1. Background
Cerebral palsy (CP) is the most common movement disorder among children, which mostly leads to some disabilities such as impairment, function limitation, and participation restrictions (1). Recently performed studies have supported the therapeutic effects of KT on improving motor function. Accordingly, this is a popular method, which is widely used die to being inexpensive and easy to apply and remove or it can be changed according to different therapeutic goals (2).
KT is a special elastic tape made of latex-free cotton fibers with no medication effect. Correspondingly, it has been designed to mimic the elasticity properties of muscle, skin, and fascia (3). Taping a joint directly increases its mechanical stability and it may also be effective on increasing proprioception signals that are important in modulating muscles tone (4).
Some studies have previously reported that KT allows more sensory information to flow to the central nervous system for integration in the presence of mechanical loads, resulting in the improved voluntary control and coordination (5). Ibrahim in a study found that KT could improve sitting control postural parameters, standing control, and balance; however, in pelvic torsion and surface rotation, no significant change was observed (6). In addition, the use of KT in CP children improves fine movement, gross motor function, and independence in activity of daily living (ADL) (3).
One of the most important problems in CP children is postural control problem (7). Of note, principles of the therapeutic approaches in CP mostly rely on achieving normal postural control, improving motor functions, and reaching the maximum level of potential independence (8).
The movement of the center of pressure (COP) has been used to evaluate postural control (9). According to a study by Pavao et al. CP children with higher COP oscillation obtained lower scores in self-care and mobility domains. In addition, a larger COP oscillation indicates the reduced control over the body in response to any imbalance (10).
Compared with healthy children, CP children principally experience the decreased knee extensor peak torque (11). The typical standing posture in CP children with spastic diplegic is the crouch posture, which is determined by excessive knee flexion in standing position. In this regard, quadriceps muscles activity is required to maintain this posture (12). In addition, Cho and Lee in their study reported that functional progressive resistance exercise caused some positive effects by increasing lower extremity strength and morphology of quadriceps, reducing quadriceps tone, and increasing both dynamic balance and functional ability in CP spastic children (13). Therefore, this study investigated the effect of KT on quadriceps muscle on postural sway among CP children. Thus, it can be said that the quadriceps muscle is important for postural control.
In a systematic review by Ortiz Ramírez and Perez de la Cruz it was reported that there are some benefits in the use of KT for CP children and it is important to define the standard criteria for determining the effects of KT, because there is no consensus on the duration of the application of KT or the extent of stretching used. As well, there is insufficient evidence to support KT use (14).
A limited number of studies evaluated the effects of KT among CP children, and the results in this regard are controversial (15). In this regard, several studies have found that the long-term use of KT tapes in rehabilitation of CP children is promising; however, immediate and short-term effects of its usage need more investigation (2).
2. Objectives
This study aimed to investigate the immediate and short-term effects of Quadriceps KT on postural sway among children with spastic CP.
3. Methods
3.1. Participants and Design
This is a before and after study without control group conducted in Neuromuscular Rehabilitation Research Center in Semnan (Iran, 2018). Thirty children aged between 4 and 11 years old with spastic CP were selected through convenience sampling. Children were recruited from rehabilitation clinics in Semnan city (Iran).
The inclusion criteria consisted of children aged between 4 and 12 years old who were diagnosed with spastic CP, the ability to perform the orders and Gross Motor Function Classification System (GMFCS) level of 1 or 2. Moreover, having no open wounds or scratches on the skin surface in thigh and knee regions (16), the absence of fixed deformity in the lower limbs, and walking disability were the other inclusion criteria (17). The exclusion criteria included botulinum toxin injection in the lower extremities for the past 6-months, allergic reaction to KT (16) and lack of children’s cooperation during the study.
3.2. Data Collection
This study was approved by the ethics committee of Semnan University of Medical Sciences (IR.SEMUMS.REC.1396.1, No. 1203, IRCT2017051621686N3). In the first stage, the study process was explained to the parents of the included children and the informed consent forms were signed by them, then the assessments were started.
In this study, 30 children with CP were included, but three cases were then excluded due to a lack of cooperation. Finally, 27 children were enrolled in this study according to the inclusion criteria.
