1. Introduction
Major depressive disorder (MDD) is a common psychological disorder. MDD is more common in women than men, particularly from adolescence to mid-50s, with a rate of 1.2 to 2.7 (1). In Iran, the prevalence of depression is about 1.7 times higher among women than men (2). It’s well-documented that functional and structural alterations of the brain are the major causes of depression (3).
As brainwave oscillations are potential biomarkers for MDD (4), there is an increasing tendency towards using quantitative EEG to assess electrical patterns of the brain in patients with psychological disorders (5). For example, the asymmetry of frontal alpha activity and increased frontal alpha are promising and generally known neuro-markers for MDD (6). There is a large body of evidence suggesting that transcranial direct current stimulation (tDCS), among various treatments, is a potentially non-pharmacological method for treating MDD patients (7, 8). From a theoretical perspective, tDCS might reduce depression symptoms through anodal stimulation of the left frontal cortex and reducing right frontal hyperactivity by cathodal stimulation. It has been convincingly shown in practice that tDCS can affect prefrontal functions and might be used as a promising treatment method for depression (9).
Several studies have mentioned acceptance commitment therapy (ACT) as a therapeutic option for depression and anxiety (10). For example, Karlin et al. (11) reported that ACT was an effective treatment for depression among veterans. In another study, ACT was considered as a treatment for depression in women with breast cancer (12). ACT emphasizes experiencing difficult emotions such as grief and loss rather than avoiding them. Hence, it can increase psychological flexibility by focusing on actions related to the core values of the patient (13). Regarding the association between ACT and brain functional activity, Smallwood et al. (14) have demonstrated that administering ACT causes reduced activation in regions which are commonly involved in the brain’s responsiveness to painful stimuli such as the middle frontal gyrus, inferior parietal lobe, insula, anterior and posterior cingulate cortex, and superior temporal gyrus. Mindfulness-based approaches like ACT impact the brain regions that are involved in attention control, emotion regulation, and self-awareness (15).
Among many currently available depression-management techniques, group therapy (GT) is getting more attention recently. As an example, O’Neill et al. (16) reported a significant improvement in the intervention group compared to controls. Considering group versus individual treatment, as a moderator method is another important issue for psychological disorders such as depression (17). As group therapy is less costly than individual therapy, it can be provided for a longer period, during which may help the patients ease their negative emotions by feeling more connected with others in terms of social interactions and experiencing more satisfaction with their life (18). Additionally, based on recent research, groups are perceived as happy and safe places to experience new feelings (19).
Although tDCs, ACT, and GT separately have been considered effective for treating depression, some patients presented only a minor or no improvement after receiving these treatments in isolation. Besides, many patients experience relapses following receiving acute treatment (20). Therefore, we hypothesized that (1) using GT after a combination of tDCS and ACT may prevent recurrence and relapse and, (2) there will also be differences in EEG oscillations of a depressed person after combining these methods.
According to the best knowledge of the authors, no study has investigated the long-term effects of combined administration of tDCS (QEEG-based), ACT, and GT. Hence, in this study, for the first time, we presented a female MDD patient who showed a long-term response to a novel treatment. We propose the treatment as a triangular systematic process. The triangle’s edges are tDCS, ACT, and GT interventions which were provided in succession (Figure 1). The patient showed improvements in Beck Depression inventory-short form (BDI-SF), Acceptance, Action questionnaire-II (AAQ-II) scores, and neurophysiological assessment (QEEG) after this triangular treatment.
2. Case Presentation
The patient was an unemployed 30-year-old right-handed female with a history of suffering from major depression for almost three years. She was single and was the last child in her family. She had a history of a suicidal attempt during the aforementioned period. Besides, she was suffering from anhedonia, motivation, a decrease in appetite, and loss of energy. She was grown up in a crowded family with uneducated parents. The patient showed resistance to antidepressant medication since treatment with SSRIs (citalopram and sertraline) prescribed by psychiatrists; however, little improvements were observed during the past six months. She was severely depressed with a very low level of social interactions, liked to be alone at home all the time, her self-esteem and hope were decreased, and she had problems with going to sleep. The patient also exhibited negative ideas about marriage and thought, if married, her situation will be exacerbated. She was admitted to Psychotherapy and Neurotherapy Center. Afterward, she consented to the treatment protocol carried out in 2018. The study was approved by the Ethical Committee of the Research Center of Shahid Ashrafi Esfahani University (12-18) and was conducted according to the principles of the Helsinki’s Declaration. She underwent a QEEG baseline examination before conducting any treatment.
