1. Background
Temporomandibular disorders (TMD) are a group of pathologies of the temporomandibular joint, their muscles, and related structures. In fact, TMD is considered a musculoskeletal disorder of the masticatory system, and it has a 25% prevalence in overall population (1). In 3% - 7% of the population, pain and dysfunction leads to the need for treatment (2). The etiology of TMD is multifactorial (3). Risk factors include age (with some particularities), sex (female predominance), ethnicity (more common in Caucasians), parafunctional habits (tics, chewing gum), bruxism, hyperlaxity and malocclusion (2-5). Genetic factors seem to play no role in the prevalence of TMD, as observed in sibling cohort (4, 5).
The TMD is characterized by signs and symptoms that include pain, muscle tenderness, joint noises, and a limited range of motion (4, 6). The temporomandibular joint (TMJ) may be evaluated clinically and radiologically (7, 8). The normal distance of mouth opening is 53 - 58 mm (interincisal distance). A minimal limit of 40 mm might be used to identify patients with limited aperture, whereas 35 mm is the necessary criteria for diagnosing disc displacement without reduction after unforced maximal aperture (7).
The TMD was first described in 1934 by James Bray Costen, and he related TMD to dental apparatus and diverse symptoms such as headache, vertigo, plugged ear sensation, hearing loss, and trismus (1). Owing to all symptoms involved, a multidisciplinary approach is recommended for correct management (1, 2). The management of TMD conservative treatment includes: (A) occlusal splints; (B) physical therapy; (C) oral medication (NSAIDs and muscle relaxants); and (D) orthodontic treatment. Physical therapy is an important option used to reduce pain and inflammation and to improve oral mobility and function (1, 4). Effective Physical therapies for TMD include (1) therapeutic exercises; (2) manual therapy; and (3) electrophysical modalities. Finally, electrophysical modalities include: (A) Ultrasound (US), (B) iontophoresis, (C) phonophoresis, (D) microwaves, (E) low-level laser therapy, (F) pulsed electromagnetic fields, (G) transcutaneous electrical nerve stimulation (TENS), and (H) acupuncture (1, 2, 4, 9-14).
Ericson in 1961 used US for the first time for the management of TM disorders (15). Unfortunately, there are few studies published that report its real effectiveness on TMD (4, 12, 13, 15). Karamuri et al. (12) and Handa et al. (4) reported US as adjuvant therapy for pain control in TMD (4). In a survey of physical therapists, 54% reported they used US to deliver medication (phonophoresis) for soft tissue inflammation, 22% for pain management, and 19.8% for soft tissue swelling (15). Phonophoresis is the delivery of a drug through the skin into deeper tissue with the help of US (15). This technique is effective for the delivery of anti-inflammatory drugs for knee and other articulations (15); however, its use for the management of TMD is limited or absent. There is only one study that reported the effect of aceclofenac on TMD (16).
2. Objectives
The aim of this study was to evaluate the effect of US plus diclofenac gel 10% (phonophoresis) as a physical therapy available for the management of TMD based on pain amelioration and function recovery.
3. Methods
Trial design: This is a prospective quasi-experimental one-group before-after study. Neither blinding nor allocating a control group was regarded in this study.
3.1. Participants
Fifty patients with temporomandibular joint disorder (TMJD) were included in the study (Rehabilitation Department at Fundacion Hospital General Santisima Trinidad, Salamanca-Spain). The study was performed between June 2014 and December 2018.
3.2. Eligibility Criteria for Participants
3.2.1. Inclusion Criteria
1) patients 18 years or older; 2) derived from ear nose and throat, stomatology, dentistry, or familiar medicine specialists; 3) pain > 3 on Visual Analog scale (VAS); 4) failed pharmacological treatment (1, 4, 12, 14).
3.2.2. Exclusion Criteria
1) electrical stimulator or pacemaker; 2) diclofenac allergy; 3) cancer or any other severe or mental diseases; 4) osteoarthritis, inflammation, infection, or radiation on the TMJ articulation, 5) joint cement or plastic components on TMJ articulation (1, 4, 12, 14).
3.2.3. Settings and Location
Patients who attended to Rehabilitation Department, Fundacion Hospital General Santisima Trinidad were evaluated. Demographic data (sex and age) and medical antecedents (diseases, pacemakers, and electrical stimulator) were asked for. The Hospital approved the treatment protocol (Ethical Committee FHGST/02/2014). Written informed consent was given and signed before the treatment.