The assessment room was quiet with adequate ventilation and lighting. During the current study, the assessments were done by an undergraduate student of occupational therapy and taping was performed by an occupational therapist (MSc.). The children were assessed during 5 sessions, as shown in diagram (Figure 1). The first session was performed on the first day before taping, the second session was performed 20 minutes after taping, the third session was 24 hours after taping, the fourth session was held by passing 72 hours from taping, and the final session was done after removing the tape (18). In this study The Kinesio Tex, Ares KT was used.
In the children with hemiplegia, tape was done on the affected side. Accordingly, if necessary, the body hair of the front of thigh to below the knee was shaved. Thereafter, KT was applied with the child seated with hip and knee flexed in the chair. Of note, KT was applied to the vastus medialis, vastus lateralis, and rectus femoris muscles. All the tapes were prepared individually as “Y-bands.”
To apply KT on the above-mentioned three muscles, it was applied with 25% tension from the proximal femur (3 cm below the anterior iliac spine) to the proximal patellar and tape “Y” was then splitted above the patellar. Next, the knee was flexed and two ending parts of KT were applied distal to the patella. The first one inch (anchor section) and the ending part were attached with no tension (19). After applying the final tape, we waited for 20 minutes until the thorough KT adherence to the skin. For all the tapes, the facilitation method was used, from origin to the insertion on the quadriceps muscles.
To apply the KT for the rectus femoris muscle, the tape was adhered from the proximal femur to the proximal of the knee. Thereafter, the tape similar to “Y” was split from the top of the patella into two sides of patella, circled it, and finally ended in tuberosity of the tibia (19). Afterward, in order to apply KT on the muscle of vastus letralis, the tape was started from the greater trochanter on the outside of the thigh and then at the top of the knee, KT was divided into two parts, as follows: (1) the medial part was applied near to the lateral of patella and the fixed under patellar apex; and (2) the lateral part was placed on the proximal of the fibulla. Finally, to apply KT for vastus medialis muscle, the tape was started from the one-third of inner part of the thigh and at the top of the knee, KT was divided into two parts as follows: the lateral part was applied near to the medial border of patella and then placed on the distal of patellar apex and the lateral part was placed on the proximal of tibia (20).
3.3. Instrument
The gross motor function of the CP children was categorized by GMFCS. The reliability and validity of the GMFCS were confirmed that supported its usage in clinical practice and research. The inter-rater and intra-rater reliabilities were both high. (ICC = 0.994, 0.993, and 0.996 respectively) and intra-rater reliability was also high (ICC = 0.972- 0.996) (21).
The severity of spasticity in hamstring muscles was measured using modified Ashworth scale (MAS), which is often used as a clinical tool for measuring an increase or a decrease in muscle tone in spastic CP patients. Moreover, MAS is a score-based scale that grades muscle spasticity from 0 to 4 (22). According to ICC scores, inter-rater reliability of MAS varies from moderate to good. As well, the ICC score of MAS is between 0.61 and 0.87. The test-retest result of MAS varies from poor to good. Besides, the ICC value was between 0.36 and 0.83 for MAS (23).
Force plate is a mechanical sensing system designed to measure the COP sway in human beings. The model of the force plate was firstly used in a study by Kistler (B 9286) and controlled via Qualysis software with a capacity to measure COP displacement in the following three-axis: X, Y, and Z (6). Thereafter, perturbation point and the point of most sway of the line of gravity were marked using Qualyzer and then saved in an Excel file. Subsequently, these points were changed into the numbers related to the sway of the line of gravity in the X, Y, and Z axis at the time of the sway. The required data were collected with a frequency of 120 Hz on a computer. The signal of the force plate was then filtered with a cut off frequency of 20 Hz.
The standing stability of the children was evaluated by the use of a linear approach based on COP sway in both mediolateral (ML) and anteroposterior (AP) directions. The following equations were used for analysis.
