1. Background
Low-back pain (LBP) is a significant public health problem in the world (1). It is associated with impairments and disability (2), such as spinal flexibility (3). Therefore, it is necessary to develop the spinal range of motion (ROM) in LBP to know the extent of impairment (4), prognosis, and disability (5, 6). Similarly, predictive tools such as the STarT back tool (SBT) were developed as valid predictors of disability to aid stratification of patients with LBP according to their future risk of physical disability (7). Specifically, the SBT uses the Biopsychosocial approach and helps the subgroup of patients with non-specific LBP into low, medium, or high risk of developing a physical disability. Accordingly, the patients are assigned to different treatments to suit their peculiar needs based on intensities (8).
There is still contention on the adequacy of patients’ self-reports of disability in clinical evaluation without the objective tests of physical performance (9). The relationship between traditional physical performance tests and prediction tools such as the SBT in ascertaining disability risks remains unexplored (10).
2. Objectives
This study assessed the convergent validity of SBT to predict the risk of future physical disability via spinal flexibility ROM among patients with LBP.
3. Methods
The Ethics and Research Committee of the Obafemi Awolowo University Teaching Hospital Complex, Ile-Ife, Nigeria, approved this correlational study (IRB/IEC/0004553). Thirty (male 14, female 16) patients with LBP signed the informed consent. They were clinically diagnosed with non-specific LBP, without radiating pain to the lower extremities, and had X-rays of the spine as recommended and screened by the physician. We excluded the pregnant women, those who had prior surgery to the lumbosacral region, and those with neurological deficits (muscle weakness or paresthesia) in the lower limb.
3.1. Instrument
In this study, we used STarT back tool (SBT) to assess disability risks. It contains nine items related to physical and psychosocial factors found as strong independent predictors for disability (8). The first four items assess leg pain, disability, and comorbid shoulder or neck pain, while the remaining five items create a psychosocial subscale, which assesses bothersomeness, pain catastrophizing, fear, anxiety, and depression. The summation of all positive responses gives the overall SBT scores (range 0 - 9). The total score is categorized as low (scores of 3 or less), medium (score of 4), and high (scores 5 or above) risks. Patients were classified as having the high risk of poor prognosis (means to have high levels of psychosocial prognostic factors with or without the physical factors present), medium risk (means to have physical and psychosocial factors, but not a high level of psychosocial factors), and low risk (means to have few physical or psychosocial prognostic factors) (8). Despite the emergence of SBT studies, a systematic review shows concurrent validity scores ranging from 0.34 - 0.802, discriminant validity score ranging from 0.69 - 0.92, and convergent validity score of 0.708 - 0.811, respectively (11).
The Verbal Rating Scale - This tool was used to assess pain intensity. It contains words describing the degrees of pain intensity. The general words are no pain (0), mild pain (1), moderate pain (2), and severe pain (3) (12).
Inclinometer: Dual inclinometer was used to assess spinal ROM. The first inclinometer was placed on the T12 vertebrae, and the second one was put on the S1 vertebrae. With the patient in a relaxed and upright position, the readings were taken respectively with the inclinometers. The patient was then asked to do the required movement (forward flexion, backward extension, or lateral flexion) to the full possible range. The upper inclinometer reading measures gross motion, and the lower inclinometer represents pelvic or hip motion. The difference between the two measurements is the lumbar motion reading (13).
Height and weight were assessed using a height meter (model RGZ480) and weighing scale (model ISO 9001:2000 Mod BR9011) following the standard procedures.
3.2. Procedure
Forward flexion and extension measurement: These measures were assessed in erect standing posture. The spinous processes of the T12 and S1 vertebrae were palpated. Then, the proximal arm of the inclinometer was placed on the skin overlying the spinous process of T12, and the distal arm was placed on the spinous process of the S1 vertebra. The readings were then respectively measured and noted in regular standing, forward bending (flexion), and back bending (extension) (4).