3.3. Outcome Measures
1) Pain (VAS); 2) mouth opening was measured by means of lip-to-lip distance as well as by means of interincisal distance in millimeters (mm), at baseline and after the treatment was completed.
3.4. Intervention
The patients were treated 20 sessions (1 session per day) of continuous ultrasound (SONOPULS 490 [Enraf Nonius® CE 0197] manufactured in Germany) to a dose of 1 W/cm2, 1 MHz for 5 minutes over the affected TMJ, with the help of ultrasound gel (5 mL) and 10% diclofenac gel (5 mL) in a proportion of 1:1 as transducer medium (evenly spread over the transducer head) (16).
3.5. Follow-Up
Review was performed at the beginning and at 20 days of the treatment to assess pain and mouth opening (lip-to-lip and interincisal distance). One-point change in VAS is considered a minimum clinically significant difference; three-point change is considered significant improvement (17, 18). A ruler graded from 0 to 10 cm was used to measure maximal mouth opening at lip-to-lip and interincisal distance (4).
3.6. Sample Size
A priori power calculation was based on the VAS scale with an effect size of 0.4, a 2 time-point of measurement (pre and post-test evaluation), a level of significance of 0.05, and the desired power of 0.8. With these parameters, a total of 46 patients were needed; allowing a dropout of 10% during the study, a total of 50 patients were finally included.
3.7. Statistical Analysis
For statistical analysis, SPSS® 20.0 package was used. Quantitative variables were presented as averages, while qualitative variables were presented as percentages and frequencies. A paired sample t-test was used to compare quantitative variables. A P value of less than 0.05 was considered statistically significant.
4. Results
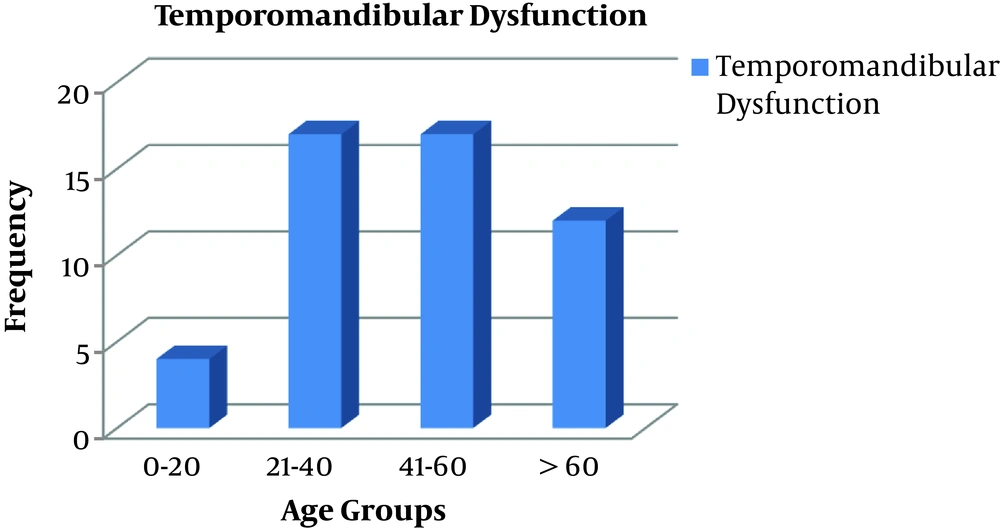
For this study, 50 patients with TMD (history of 6 months) were analyzed. Female patients (n = 41, 82%) were more common than males (n = 9; 12%), with a ratio female male of 4:1. The mean age of the sample was 47.22 ± 18.5 years (Table 1). The prevalence was more common at 21 - 40 years (n = 17, 34%) and at 41-60 years (n = 17, 34%), it was less frequent at group older than 60 years (n = 12, 24%) and at group younger than 20 years (n = 4, 8%) (Figure 1).
| Variable | Values |
|---|---|
| Female | 41 (82) |
| Male | 9 (18) |
| Age, y | 47.22 ± 18.48 |
| Time of disease, mo | 6 |
| Dropouts (due to severe events) | 0 |
| Number of sessions, d | 18.9 ± 4.59 |
| Mouth opening (lip-to-lip distance), mm | 50 ± 8.23 |
| Mouth opening (incisional distance), mm | 37 ± 7.2 |
| Pain VAS (0 - 10) | 6.67 ± 0.82 |
Abbreviations: d, days; mm, millimeters; mo, month; SD, standard deviation; VAS, Visual Analog scale; y, years.
aValues are expressed as mean ± SD or No. (%).
