1. Context
Unani medicine is one of the oldest traditional systems of medicine, which originates from the era of Hippocrates (460 - 377 BC). Unani medicine is based on the concept of four temperaments and four humours, proposed by Hippocrates, the father of Unani medicine. Unani medicine utilizes medicines of herbal, mineral, and animal origin but mostly herbal drugs for both therapeutic and preventive measures of the disease (1, 2). Unani specifically promotes the prevention of diseases by recommending certain drugs and regimens to empower immunity status and the general health of the body. History of the epidemic has taught ancient Unani physicians to encourage preventive measures during epidemics such as cleanliness and hygiene, isolation of sick patients, disposal of infective materials from the patients, and usage of prophylactic medicine and general tonics before and during infective seasons (3, 4). Tiryaq is specifically originated and designed by Unani scholars to achieve similar aims (5).
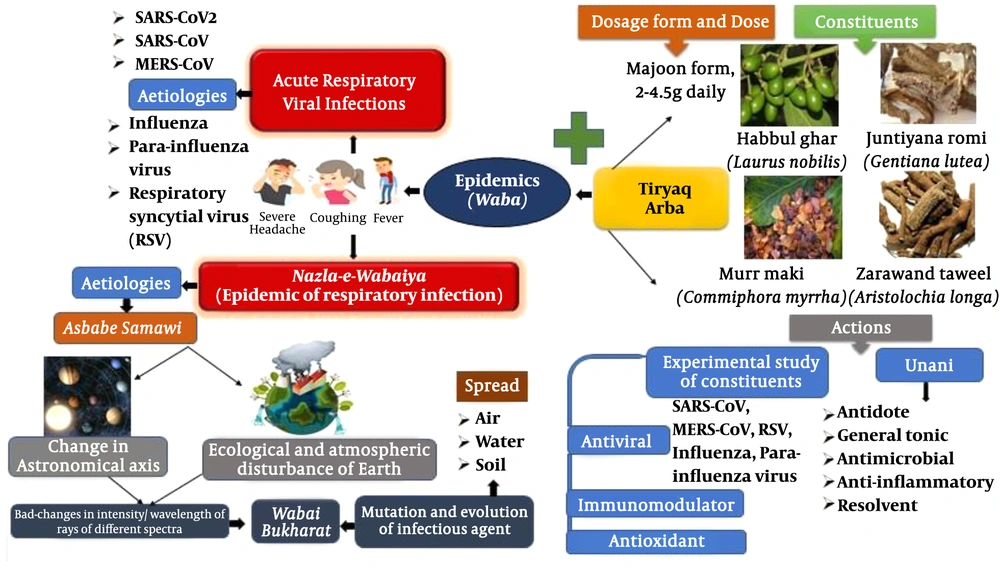
“Tiryaq Arba” is an age-old Unani formulation to be used by Unani physicians as a prophylactic medicine in epidemics since centuries. The name of this polyherbal formulation justifies its action and composition e.g., “Tiryaq” means “antidote” and “Arba” means four. The medicine has been used as an antidote for prophylactic measures against epidemics as well as an antidote against poisons. Since the medicine is composed of four types of herbal constituents, hence named “Tiryaq Arba”. Habbul ghar (Laurus nobilis) is the chief ingredient of this medicine. The other three are juntiyana romi (Gentiana lutea), murr maki (Commiphora myrrha), and zarawand taweel (Aristolochia longa). The medicine is available in a mixture form (powdered constituents are mixed with honey to achieve a semisolid consistency) to be taken at a dosage of 2 - 4.5 g daily (5)
Constituents of Tiryaq Arba have been substantiated for their antiviral efficacy against severe acute respiratory syndrome coronavirus (SARS-CoV), adenovirus and respiratory syncytial virus infections, parainfluenza virus, human rhinovirus B, and coxsackievirus, parainfluenza virus type 3, Newcastle disease virus, and influenza A virus (Figure 1) (6-19).
