional, 0.957 for the Emotional subscale (Table 2).
| Score | Number of Items | Reliability Analysis | |
|---|---|---|---|
| Alpha a | ICC b | ||
| Physical | 9 | 0.751 | 0.952 |
| Functional | 9 | 0.836 | 0.988 |
| Emotional | 7 | 0.773 | 0.957 |
| Total | 25 | 0.900 | 0.984 |
Abbreviation: ICC, intraclass correlation coefficient.
aCronbach’s alpha sample size, n = 100.
bICC sample size, n = 20; average test-retest interval = 14 days.
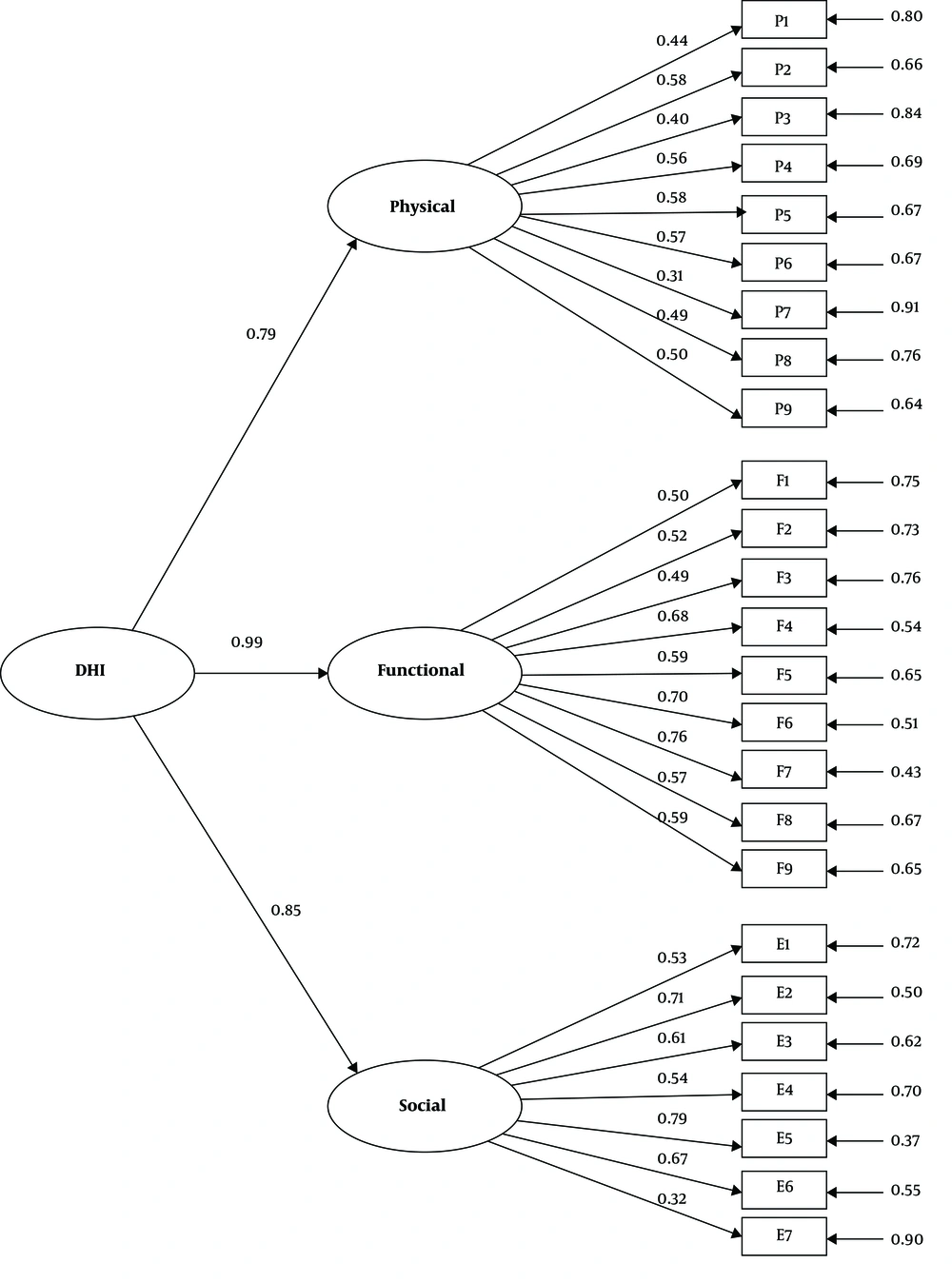
4.3. Confirmatory Factor Analysis
The CFA was undertaken to examine the fitness of the second-order three-factor model of the P-DHI. The fit indices indicated an acceptable fit of the data to the model (χ2 = 484.61, df = 273, P = 0.0001; χ2/df = 1.77; CFI = 0.901; RMSEA = 0.088 and SRMR = 0.010). As presented in Figure 1, all standardized factor loadings were significant and in the expected direction, ranging from 0.32 to 0.79.