The protocol of phonophoresis (Ultrasounds plus diclofenac gel 10%) was prescribed at a mean of 18.9 ± 4.59 sessions (Table 1). Phonophoresis protocol was able to improve all outcome measures with statistical differences. Pain evaluated by VAS was 6.67 ± 0.82 and decreased to 3.48 ± 0.8 points (P = 0.0000). Mouth opening at a lip-to-lip distance was 50 ± 8.23 mm and improved to 56 ± 6.2 mm (P = 0.0000). Mouth opening at an interincisal distance was 37.9 ± 7.02 mm and increased to 44 ± 5.5 mm (P = 0.0000) (Table 2). No adverse events were observed during the study, and there were no dropouts because of them (Table 1).
| Outcome Variables | Before | After | P value |
|---|---|---|---|
| Lip-to-lip distance, mm | 50 ± 8.23 | 56 ± 5.47 | 0.000 |
| Incisional distance, mm | 37.9 ± 7.02 | 44 ± 5.5 | 0.000 |
| Pain VAS (0 - 10) | 6.67 ± 0.82 | 3.48 ± 0.75 | 0.000 |
Abbreviations: mm, millimeters, SD, standard deviation; VAS, Visual Analog scale.
aValues are expressed as mean ± SD.
5. Discussion
To the best of our knowledge, this is the first article that states that diclofenac phonophoresis is effective for the management of TMD in terms of pain relief and function recovery (mouth opening). No article had already defined the effectiveness of diclofenac phonophoresis on pain management and function recovery on TMD.
Phonophoresis is a physical therapy modality that favors the absorption of topical drugs and increases the concentration of the drug at the target region (16). Previous reviews have suggested that an effective drug into the TMJ could result in alleviating TMD symptoms. In phonophoresis, the US increases skin permeability because of chemical, thermal, and mechanical US properties. Deep heat (thermal US effect) causes local vasodilatation, which increases cell permeability and pain relief. Moreover, acoustic pressure waves (non-thermal US effect) causes the cells to oscillate at high speed (vibration) and to disrupt the membrane favoring the diffusion of the anti-inflammatory drug (diclofenac) (16). We postulate that the anti-inflammatory effect of diclofenac plus the biological effect of US (19) are capable of ameliorating TMD symptoms, a fact that has been demonstrated in this study.
The findings of this study come in line with a report from Deniz et al. (20) who observed that diclofenac gel phonophoresis (in continuous or pulsed US mode) could decrease pain and to improve functional status in knee osteoarthritis, and the benefit was more notable if compared with topical diclofenac gel application. This suggests that the delivery of the drug plus the biological effects of the US are responsible for these achievements (20).
In our study, diclofenac was applied in the form of gel formulation, not in a cream formulation. The reason for this was that in a previous article, Coskun Benlidayi et al. (21) stated that the gel-formulation is very similar to the US gel used as coupling media in diagnostic and therapeutic US. That is because the gel preparation has a higher acoustic transmission ability than the cream preparation (21).
Rai et al. (22) and Mishra et al. (23) have stated that no single treatment is more effective than any other for the management of TMJD. However, they state that any treatment modality (US, LASER, short-wave diathermy, and pulsed short-wave diathermy) is better than placebo. In Rai’s article, it is stated that the US must be used as an adjunct to other therapies (oral splints, heat, acupuncture, or muscle conditioning exercises) (22). Mishra stated that since any single treatment is not better than the others, treatment depended on the expertise of the clinician, the clinical presentation, and the reduction of the risk factors (23). That was the reason to choose phonophoresis, our Rehabilitation Department uses that technique for decades, and we are expertise in the technique.
Our study confirms that TMD is more frequent on females (3) as it was stated by Rai et al. (ratio 2:1) (22), Knezevic et al. (ratio 2:1) (11), Poveda-Roda et al. (ratio 4:1) (2), and again Poveda-Roda et al. (ratio 6.2:1) (24). There is no clear explanation for the more common female prevalence in TMD based on differences in psychosocial, endocrine, constitutional, and behavioral factors (24). Poveda-Roda et al. (24) has suggested that the estrogen receptors in women would modulate the laxity of the ligaments. Estrogens would increase attention to pain stimuli by limbic activity at the central nervous system (2).