2. Evidence Acquisition
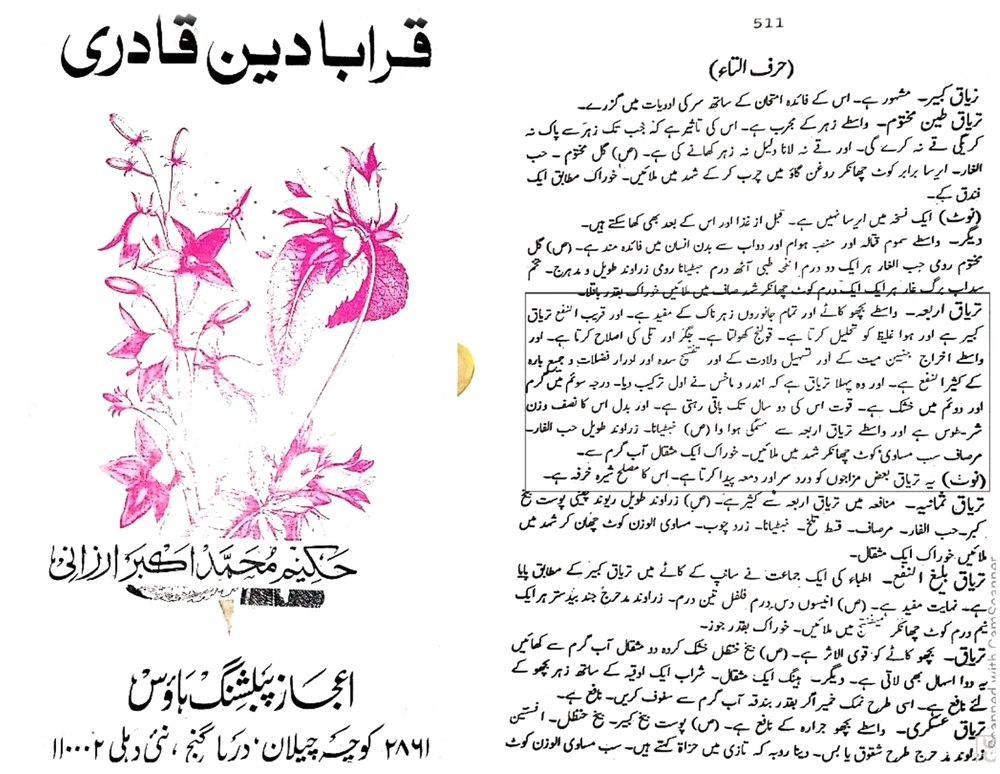
The MEDLINE®, Embase, Cochrane databases, and Health-organizations web-guideline were searched to review literature related to acute respiratory infections, coronaviruses illnesses and COVID-19 for all relevant articles written in English up to 20 March, 2020 (exclusive). We conducted a review of Urdu version of Unani literary books to search for a description of “Waba” or “Amraze waba” or “Nazl-e-wabaiya” (terminology), which was correlated with constellation of manifestation related to epidemics of acute respiratory infections. We further underlined and explored the concept of “Waba” and “Nazl-e-wabaiya” and its aetio-pathogenesis by utilizing certain Unani manuscripts e.g., “Al-qanoon fit tibb” (The canon of medicine), “Ikseere Azam”, and “Al-asbab wal ala’mat”. The literary review of “Tiryaq Arba” was performed using standard Unani pharmacopeial manuscripts such as “Qarabadeen Qadri”, “Qarabadeen najmul ghani”, “Al Qarabadeen”, and “Makhzanul mufradat maroof ba khawasul advia”. Above mentioned e-libraries and databases were also utilized to search experimental studies on constituents of “Tiryaq Arba” by searching through their common and botanical name for their antiviral, immunomodulatory, and antioxidant action.
3. Background and Current Scenario of Epidemics of Acute Respiratory Viral Infections
Hundreds of thousands of adults and children are sickened every winter by concurrent outbreaks of respiratory viruses. Acute respiratory viral infections (ARIs) are the leading cause of morbidity and mortality from infectious diseases in the world. Almost four million people die from ARIs each year, with 98% of these deaths due to lower respiratory tract infections (20).
Acute respiratory viral infections are the leading cause of morbidity and mortality from infectious diseases worldwide, especially affecting the younger and the elderly in low- and middle-income countries. These infections, typically caused by viruses [influenza virus, parainfluenza type 1 and 2, respiratory syncytial virus, Middle East respiratory syndrome related-coronavirus (MERS-CoV, SARS-CoV, novel coronavirus disease 2019 [COVID-19], etc.) or combined viral cum bacterial infections can spread rapidly and can be infectious. However, the mode of transmissions area constantly evolving, existing data suggest that droplet infections are the major mode of transmission in ARIs. But certain pathogens may also transmit via touch or infectious aerosols in specific circumstances (20, 21).