Lateral flexion measurement: The inclinometers were positioned on surface anatomy corresponding to the prominence of S1 and T12 vertebrae spinous processes on a straight line. Holding the two inclinometers upside down and against the back so that the gravity swings the pendulum freely. We asked the participants to stand erect facing the wall with maximum closeness possible to keep them from bending forward during lateral flexion measurements. After that, we asked them to laterally flex to the right and touch their right knee with their right hand. The readings from the two inclinometers were noted. The difference between the T12 and the S1 inclinometers gave the result of the true right lateral flexion value. The procedure was repeated for the left, denoting the left lateral flexion reading. The average value for the three consecutive readings made was the value noted for lumbar ROM (4).
3.3. Data Analysis
We used descriptive statistics to summarize data and Spearman correlation analysis, and Fisher's exact tests to analyze the association between the SBT scores/levels and spinal ROM scores/level. Also, we employed the box plot to depict the correlation between the dependent and independent variables. Analysis of Covariance was used to account for the contextual variables (gender, age, weight, height, body mass index, and pain severity). Statistical package for social sciences (version 20) IBM Corp. was used in the analysis. Alpha level was set at P < 0.05.
4. Results
The mean age of the participants was 46.33 ± 16.31 years (Table 1). The mean values for the forward flexion (FFlex), backward extension (BExt), left lateral flexion (LFlex), and right lateral flexion (RFlex) for the participants were 14.70 ± 11.16°, 31.63 ± 11.08°, 9.40 ± 5.36°, and 9.33 ± 6.47°, respectively (Table 1). The pain intensity was higher among males (3.42 ± 0.851 vs. 3.25 ± 0.85; P = 0.572).
| Variable | Male | Female | T-Cal | P-Value | All Participants |
|---|---|---|---|---|---|
| Age (y) | 48.6 ± 15.4 | 44.4 ± 17.3 | 0.697 | 0.492 | 46.3 ± 16.3 |
| Weight (kg) | 72.4 ± 11.4 | 65.4 ± 14.3 | 1.475 | 0.151 | 68.7 ± 13.3 |
| Height (m) | 1.65 ± 0.06 | 1.58 ± 0.05 | 3.081 | 0.005 | 1.62 ± 0.06 |
| BMI (kg/m2) | 25.8 ± 4.20 | 25.8 ± 5.83 | 0.005 | 0.996 | 25.9 ± 5.04 |
| FFlex | 16.2 ± 13.6 | 13.4 ± 8.71 | 0.688 | 0.497 | 14.7 ± 11.2 |
| BExt | 32.2 ± 10.0 | 31.1 ± 12.2 | 0.264 | 0.794 | 31.6 ± 11.1 |
| LFlex | 9.28 ± 6.28 | 9.50 ± 4.61 | -0.107 | 0.915 | 9.40 ± 5.36 |
| RFlex | 10.0 ± 6.83 | 8.75 ± 6.29 | 0.521 | 0.606 | 9.33 ± 6.47 |
Abbreviations: BMI, Body Mass Index; FFlex, forward flexion; BExt, backward extension; LFlex, left lateral flexion; RFlex, right lateral flexion.
aValues are expressed as mean ± SD unless otherwise indicated.
Poor and moderate spinal ROM for FFlex (93.3%, 6.7%), LFlex (63.30%, 36.70%), and RFlex (80.00%, 20.00%) respectively were common. BExt (36.70%, 46.70%) was mostly good and very good (Table 2). 60% of the participants had a medium risk category based on SBT sub-grouping (Table 2).
| Categories | FFlex | BExt | LFle | RFlex |
|---|---|---|---|---|
| Poor | 28 (93.3) | 1 (3.3) | 19 (63.3) | 24 (80.0) |
| Moderate | 2 (6.7) | 4 (13.3) | 11 (36.7) | 6 (20.0) |
| Good | 0 (0.0) | 11 (36.7) | 0 (0.0) | 0 (0.0) |
| Very good | 0 (0.0) | 14 (46.7) | 0 (0.0) | 0 (0.0) |
| SBT risk group | Male (n = 14) | Female (n = 16) | χ2 | All subjects (n = 30) |
| Low risk | 2 (14.30) | 3 (19.0) | 0.210 | 5 (16.7) |
| Medium risk | 9 (64.30) | 9 (56.0) | 18 (60.0) | |
| High risk | 3 (21.40) | 4 (25.0) | 7 (23.3) |
Abbreviations: SBT, StarT back Tool; χ2, Fisher’s exact test; FFlex, forward flexion; BExt, backward extension; LFlex, left lateral flexion; RFlex, right lateral flexion.
aValues are expressed as No. (%) unless otherwise indicated.