At the first stage of the triangle, based on the patient’s QEEG analysis, tDCS was administered for 12 sessions three times a week (1st edge). Secondly, she started receiving ACT twice a week for eight 1.5 h sessions (2nd edge). Finally, she underwent receiving GT every two weeks (3rd edge).
2.1. EEG Acquisition
Nineteen surfaces (19 active and 2 references) EEG electrodes were placed according to the international 10/20 system using a linked-ear montage. All data were sampled with a frequency of 250 Hz. Besides, to minimize aliasing effects a band-pass filter between 0.1 to 35 Hz was used. All electrode impedances were kept below 5 kΩ. The EEG was recorded with the patient in a comfortable chair in both eye-open and eye-close conditions (each lasted five minutes) before treatment, both after the tDCS protocol and at the final stage of the triangular method.
To exclude contaminated EEG and removing eye and head movements, muscle, or Alpha artifact, all data were visually inspected. The analysis was conducted on four frequency bands delta, theta, alpha, beta, and high-beta with Neuroguide software version 2.3.8 (21). Subsequently, low-resolution brain electromagnetic tomography (LORETA) analysis was used to estimate changes in intracerebral activation (22).
2.2. tDCS Intervention
tDCS was delivered by a pair of rubber carbon pads (10.5 cm2). Through 12 sessions of tDCS treatment, anodal stimulation (with a 30-second ramp on, 8-second ramp down, 1.5 mA current was applied for 20 minutes) was performed on F3 while cathode was placed over the contralateral shoulder. The localization of the electrodes was fine-tuned using LORETA source localization based on the EEG. Both anodal and cathodal stimulation was delivered by an Iranian electrical stimulator device (NEURO STIM 2). The safety guidelines specified by Nitsche et al. (23) were followed during treatment.
2.3. ACT Intervention
A certified psychotherapist worked with the patient in the acceptance commitment therapy edge for 1.5 hours each session, twice time a week for a total of 8 sessions (24). The therapy sessions provided following the program are described in Table 1.
| Session | Introducing concepts | Description |
|---|---|---|
| 1 | Creative hopelessness | Helped the patient to experience the costs of her avoidance behavior. |
| 2 | Control strategies | Increased patient’s awareness that her controlling strategies is one of the main causes of her symptoms. |
| 3 | Defusion strategies | Helped the patient to notice her thoughts and feelings and related to them with different lenses. |
| 4 | Acceptance/willingness | Increased patient’s acceptance of attitudes toward negative feelings. |
| 5 | Values | Helped the patient to be aware of her positive values. |
| 6 | Observing self | Helped her to observe herself objectively and compassionately. |
| 7 | Committed action | Modulated her ability to take actions guided by her values. |
| 8 | Review | Reviewed the previous sessions with her, assessed the proposed techniques and her satisfaction. |
2.4. GT Intervention
Receiving group-based therapy may help the patients to share their feelings with others and assists them to realize they are not alone. Therefore, GT was applied as a maintenance treatment over a minimum of 3 months to avoid withdrawal symptoms or rebound relapse (25). Group therapy for depression is multimodal psychoeducational group treatment. It gives patients the techniques and strategies for coping with the problems that are assumed to be related to their depression. Our GT protocol addressed several target behaviors such as social skills, thought management, self-monitoring, setting realistic goals, pleasant activities, and relaxation in line with the coping with depression course at the University of Oregon Depression Research Unit. Using these strategies helps the patient to feel more effective in handling daily activities. Groups typically consist of 6 to 10 adults (aged 18 and older), with a single group leader (a therapist may be used) every two weeks for 2 hours.
2.5. Instruments
2.5.1. Beck Depression Inventory-Short Form
It consists of 13 items for assessing the severity of depression using statements scored on a three-point Likert scale. The Persian version of the BDI-SF was used in the present study. Cronbach alpha from previous studies with Iranian samples ranged from 0.89 to 0.94 (26).