In modern medicine, interventions to prevent and monitor infection (IPC) in healthcare settings are of vital importance to patient safety, healthcare personnel, and the habitat, and to mitigate the risk of the infectious disease locally and worldwide. The management of ARIs is no exception to this. Since many ARI symptoms are frequent and non-specific, it can be difficult and confusing to apply IPC measures for ARIs in areas where healthcare resources are restricted. In these areas, screening procedures, early diagnosis, quarantine procedures, rapidly creating and placing patients in isolation, and proper aeration could be the steps to control and mitigate the spread of the infectious agent. These recommendations reflect an update to the interim guidance of the World Health Organization (WHO) infection prevention and control in health care of infectious and pandemic-prone acute respiratory diseases, 2007 (21, 22). They also provide emergency advice for confirmed, possible, or suspected pandemic cases (H1N) 2009 virus infection and influenza-like disease as provided by the WHO for prevention and control of infectious diseases in 2009 (21).
Commonly, respiratory viruses involve the mucosa of the respiratory tract (upper and lower). Influenza is commonly manifested by cold, cough, croup, bronchiolitis, and pneumonia. On the other hand, rhinovirus leads to the typical manifestation of common cold, while respiratory syncytial virus (RSV) mostly leads to bronchiolitis which may progress to ARDS (acute respiratory distress syndrome) (20, 21).
The extent of viral respiratory illness varies widely; in older patients and children, serious illness is more likely. Morbidity may result directly from a viral infection or maybe indirect due to exacerbation of underlying cardiopulmonary or lung conditions, paranasal sinus, or bacterial superinfection in the middle ear (21).
Mostly respiratory infections epidemics begin during October and peak till February. The normal trend for odd-numbered epidemiological years is for parainfluenza type 1 virus, which occurs during fall or at the beginning of October, followed by parainfluenza type 2. The later causes lower respiratory tract infection in fewer cases. Influenza virus starts January, and peaks in February while RSV starts during November and outbreak between December and January. In general, the type 3 parainfluenza virus accompanies the influenza epidemic and is widespread during November and February (20, 22).
Acute respiratory disease outbreaks are common and can occur in many settings (e.g., households, nursing homes, army barracks). It can require different treatments, infection prevention procedures and other preventive measures to manage outbreaks. Research into the clinical and epidemiological characteristics, as well as the etiology of outbreaks, is therefore specifically relevant to public health. To rule out emerging health risks, investigating serious unexplained respiratory outbreaks may be of particular importance (21, 22).
The etiology of many acute respiratory diseases can remain unknown, despite continuing efforts. Investigating unexplained respiratory outbreaks may classify infectious agents that involve specific control and prevention approaches (e.g., pulmonary hantavirus syndrome, SARS, COVID-19); however, are outbreak investigations for previously established etiologies are equally relevant. This mechanism can be improved by concrete efforts to Alert clinicians to recognize and record cases and clusters of unidentified infectious diseases. Prepare health departments for those clusters to be investigated (21, 22).
On 11 March 2020, the WHO announced the outbreak of COVID-19 as a pandemic and reinforced an appeal for countries to take urgent action and increase response to treat, diagnose and minimize spread to save lives for people (23). Coronaviruses (CoV) are a wide family of viruses which lead to diseases varying from cold or flu to more serious illnesses, such as SARS-CoV, MERS-CoV, and COVID-19. Pneumonia of an unknown origin found in Wuhan, China was first confirmed on novel coronavirus infection (nCoV) to the WHO Country Office in China on 31 December 2019. On 20 March 2020, there were 209,839 confirmed cases, 8,778 confirmed deaths in 169 countries, areas, or territories of the world (24). The virus is believed to spread mainly from one person to another. People who are in close contact within six feet and breathing in the air, coughed and sneezed by an infected individual in close contact. The droplets from an infected person may enter other people’s respiratory tract through the nose or mouth. Touching the infected surface and goods with the virus may transmit infections in some cases (25, 26).
The COVID-19 is a new strain that was identified in 2019 and not established in humans beforehand (24). A new coronavirus now called SARS-CoV-2 (the official name for the coronavirus that causes the COVID-19 disease) causes the COVID-19 pandemic. This coronavirus is closely related, but differs from the coronavirus that triggered the SARS outbreak in 2002 - 2003. Coronaviruses are zoonotic, which means that they are spread between animals and humans. Coronaviruses are prevalent and account for up to 25% of “common colds”. Certain coronaviruses, such as those responsible for SARS and MERS, contribute to much more severe diseases. Various species of bats serve as the natural host for coronaviruses, which break out as zoonotic epidemics periodically into human populations (27, 28).