4.4. Relationship of P-DHI with Demographic Characteristics
Table 3 shows the relationship between the demographic/clinical characteristics and P-DHI using univariate analysis. According to the correlation analysis, total P-DHI score were uncorrelated with age (r = 0.123, P = 0.223), level of education (r = -0.160, P = 0.113), and duration of disease (r = 0.154, P = 0.126). Scores also did not differ significantly by sex (P = 0.936). Regarding the self-reported severity of dysphagia, the total P-DHI score was significantly positively correlated with the severity of dysphagia (P< 0.001). Moreover, as presented in Table 3, the same results were obtained for Physical, Functional, and Emotional subscales.
| Physical | Functional | Emotional | DHI Total | |||||
|---|---|---|---|---|---|---|---|---|
| r Value | P Value | r Value | P Value | r Value | P Value | r Value | P Value | |
| Age | 0.123 | 0.221 | 0.104 | 0.304 | 0.089 | 0.378 | 0.123 | 0.223 |
| Level of education | -0.145 | 0.149 | -0.165 | 0.102 | -0.093 | 0.355 | -0.160 | 0.113 |
| Duration of disease | 0.154 | 0.125 | 0.097 | 0.339 | 0.159 | 0.114 | 0.154 | 0.126 |
| Sex | 0.837 | 0.926 | 0.895 | 0.936 | ||||
| Male | 13.45 ± 7.37 | 11.32 ± 7.93 | 9.32 ± 5.92 | 34.09 ± 18.89 | ||||
| Female | 13.15 ± 6.96 | 11.17 ± 8.05 | 9.47 ± 5.66 | 33.79 ± 17.46 | ||||
| Severity of disorder | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||
| Normal | 5.64 ± 1.96 | 4.00 ± 1.26 | 4.00 ± 2.19 | 13.64 ± 3.44 | ||||
| Mild | 9.24 ± 3.90 | 5.29 ± 3.60 | 5.18 ± 3.54 | 19.71 ± 6.04 | ||||
| Moderate | 13.57 ± 5.67 | 11.70 ± 6.09 | 9.70 ± 4.05 | 34.97 ± 10.95 | ||||
| Severe | 24.67 ± 5.74 | 24.00 ± 8.00 | 18.83 ± 5.75 | 67.50 ± 16.32 | ||||
| Type of disorders | 0.988 | 0.737 | 0.481 | 0.714 | ||||
| Neurological | 13.28 ± 6.96 | 11.47 ± 7.61 | 9.75 ± 5.11 | 34.51 ± 16.35 | ||||
| Head and neck | 13.30 ± 7.42 | 10.93 ± 8.47 | 8.93 ± 6.54 | 33.16 ± 20.27 | ||||
Abbreviations: SD, standard deviation; r, Pearson correlation coefficient.
aValues are expressed mean ± SD.
5. Discussion
The purpose of this study was to examine the factor structure and validation of the P-DHI in a sample of Iranian patients with oropharyngeal dysphagia. P-DHI is a dysphagia-specific instrument and opposed to similar generic measures, it only limits the factors affecting the quality of life to dysphagia and not the other stressful events. In the present study, the mean P-DHI score was which is higher than what was reported by Silbergleit et al. (9) and Farahat et al. (14). Moreover, the highest P-DHI subscales score (worst QoL) was observed for the Physical subscale. This finding is in agreement with the results reported by Silbergleit et al. (9), Farahat et al. (14), and Barzegar-Bafrooei et al. (15). It can be explained in this way that individuals with dysphagia are most familiar with their physical symptoms over the others and they tend to associate them with a swallowing disorder.
This is the first study, to the best of our knowledge, examining the factor structure of DHI by CFI. The second-order three-factor model of P-DHI was tested. In general, this model provided an acceptable fit to data and all standardized factor loadings were statistically significant.
The scale and its subscales showed acceptable to excellent internal consistency. This result is in line with previous investigations that have reported acceptable to excellent internal consistency for this scale (9, 14, 16). The scale and its subscales also showed excellent test-retest reliability, indicating that the scores of the P-DHI were stable after the two-week interval. This is in agreement with previous studies that have reported adequate test-retest reliability for DHI (9, 14-16).
There was a positive correlation between the overall P-DHI scores and severity of dysphagia scores; in other words, the higher the severity, the greater the DHI score. This is also in line with previous findings from Silbergleit et al. (9), Farahat et al. (14), Barzegar-Bafrooei et al. (15), Oda et al. (16) and Shapira-Galitz et al. (17). P-DHI score was not significantly related to age, sex, level of education, and duration of disease.
5.1. Limitations
It is plausible that some limitations could have influenced the results obtained. First, the sample size was relatively small given the wide confidence intervals thus the findings of the study should be interpreted with caution. Second, because there were no other tests in Persian to assess the quality of life in dysphagic patients, we could not measure the relationship between the scores of P-DHI and the scores of other tests, in other words, convergent validity has not been evaluated in this study. Finally, this study design was cross-sectional, thus it is not possible to conclude the nature of relationships between P-DHI and demographics or clinical variables.
5.2. Conclusions
In general, it can be concluded that 25 questions of the Persian version of the swallowing disability index, which are summarized in three physical, emotional, and functional factors, are related to each other by factor analysis method and can determine the effect of dysphagia on patients’ quality of life. Confirmatory factor analysis (CFA) revealed that the three-factor model of P-DHI demonstrated a superior fit to the data and the CFA findings provide additional support for the three-factor structure of the P-DHI and the use of the subscales as distinct variables. The Cronbach alpha values showed that P-DHI has good reliability. The results supported the notion that the P-DHI is a valid and reliable measurement instrument in predicting effects of dysphagia on quality of life and can be used as a tool that has good for clinical and research activities of dysphagia