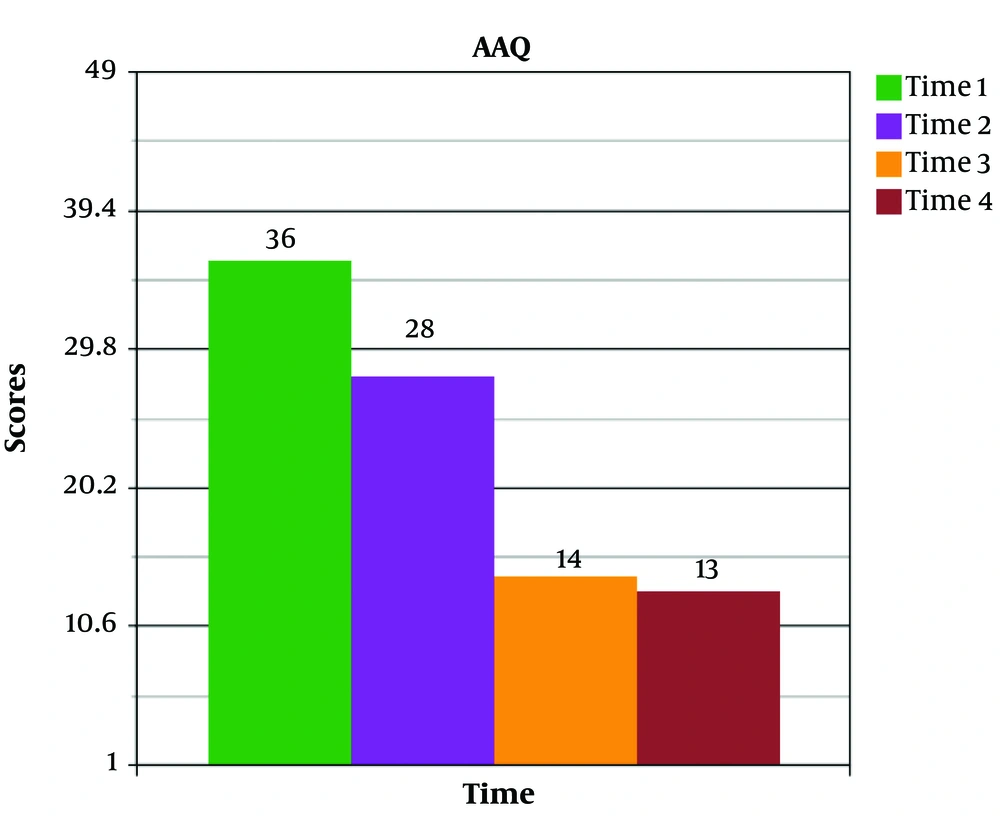
2.5.2. Acceptance and Action Questionnaire-II
This is a reliable (alpha coefficients: 0.84) one-factor measure of psychological inflexibility, or experiential avoidance and is made of seven items (Individuals respond to a 7-point Likert scale ranging from never true to always true. Higher scores indicate greater levels of psychological inflexibility (27).