Respiratory symptoms, fever, cough, shortness of breath, and trouble breathing are typical signs of infection. For more serious cases, pneumonia, extreme acute respiratory syndrome, kidney failure, and even death may result from infection. Although COVID-19 symptoms frequently mimic influenza symptoms, including fever and cough, COVID-19 tends to be even more infectious than flu and has a case fatality rate that can be up to 10 times higher than influenza. While the crude case fatality rate appears to be 3.96 percent, based solely on reported numbers of cases and deaths, the actual risk of COVID-19 death is unclear as testing for SARS-CoV-2 infection and supporting COVID-19 care varies widely around the world (25, 27). Actual death rates in South Korea are 0.9% and vary tremendously such as 7.3% in Italy. Although the reasons for these large differences are uncertain in case of fatality rates, what is apparent is that older age (particularly patients over 70 years of age) and underlying medical conditions, such as hypertension and cardiovascular and pulmonary diseases, significantly increase the risk of mortality. Conversely, unlike the 2009 H1N1 swine flu outbreak, rates of a symptomatic infection, and as a result, a serious disease in children and adolescents are substantially lower with COVID-19 compared with older adults (27, 28).
A total of 195 COVID-19 cases (163 Indians and 32 foreign nationals) were registered in 20 States/Union territories of India as of 20 March 2020 (9:00 AM). These included 19 people who were cured/discharged, one person who migrated, and four deaths were reported. Hospital isolation of the contacts from all reported incidents, tracing and home quarantine are continuing (23).
The preventive strategy is the same as any of the respiratory viral infections like influenza, including social distance, regular hand washing, and avoiding touching eyes, nose, and mouth. Those who have had close contact with a person with confirmed COVID-19 will have 14 days of self-quarantine (the average duration of incubation is 5 - 7 days, but some cases occurred as long as 12 - 14 days after exposure) (27).
4. Background of Epidemics in Unani Medicine
Unani theoretical framework conceptualized that human health is based upon the homeostasis of the four humours and temperaments in association/under the influence of six essential factors. Disturbance in the normal routine of six essential factors such as (1) air, (2) food, (3) sleep and awareness, (4) physical activity and repose, (5) mental awareness and repose, and (6) elimination and retention which disturbs genetic homeostasis of the humours for a person viz a viz production of morbid humours. These morbid humours are the root cause of pathology produced in the body (3, 4).
Unani medicine affirms that the occurence of infectious diseases requires three factors (1) infectious agent; (2) vulnerability in the human body; and (3) environmental conditions (4). Epidemics are greatly discussed in the Unani literature. Unani scholars suggest that the spread of epidemics occurs via infected air, water, and soil or altogether. The air may also change/epidemics are exacerbated due to disturbance in the natural balance of the earth or could be due to global warming. Unani scholars proclaimed that certain areas of the earth have changes in intensity/ wavelength of rays which have a negative impact on the air of that area. The old air near the soil generally gets purified with healthy rays becomes infected due to bad changes in the rays. These infected vapors may cause the growth and mutation of an infectious agent. Unani scholars also documented that bad disposal of refuse/waste, collection of water, and bad community hygiene promotes the development and spread of epidemics. These could be the plausible reason for the rise of epidemics/pandemics in this era. Reputed scholar of Unani medicine, Ibne Sina (Avicenna, 930 - 1037 AD) documented in “Al-qanoon Fit Tibb” that certain qualitative changes occur in the air during epidemics. Lack of diagnostic methods of identifying infectious agents during that era led Ibn Sina to call those changes as the presence of infected vapors in the air which is a broad term to denote the presence of many elements in the air of epidemic area including the infectious agent. Ibne Sina proclaimed that hotness and humidity promote the growth of infectious agents and the spread of epidemics. He also stated in the book “Al-Qanoon fit Tibb” (The canon of medicine) that those epidemics which occur during the spring season are worst in nature (pathology/severity/spread). His statement on the spread of epidemics via air suggests that core-changes such as the presence of infectious agents occurs in the air of that epidemic area (3, 4, 29).
Epidemiological studies confirm that only a certain proportion of the population is highly sensitive to acquire infections. The development of diseases after acquittance with viruses, bacteria, and other microbes requires vulnerability in the human body to develop a particular disease. Genetic and racial predisposition, habits, nutritional, and immune status make a person liable to a particular infection. Ibne Sina proclaimed that vulnerability of an infection increases in those individuals who have weak constitution/immunity/general condition or presence of an excess of morbid humours in the body or if body pore/body constitution is open/ample welcoming to outside influences/elements along with the dominance of moistness (3, 4, 29).