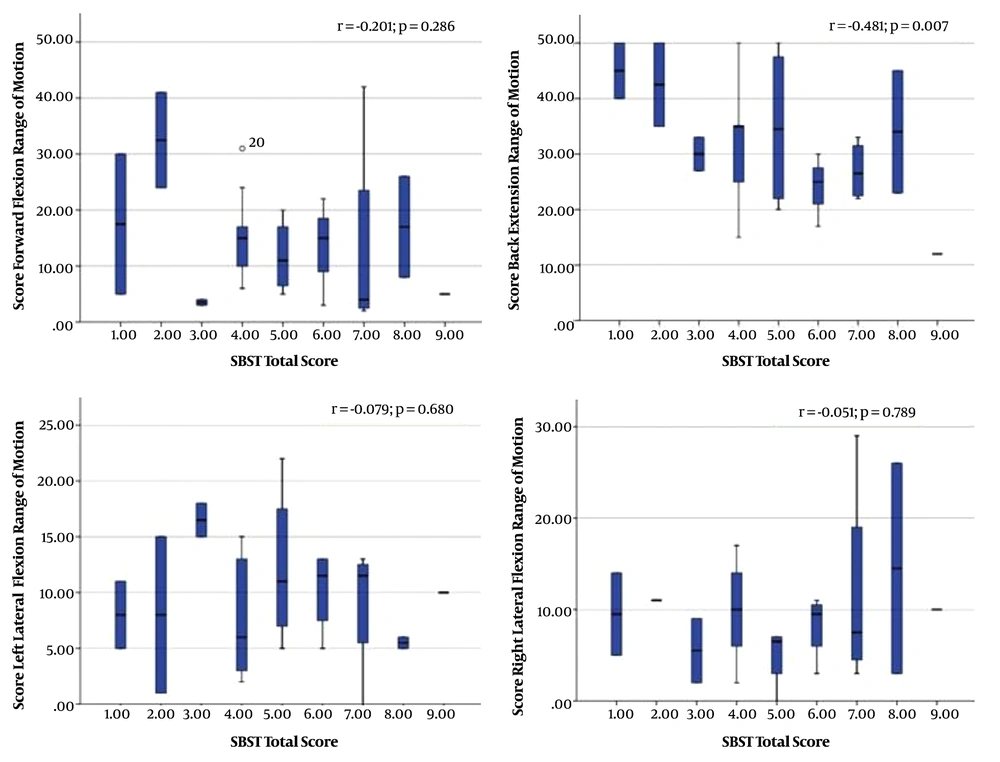
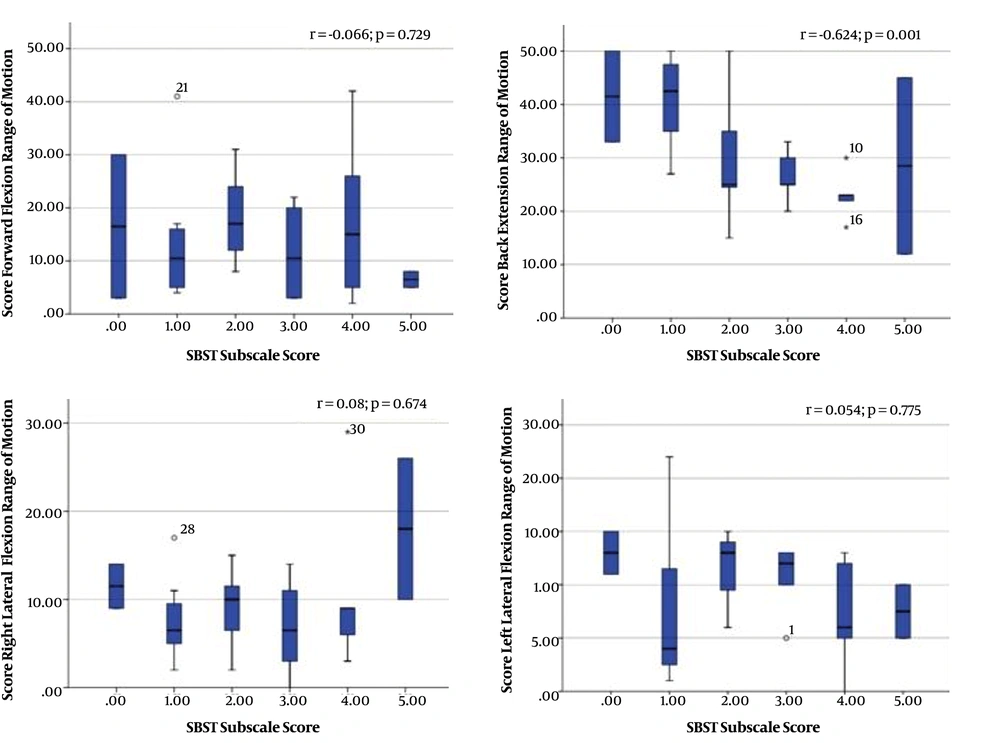
There was significant moderate correlation between SBT total score and BExt score (rho = 0.481; P = 0.007) and between the SBT sub-score and BExt score (rho = -0.624; P = 0.001). Figures 1 and 2 show boxplots for correlation between SBT total score - spinal ROM scores, and SBT sub score - spinal ROM.
There were no significant associations between SBT physical disability risk prediction and spinal flexibility (P < 0.05) (Table 3). Age was a significant mediator in the correlations between SBT total score and each of BExt (P = 0.035), RFlex (P = 0.004), and LFlex (P = 0.012) scores. While height (P = 0.044) significantly influenced Rflex correlation with SBT. Pain intensity significantly influenced the correlation between SBT total score and each of FFlex (P = 0.035), BExt (P = 0.005) and Lflex (P = 0.001). Also, age significantly influenced the correlation between the SBT subscore and each of BExt (P = 0.024), LFlex (P = 0.016), and RFlex (P = 0.012) scores. In addition, gender significantly influenced right (P = 0.027) and LFlex (P = 0.030) correlation with SBT, while height (P = 0.027) significantly influenced LFlex correlation with SBT subscore.
| Spinal Flexibility Level | STarT Back Tool Disability Risk Groups | ||||
|---|---|---|---|---|---|
| Low, No. (%) | Medium, No. (%) | High, No. (%) | Statisticsa | P-Value | |
| Forward flexion | 3.874 | 0.152 | |||
| Poor | 4 (14.2) | 18 (64.2) | 6 (21.42) | ||
| Moderate | 1 (50.0) | 0 (0.0) | 1 (50.00) | ||
| Good | 0 (0.0) | 0 (0.0) | 0 (0.00) | ||