The children with orthopedic shoes stood on the force plate with feet hip-width apart and a marked point on the force plate was then placed in the middle of their feet and arms at the sides. In all the records, the children's eyes were open and they were looking at a point in front of them with 1.5 meters distance in the same level as their eyes. The needed data related to the force plate were collected within 30 seconds, but 10 seconds of the first and last times of the test were not considered. If the cases suddenly lost their balance, the test was repeated once more. We repeated 3 records per session for each case. The final COP displacement was the mean of the obtained three records. The test-retest reliability of the displacement of COP in ML and AP planes in 5 CP children after one week was found as high. (ICC = 0.85, SEM = 18.62, ICC = 0.76, SEM = 19.16).
The TUG is a test used to measure the balance among CP children (ICC = 0.99). TUG is a simple, valid, and reliable test for examining children with CP (24). Using this test, children sit in the chair with the hip and knees with 90 flexion. Afterward, the children stood up from a chair and walked for 3 meters, turn around, and then sit. The time required for performing this test is the TUG measure (25). This test was done twice and the average of these two times was considered for data analysis.
Data analysis was conducted using SPSS-16 (SPSS for Windows, Version 16.0 (Chicago, SPSS Inc; 2007) at a significance level of 0.05. Kolmogorov-Smirnov test and histogram drawing was used to assess the normality of variables. To examine the difference of the variables in five records of the TUG and the COP displacement, repeated measure analysis was used. To find the difference between measures, Bonferroni Correction was used.
4. Results
In this study, 17 children with hemiplegia and ten children with diplegia were enrolled (19 boys and 8 girls). As well, 18 children were in GMFCS level 1, and 9 cases were in GMFCS level 2. In terms of the MAS score of hamstring muscles, 16 children had grade 1, eight of them had grade +1, and three children had grade 2. The mean (standard deviation) age, height and BMI were 7.11 (2.87) years, 117.63 (18.68) cm, and 15.88 ± 2.79 kg/m2.