The assessment of Unani literature revealed that ancient physicians were aware of the features of epidemics and documented their preventive measures and remedies. They also reported certain rapidly spreading deadly-infectious diseases. The severity of epidemics depends on the type of infectious agents. Unani scholars mentioned that multisystem involvement and serious symptoms in epidemics suggest the acute and severe nature of the infectious agent (3, 4, 29).
The major clinical features of epidemics mentioned in Unani literature are the feeling of more or less suffocation in the air with visibility of heavy particles or smog. Flies and mosquitos are increased. The normal duration of weather is increased or decreased with the presence of clouds (3, 4, 29).
In infected individuals, the following features are generally observed; the bad strong smell in body wastes, including air breathed out/expired air. Many people suffer from fever simultaneously because of breathing in the same epidemic air, sharing of the same food articles, and touching objects. Breathing and pulse are rapid. Even though fever lessens, the patient feels extreme weakness and irritability. Headache, vomiting, and semi/un-consciousness may occur with infectious fevers (3, 4, 29).
In the Unani literature, the clinical manifestation of “nazle-e-wabaiya” (an epidemic form of respiratory infection) simulates the clinical manifestation of ARIs, which spreads in an epidemic form such as influenza virus, parainfluenza type 1 and 2, respiratory syncytial virus, MERS-CoV, SARS-CoV, SARS-CoV-2, etc. Owing to in-advancement in diagnostic methods in the ancient era, Unani scholars were not able to observe and differentiate those infectious agents, but they were aware of their presence and entitled them with the entity “wabai bukharat”. The clinical features of nazla-e-wabaiya, mentioned in the Unani literature are fever, coughing, sneezing, sore throat, nasal congestion, headache, chest pain, anxiety, diarrhea, general weakness, and delirium. The Unani scholars also mentioned that the infection may complicate and progress to pneumonia (za’tul riya) and pleurisy (za’tul janab) in the elderly, children’s and patients of low immune status (3, 4, 29). These literary findings state that Unani scholar was well aware of the epidemic of ARIs. Thus, their therapeutic indices and management guidelines could be utilized as a tool to combat rapidly rising respiratory epidemics of current-era. The hypothesis “viruses are changing with the environmental conditions so does nature and their antiviral constituents” fits the current scenario of evolving-microbes and searching treatment options from plant-side. Plant-source drugs could be a hope to meet the challenges of drug-resistance due to mutated and ever-evolving viruses including MERS-CoV, SARS-CoV, SARS-CoV2, etc. Since secondary active-metabolites of the plants also change as per unfavorable environmental conditions of nature and earth, it could be the best solution in developing a treatment for such viruses (30).
5. “Tiryaq Arba” as Prophylactic Medicine in Unani Medicine Against Epidemics
5.1. Background of “Tiryaq Arba”
Unani literature suggests that Unani scholars were well experienced in diagnosing and managing epidemics. They promoted preventive measures such as personal hygiene, abstinence from travel, and isolation of the sick. Through their vast experiences, they utilized various herbs to be used as prophylactic medicine during epidemics. They have used these single and compound Unani medicine in healthy as well as sick individuals before or during epidemics and observed beneficial results. They formulated certain preparation known as “tiryaq” means “antidote” to be used against toxins and as prophylactic medicine. “Tiryaq Arba” is one of the compound formulations to be used extensively in Unani medicine until now. It is named “arba” because of the presence of four constituents in it (5). It is the first and oldest tiryaq prepared by Unani scholar, “Indru makhiz” (Figure 2). The popularity of “Tiryaq Arba” rises in the current scenario of epidemics where it can be utilized as prophylactic medicine. Hakim Azam Khan outlined anti-inflammatory, anti-flatulent, resolvent, and antidote properties of Tiryaq Arba. The above-mentioned properties led to its usage in epidemics such as cholera, plague, respiratory infections, etc. Unani scholars including Hakim Ghulam Jeelani have proposed that Tiryaq Arba is a potent tonic to heart and brain, thus justified to be used in epidemics where chances of acute involvement of these systems are higher (5, 30).