| Very good | 0 (0.0) | 0 (0.0) | 0 (0.00) | ||
| Backward extension | 7.726 | 0.202 | |||
| Poor | 0 (0.00) | 0 (0.0) | 1 (100.0) | ||
| Moderate | 0 (0.00) | 2 (50.0) | 2 (50.0) | ||
| Good | 1 (9.09) | 7 (63.6) | 3 (27.3) | ||
| Very good | 4 (28.57) | 9 (64.3) | 1 (7.14) | ||
| Left-lateral flexion | 1.962 | 0.442 | |||
| Poor | 3 (15.8) | 10 (52.6) | 6 (31.6) | ||
| Moderate | 2 (18.8) | 8 (72.7) | 1 (9.09) | ||
| Good | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Very good | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Right-lateral flexion | 0.817 | 0.820 | |||
| Poor | 4 (16.7) | 15 (62.5) | 5 (20.8) | ||
| Moderate | 1 (16.7) | 3 (50.0) | 2 (33.3) | ||
| Good | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Very good | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| SBT Total Score | |||||
| Contextual factor | FFlex (p-value) | BExt (p-value) | LlFlex (p-value) | RlFlex (p-value) | |
| Gender | 0.753 | 0.620 | 0.265 | 0.108 | |
| Age | 0.129 | 0.035 b | 0.004 b | 0.012 b | |
| Height | 0.524 | 0.684 | 0.658 | 0.044 b | |
| Weight | 0.374 | 0.887 | 0.210 | 0.780 | |
| Body mass index | 0.701 | 0.257 | 0.122 | 0.888 | |
| SBT Sub-Score | |||||
| Gender | 0.929 | 0.249 | 0.027 b | 0.030 b | |
| Age | 0.090 | 0.024 b | 0.016 b | 0.012 b | |
| Height | 0.126 | 0.242 | 0.497 | 0.027 b | |
| Weight | 0.176 | 0.355 | 0.926 | 0.583 | |
| Body mass index | 0.268 | 0.886 | 0.895 | 0.924 | |
Abbreviations: FFlex, forward flexion; BExt, backward extension; LlFlex, left lateral flexion; RlFlex, right lateral flexion;
a Fisher’s-exact test.