In the present study, age of presentation was more frequent in patients from 21 - 40 years (n = 17, 34%) and in patients from 41 - 60 years (n = 17; 34%). These findings are similar to those reported by Rai et al. (20 - 40 years) (3), Akadiri (early adulthood and middle age) (25), de la Torre Rodriguez (25 - 35 years) (26), Algozain Acosta et al. (22 - 59 years) (27) and by Adibi (bimodal peak at < 25 years and at 55 - 60 years) (5).
In the present study, the US treatment protocol dose was set at 1 W/cm2/1 MHz/5 minutes/every day until 20 sessions of treatment were completed. This is in accordance with the dose proposed by Rai et al. (22) (0.5 - 1 W/cm2/3 MHz/5 min duration) for anti-inflammatory effect. Rai et al. (22) stated that lower doses (0.1 - 0.6 W/cm2) should be used in acute states, whereas higher doses (0.3 - 0.8 W/cm2) must be used for chronic states. Rai et al. also suggested that higher frequencies (3 MHz) had to be used for superficial lesions (1 - 2 cm depth), while lower frequencies (1 MHz) had to be used for deeper injuries (3 - 5 cm depth).
The proposed protocol in our study ameliorated the pain and improved mouth opening that agree with those observed by Rai et al. (3), Ucar et al. (28), Arora et al. (29), Sata (30), and Singh e al. (31). All the referred studies reported an amelioration of pain and an improvement in mouth opening.
The only known study that evaluated phonophoresis with aceclofenac gel on TMD used a protocol similar to ours (1 MHz/0.8 - 1.5 W/cm2/10 minutes). In that study, a frequency of 1 MHz showed higher transport than 3 MHz on topical gel application (16). In the referred study, their similar protocol decreased pain both in males (from 7 to 2.1 points) and females (from 7.85 to 3.6 points) and improved mouth opening both in males (from 33.5 ± 8.4 to 39.7 ± 7.8 mm) and in females (from 29.2 ± 7.3 to 34.3 ± 8.8 mm) (16).
Deniz et al. (20) have stated that phonophoresis is one of many techniques useful for the treatment of musculoskeletal disorders, including tendinitis, tenosynovitis, knee osteoarthritis, and TMD. Phonophoresis intensifies the absorption of a topical agent (steroids, salicylates, anesthetics, acetic acid, and non-steroidal anti-inflammatory drugs [NSAIDs]) by the use of US (20). Deniz et al. (20) have demonstrated that diclofenac gel phonophoresis (either in continuous or pulsed US mode) is more effective than topical diclofenac gel application for the management of knee osteoarthritis (20). Pain and function improved significantly in the diclofenac gel phonophoresis group if compared to the topical group (20). Moreover, the topical diclofenac group was similar to the placebo group in terms of evaluation of pain at rest and activity (20). Diclofenac gel phonophoresis was superior to topical diclofenac gel and placebo (20).
Our findings and those reported by the studies from Vijayalakshmi et al. (16) (aceclofenac gel phonophoresis on TMD) and Deniz et al. (20) (diclofenac gel phonophoresis on knee osteoarthritis) came to similar conclusions that US plus diclofenac gel 10% is an effective and safe alternative for the management of TMD.
5.1. Limitation of the Study
An important limitation of the study is the absence of a control group. When an intervention is expected to get a clinical benefit, it is unethical to deny such an intervention. Therefore, in quasi-experimental studies, there is no control group, mainly because of ethical reasons. In that scenario, the change in a before-after study is expected to be the direct consequence of the intervention (phonophoresis of diclofenac). This design allowed us to evaluate the impact of a quasi-independent variable (phonophoresis) under naturally occurring conditions. Generally, the hypotheses were answered through this design (phonophoresis decreases pain and improves function in TMD) (32); however, neither the small sample-size nor the lack of control group influenced the results observed in the current study.
5.2. Conclusions
Diclofenac phonophoresis is an effective physical therapy for the management of TMD, evaluated by pain improvement and function recovery. Neither dropouts nor adverse effects have been observed in the present study.