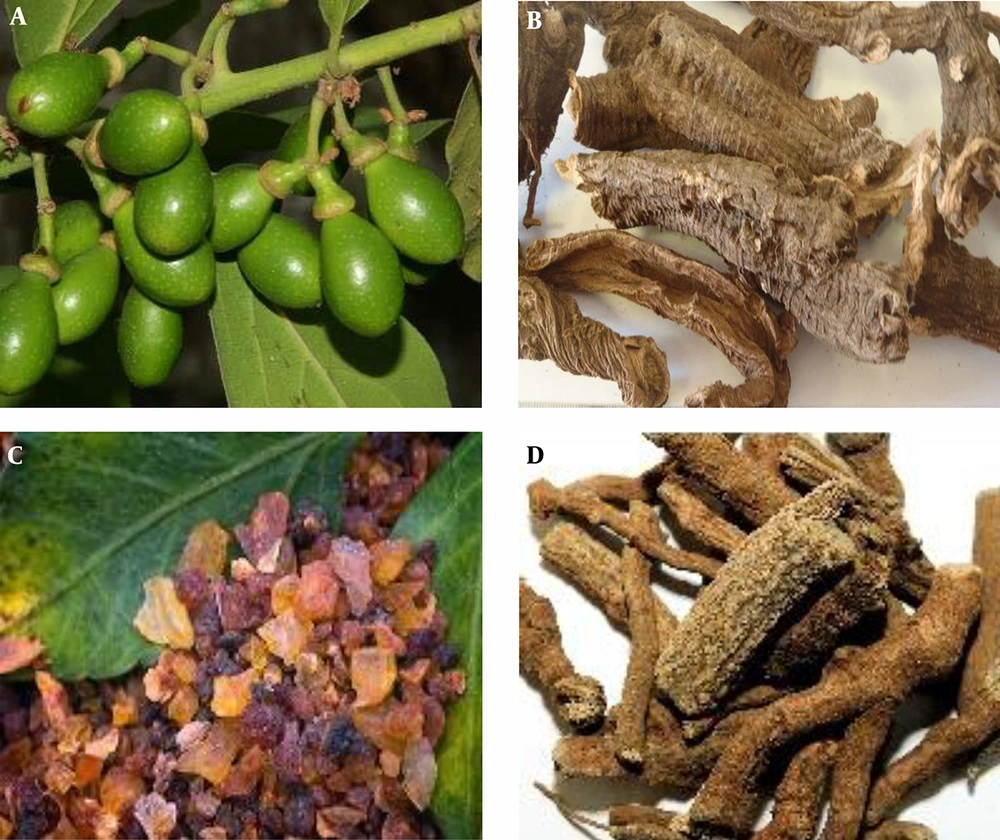
It is also known by the name of “tiryaq sagheer” as per the book “Bayaz Khas/ ilajul amraz” of Hakim Shareef Khan, translated by Hakeem Mohammad Kabiruddin (5, 30). Some people utilize qust talkh (Saussurea costus) in place of murr maki. Ibne Sina stated that some people utilize zarawand mudhiraj (Aristolochia indica) against zarawand taweel (Aristolchia longa). Some scholars add zafran (Crocus sativus) as an additional fifth constituent to add its efficiency (5, 30). Temperament of “Tiryaq Arba” is hot and dry (5, 30) and its constituents and their proportions have been shown in Table 1 and Figure 3 (5, 30, 31).
| Constituent (Unani Name) | Part Used and Botanical Name | Temperament | Actions | Proportion in Compound | References |
|---|---|---|---|---|---|
| Habbul ghar | Berry of Laurus nobilis | Hot and dry | Anti-inflammatory (muhalil); anti-tussive and anti-asthmatic; stomachic (muqawwiye maeda); emmenagogue (mudir haez); lithotriptic (mufattite hasat) | Equal | (5, 32, 33) |
| Juntiyana romi | Root of Gentiana lutea | Hot and dry | Antidote, antiseptic (tiryaq samoom); General tonic (Muqawwiye badan); stomachic (muqawwiye maeda); diuretic (mudir baul); emmenagogue (mudir haez); anti-flatulent (kasire riyah) | Equal | (5, 32, 33) |
| Murr maki | Oleogum resin of Commiphora Myrrha | Hot and dry | Anti-septic (da’fe taf’fun); desiccant (mujafif); expectorant (munaf’fis balgham); anti-inflammatory (muhalil); deobstruent (mufattih) | Equal | (5, 32, 33) |
| Zarawand taweel | Root of Aristolochia longa | Hot and dry | Anti-inflammatory (muhalil); deobstruent (mufattih); demulcent (mulat’tif); Expectorant (muqatiyye/mukhrije balgham); detergent (jali); analgesic (musakkin auja); emmenagogue (mudir haez); aphrodisiac (muqawwiye bah) | Equal | (5, 32, 33) |
Constituents of “Tiryaq Arba”
5.2. Method of Preparation of “Tiryaq Arba”
Habbul ghar, juntiyana romi, murr maki, and zarawand taweel cleaned, chopped, sieved, and powdered in equal quantity. All these powders are made greasy/roasted with ghee and mixed in 3 times volume of (5, 30). The consistency for mixture is of two tar. Tiryaq Arba is also prepared under a similar line for preparation of mixture where honey or sugar is utilized as a base and simmered at optimized flamed until two tar-consistency is obtained (32). Unani scholars advised using freshly prepared “Tiryaq Arba” after room temperature incubation of 40 days (5, 30).