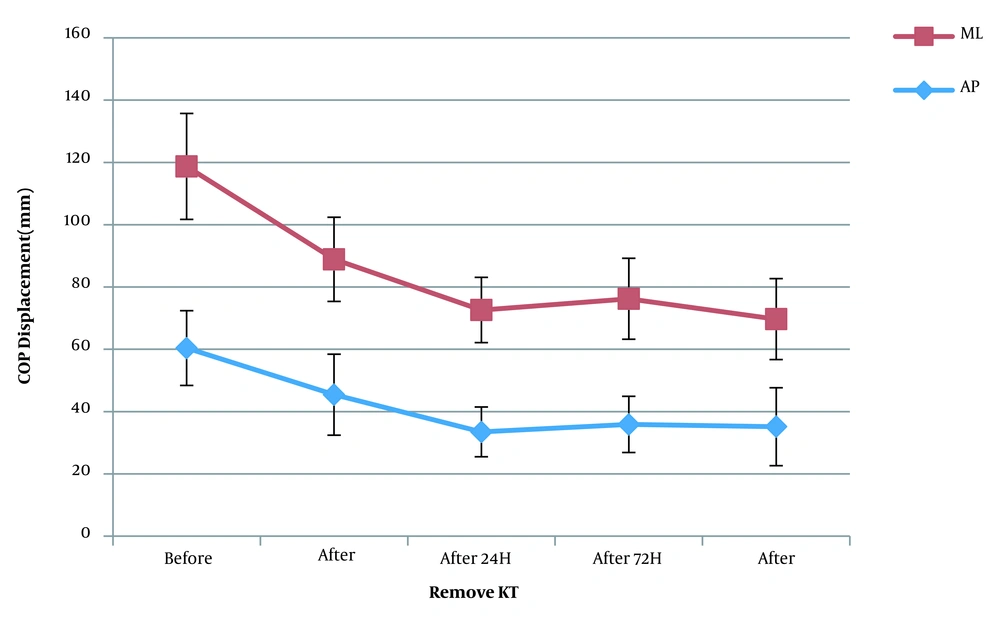
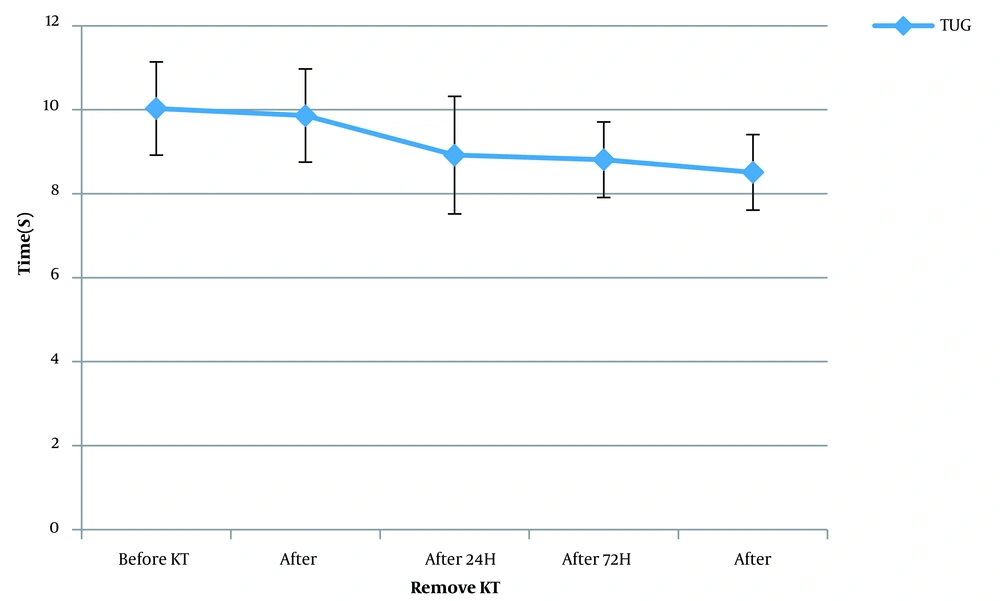
The mean and standard deviation of the five records of COP displacement and TUG as well as the results of repeated measure analysis with a Greenhouse-Geisser correction are shown in Table 1 and Figures 1 and 2. Moreover, it was indicated that the results of the five assessments of KT on QcM could reduce the time of performing the TUG test (P < 0.01). Also, COP displacement on the mediolateral (ML) and anteroposterior (AP) direction decreased significantly (P < 0.05).
| Variables/Assessment Session | Mean ± SD | 95% Confident Interval | F | P Value | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| TUG | 8.72 | < 0.001 | |||
| First | 10.03 ± 2.28 | 9.13 | 10.94 | ||
| Second | 9.86 ±2.21 | 8.99 | 10.74 | ||
| Third | 8.92 ± 2.8 | 7.81 | 10.03 | ||
| Fourth | 8.51 ± 1.87 | 7.94 | 9.68 | ||
| Fifth | 8.51 ± 1.87 | 7.77 | 9.25 | ||
| ML COP displacement | 5.018 | 0.005 | |||
| First | 58.31 ± 33.83 | 44.02 | 72.6 | ||
| Second | 43.45 ± 26.9 | 32.09 | 54.81 | ||
| Third | 39.14 ± 21.28 | 30.15 | 48.13 | ||
| Fourth | 40.34 ± 26.05 | 29.34 | 51.35 | ||
| Fifth | 34.53 ± 26.55 | 23.31 | 45.74 | ||
| AP COP displacement | 7.7 | < 0.002 | |||
| First | 64.03 ± 40.01 | 46.8 | 79.93 | ||
| Second | 45.44 ± 25.91 | 34.5 | 56.39 | ||
| Third | 33.48 ± 16.04 | 26.85 | 40.1 | ||
| Fourth | 35.89 ± 18.16 | 28.2 | 43.58 | ||
| Fifth | 35.15 ± 23.01 | 25.65 | 44.66 | ||
Abbreviations: SD, standard deviation; TUG, time up and go; COP, center of pressure; ML, medial lateral; AP, anterior posterior.
The difference between the five sessions’ assessments using Bonferroni Correction showed that before the taping process and 72 hours after that, the decrease in the COP displacement was significant and the time of performing the TUG test significantly decreased. Before and after the taping, the results of COP displacement and TUG test were not significant. Furthermore, no significant difference was observed among all the assessments by passing 24 and 72 hours. The reduction in the COP displacement only in the AP direction was significant by passing 24 hours from the taping.