b Indicate significance.
5. Discussion
Finding this study reveals that male patients with LBP had higher spinal ROM scores than their female counterparts, but the differences were not statistically significant. This finding is inconsistent with studies reporting that males are less flexible than females owing to their anatomical and geometrical differences (14). Overall, the patients in this study had poor to moderate spinal ROM levels. This finding confirms that the reduction in spinal ROM is the cause and effect of LBP (6). The spinal ROM levels observed in this study were lower than the normative values for regular individuals in Nigeria (15).
From this study, back extension ROM score moderately influences SBT total score and SBT sub-score, respectively. This finding seems to buttress that mobility deficit in lumbar extension compared with flexion is a more common impairment in patients with LBP accompanied by functional disability (16). This may also account for the association between the improvement in lumbar extension ROM and reduction in LBP disability (4-6). 60% of patients with LBP in this study had moderate physical disability risk. It is implied that patients categorized as being at moderate risk predominantly constitute those with physical and psychosocial factors, but not a high level of psychosocial factors, and will most likely benefit from therapeutic interventions (7).
This study also found no significant association between SBT disability risk groups and spinal flexibility ROM categories. Parks et al. (17) found no relationships between lumbar motion and functional test scores in chronic LBP. Another study found a weak positive association between lumbar ROM and disability among patients with sub-acute and chronic LBP (18). Another study reported an inverse correlation between lumbar flexion and disability measures in chronic LBP (19). To our knowledge, this is the first study to explore the relation between SBT and spinal ROM. Thus, the current study seems to align with findings that suggest no significant relationship between self-reported tools for functional disability and lumbar ROM (9).
Hill et al. (7) explained that self-reported disability questionnaires such as the SBT are quick to administer, easy to understand, responsive, and also allows for influences from the patient’s psychological status (20). On the other hand, physical performance measures evaluate what the patient can actually, particularly in cases of poorer physical functioning and compromised spinal motions (21, 22). The lack of a significant association between SBT and spinal ROM tests may indicate that both measures are divergent and may not be used independently but complementary for clinical assessments. Thus, this study corroborates a report by Atya (23) that spinal ROM does not appear to be a valid measure for the prediction of functional disability in patients with chronic LBP.
Age and height were found to significantly mediate the result of the correlation between SBT and spinal ROM. Age is related to trunk ROM impairment among patients with LBP (24). Also, the influence of height on spinal flexibility in a healthy individual is replete in the literature (25), while little has been reported among patients (26). Pain intensity was found to also influence the correlation between SBT prediction and spinal ROM. Ogundele et al. (26) found that patients with higher pain intensity had lower lumbar spine ROM in flexion and extension. Also, age, gender, and height significantly could influence the correlation between and spinal ROM scores and the psychosocial subscale of SBT. Psychosocial factors are reported to be related to LBP (27), and the influence seems to vary depending on personal factors, including demographic and anthropometric parameters (28).
This study has potential limitations. Pain and patients’ psychological state is believed to influence physical performance test results. Also, the sample size in this study was somewhat small, and as such, may affect the generalizability of the findings. The Spearman correlation and Fisher’s exact tests were used instead of Pearson’s correlation and Chi-square test to accommodate this limitation. Future studies with a larger sample size are needed to validate the findings of this study.
5.1. Conclusions
The SBT and spinal flexibility assessment are independent measures of functional disability. They should complement one another in clinical assessment procedures to achieve effective outcomes in the treatment of LBP.