5.3. The Dose of “Tiryaq Arba” and Expiration
Administration of 2 - 4.5 g with lukewarm water is generally advised. Unani scholars stated that the efficiency of “Tiryaq Arba” remains until two years. However, they have not mentioned the temperature and condition of storage where it can be stored up to 2 years (5, 30).
5.4. Actions and Indications of Usage of “Tiryaq Arba”
Unani scholars, including Ibne Sina and Akbar Arzani advised its usage in a variety of conditions such as a toxic bite from a snake, scorpion, spider, and other poisonous inmates, epilepsy, paralysis, and diseases where the predominance of coldness and phlegmatic humour exists. It also improves the functions of the liver and spleen. It is also used as abortifacient and helps in the delivery of a child. It is also used in intestinal obstruction (5, 30). The following actions of Tiryaq Arba are mentioned in Unani literature such as antidote, deobstruent, antispasmodic, diuretic. Murr maki (Commiphora myrrha) is said to relieve palpitation (30).
5.5. Adverse Effects and Corrective
The headache could be the side effect of using Tiryaq Arba. Purslane Seeds is mentioned as corrective to its side effects (5, 30).
6. Scientific Studies
Table 2 represents a summary of scientific studies on the constituents of “Tiryaq Arba” against respiratory viruses (Table 2).
| S. Number | Ingredients (Unani Name) | Botanical Name | Antiviral Against Respiratory Viruses | Immunomodulatory Activity | Antioxidants Activity |
|---|---|---|---|---|---|
| 1. | Habbul ghar | Berry of Laurus nobilis | Loizzo et al. (6), reported strong antiviral activity against severe acute respiratory syndrome coronavirus (SARS-CoV) among seven plants. Oil showed antiviral activity against SARS-CoV (SI; TC50/IC50) of 4.2 and IC50 value of 120 mg/mL. | Yerou et al. (8), reported essential oil increased white blood cell count, in vivo. | Kaurinovic et al. (7), reported ethyl acetate extract exhibited the largest free radical scavenging activity against DPPH, NO, O2- and OH radicals, in vitro. Protective effect against GSH, GSHPx, LPx, Px, CAT and XOD (lipid peroxidation), in vivo (7, 8). |
| 2. | Juntiyana romi | Root of Gentiana lutea | Sinupret®, polyherbal preparation, which contain Gentiana lutea as main ingredient has strong inhibitory activity against adenovirus and respiratory syncytial virus infections and influenza, influenza A virus, parainfluenza virus, human rhinovirus B, and coxsackievirus which causes acute respiratory infections by Glatthaar et al. (9). | Singh et al. (10) reported that extract significantly (P < 0.01) potentiated the humoural immune response in cyclophosphamide immunosuppressed mice at 100 and 200 mg/kg of each extract and fraction as compared to control. | Azman et al. (11), reported G. Lutea aqueous methanolic extract exhibited potent antioxidant property as scavenger in DPPH and Trolox equivalent capacity assay (TEAC) (15.89 and 48.90 µmol of TE/g DW, respectively). |
| 3. | Murr maki | Oleogum resin of Commiphora Myrrha | Cenci et al. (15), (2012) reported that methanolic extract of myrrh resin of 61% (w/w), exhibited antiviral activity against parainfluenza virus type 3 in HEp-2 cells plaque forming units (PFU) reduction assay. Bakri et al. (13), reported that resin-extract has reduced Newcastle disease virus titres significantly (P < 0.001), while chicken embryos treated with resins at a dose of 500 µg/mL had been negative for virus in the allantoic fluid. Ahmad et al. (14), also reported high antiviral activity against Newcastle disease virus. | Ashry et al. (16), reported immune-potentiating activity of extract by benefitting humoural immune system. Administration of extract 100 mg/kg b.wt. for 2 months before and concurrently with lead administration favorably protects the immune system against lead toxicity. | In both DPPH scavenging and Fe2+ chelating assays, the extract exhibited the highest free radical scavenging activity compared to oil. |
| 4. | Zarawand taweel | Root of Aristolochia longa | Idriss et al. (17), reported that extract inhibited influenza A virus infection by interacting with the viral hemagglutinin, affect nuclear transport of viral nucleoprotein (NP) and inhibit both viral attachment and replication. | Benzakaur et al. (18), reported a high number of lymphocytes in the different organs after extract administration in vivo, which indicated that it was an immune system activity. | El-Omari et al. (19), reported that extract showed maximum antioxidant action in DPPH (IC50 = 125.40 ± 2.40 µg/mL) and ABTS assay IC50 = 65.23 ± 2.49 µg/mL) (19). |