5. Discussion
The results of this study show that immediately after the KT application over the QcM muscle of children with spastic CP, COP displacement and walking speed do not change. We observed that KT reduced the COP displacement in AP and ML directions after 72 hours, and increased walking speed. So, it can be said that in children with spastic CP, the effect of KT on the QcM muscle can be observed during the first 72 hours.
In this study, we only examined the muscle function, not its activity, and we observed no significant change in the immediate effect of KT. It was demonstrated that the use of KT for short-term could improve balance among CP children. The facilitating effect of KT on cutaneous mechanoreceptors results in some physiological changes in the taping area and also improves muscle excitability even in the short-term. Therefore, applying KT in short-time could stimulate cutaneous mechanoreceptors in CP children, thereby improving proprioceptive inputs for muscles to better perform (16).
There is a deficit in sensory pathways in CP children, known as the decreased tactile and proprioceptive stimuli receptions. Stimulation of somatosensory receptors in skin, ligament, and joint capsule, leads to the activation of gama motoneuron, which, in turn, regulates the modulation of Ia afferent fibers. So, the feedback provided by Ia afferent fibers could consequently control the recruitment of motor units with a high threshold that are responsible for producing strength (11).
This based on that, the KT application could not lead to the reduced COP displacement after 24 hours. It seems that after 72 hours, the increased QcM muscle activity along with the effect of motor learning could improve the muscle performance by decreasing COP displacement in spastic CP children.
Since the QcM muscles are extensors of the knee and this movement occurs in the sagittal plane, it can be said that the improvement in QcM activation could decrease the COP displacement in the AP direction even during the first 24 hours. In addition, due to the role of the QcM muscle in gait, the speed of walking increases, as well.
Because most children included in this study were hemiplegic CP, it is possible that there was a misalignment of the pelvis in the frontal plane like ipsilateral drop, due to knee flexion in the paretic limb. It seems that by applying KT over the QcM muscles on the affected side and increasing muscle activity, the knee joint was extended in quiet standing and hip alignment was corrected in the frontal plane, so the COP displacement decreased.
Dos Santos et al. in a study investigated the effects of Kinesio taping on the rectus femoris by measuring the muscle activity through electromyography. It was reported that in children with unilateral CP, the immediate effect of KT on the rectus femoris muscle improved muscle activation and body alignment during the performance of sit-to-stand, but it did not clinically change any functional measure such as the time used to do the task (15). Additionally, we observed no significant change in the immediate effect of KT on muscles function in walking speed and COP displacement.
Dos Santos and Rocha in a case-report study conducted on the immediate effect of KT on knee extensor torque of children with CP mentioned that the use of KT could increase the muscle strength in children with CP. They suggested that KT could be more effective on children with muscle weakness (11). Furthermore, they investigated the effect of KT in three children who may differ in terms of the severity of QcM weakness from our participants.
In another study, Ozmen et al. found that KT does not affect the spasticity of plantar flexor muscle and ankle range of motion, but it improves the balance and gait in the hemiplegic CP children by passing 48 hours from the KT application (26). In addition, Jang et al reported that the KT application could improve walking speed, step length, stride length, and right single limb support time in diplegic CP children. However, no significant differences were found in cadence, left leg single support time, (27) and double support time. In line with the results of the current study, these studies concluded that the use of KT could improve the balance in children with CP.
In line with our study, regarding the short-term effect of KT, Partoazar et.al in a study applied KT on the thoracic and lumbar regions of CP children. They evaluated children before, immediately after, after 48 h from applying the KT, and after 48 hours from its removal. As a result, they reported that KT seems to be effective on improving dynamic balance and functional mobility in spastic CP children, so it can be used as a complementary therapy in the neurorehabilitation of CP children (28).
According to our results, the short-term application of KT on the QcM muscles could lead to the improved walking speed as well as the decreased COP displacement in children with spastic CP. Of note, the use of KT on QcM could not immediately improve balance in these children.
5.1. Study Limitation
This study was a before-after trial with no control group. Our sample size was small, and the CP children who participated in our study had high function, so the results could not be generalized to all CP children. We applied KT only on the QcM muscles; therefore, it is recommended in further studies to investigate the KT application on other muscles in lower extremity.