Components of “Tiryaq Arba” and Antiviral Mechanism of its components Against Respiratory Viruses
7. Discussion
The epidemics of acute respiratory viral infections are caused by viruses such as influenza, parainfluenza, SARS-CoV, MERS-CoV, SARS-CoV-2, etc., which are highly contagious, rapidly spreading and showed higher mortality and morbidity of all infectious diseases around the world. Earlier epidemics of influenza, SARS, H1N1, and recently COVID-19 were associated with symptoms of common cold, bronchiolitis, croup, pneumonia, etc. They generally spread through droplet infections, aerosols, and touch. The world health organization (WHO) declared a pandemic of COVID-19 on 11 March 2020. The WHO data reported 209,839 confirmed cases, 8,778 confirmed deaths in 169 countries on 20 March 2020 (until 9:00 AM). Currently, there is no approved treatment or vaccine for the same. Unani medicine is one of the oldest traditional system of medicine, which has documented many mild to deadly epidemics and also put forward the concept of preventive and therapeutic strategy during and/or before seasons of epidemics. Preventive strategies similar to the modern world such as isolation of sick, abstinence from travel, and maintenance of personal, social, and community hygiene have been documented in Unani literature for the management of before or during epidemics.
Unani medicine claims that the spread of epidemics occurs through the air, water, and soil or altogether. Unani medicine affirms that interaction with an infectious agent and the development of disease requires individual vulnerability to it. Considering these facts, Unani scholars developed certain Unani polyherbal formulation to be used before and/or during epidemics in both sick and vulnerable populations as prophylactic medicine. “Tiryaq Arba” is one of the semisolid compound Unani formulation, which has been specifically designed as an antidote (“Tiryaq” means antidote) to various poisons and infectious agents of epidemics. It is a sweet and semi-solid mixture that has been prepared by mixed all the four constituents in equal quantity and mixed three-times volume of honey in a final consistency of two tar, which is hot and dry at level 2 in temperament.
Unani scholars have been using this medicine in epidemics of cold/respiratory illnesses and observed beneficial effects. Scientific studies have also evidenced that constituents of “Tiryaq Arba” have antiviral activity against acute respiratory viruses such as SARS-CoV, adenovirus and respiratory syncytial virus infections and influenza, influenza A virus, parainfluenza virus, human rhinovirus B, and coxsackievirus, parainfluenza virus type 3, Newcastle disease virus, influenza A virus, etc. Besides, Unani scholars have proposed that “Tiryaq Arba” is an excellent medicine to be used in epidemics since it is a tonic/protective to brain and heart. It works as a potent anti-inflammatory, resolvent, and antidote in acute respiratory infections. It is advised to be taken at a dosage of 2 - 4.5 g with lukewarm water during and/or before epidemic seasons. Recently, the Central Council for Research in Unani Medicine (CCRUM), Ministry of AYUSH, Government of India has also included this formulation in the management guideline related to COVID-19, especially laid down for Unani practitioners. The CCRUM in their guidelines and We authors, do not claim for “Tiryaq Arba” effectiveness in COVID-19 since no systematic scientific data is available in this regard. However, this formulation could be a potential candidate to underline and explore its effectiveness in the management of COVID-19 as a prophylactic and or therapeutic medicine.
8. Conclusions
Unani physicians were aware of the concept of epidemics related to respiratory infections. Therefore, they formulated certain Unani preparations such as “Tiryaq Arba” to prevent and manage a rapidly contagious form of respiratory infections. Constituents of “Tiryaq Arba” have substantiated for their effectiveness against respiratory viruses, which spread in epidemic form, besides of its immunomodulatory and antioxidant potential. Even though with these enormous benefits of “Tiryaq Arba”, plausibly needed in the current situation of COVID-19, this Unani medicine lacks limelight and scientific experimentation and should be researched for its benefits in managing epidemics of acute respiratory viral infections for the greater good of the society and mankind.