2.6. QEEG Data
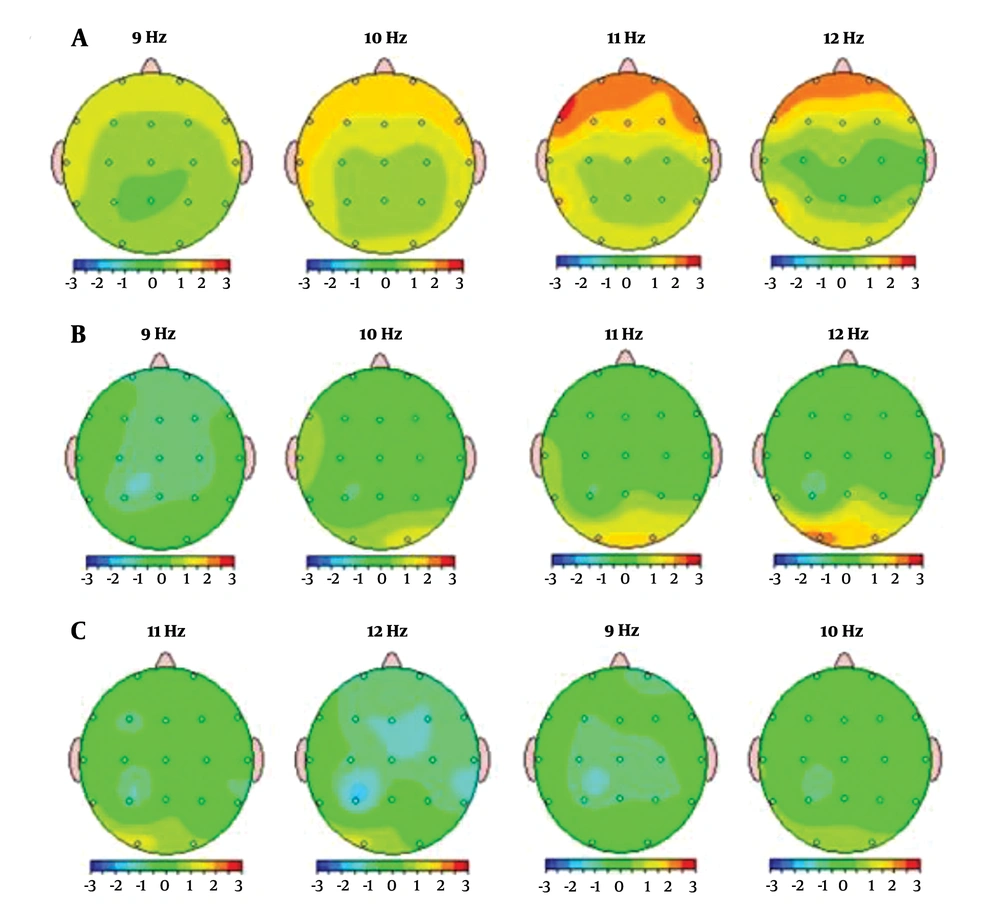
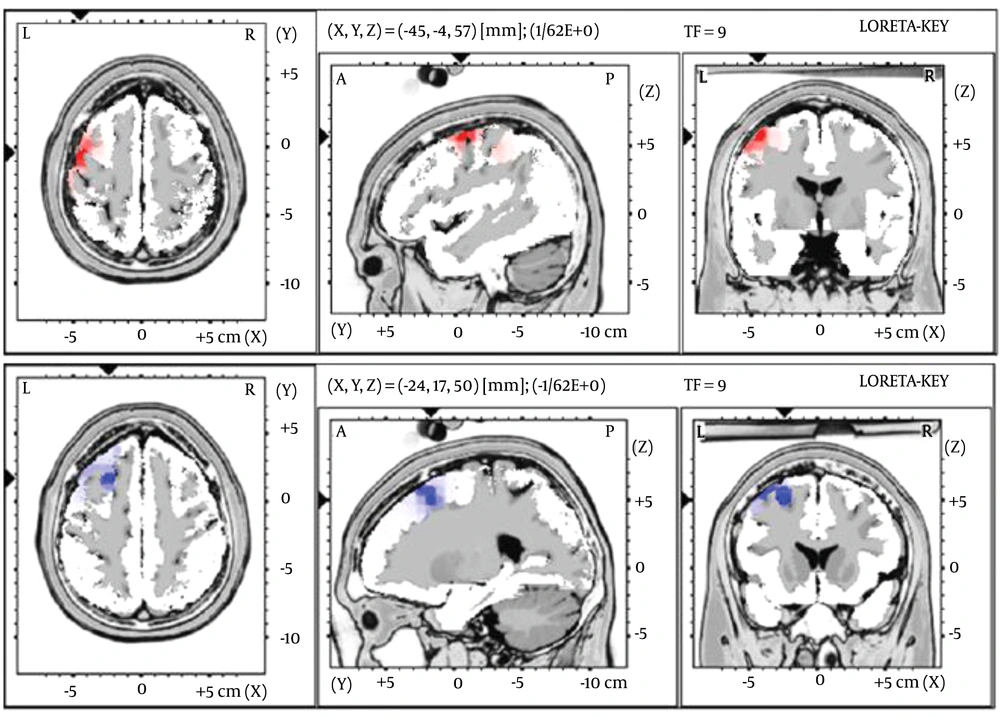
Detailed brain maps of the patient were obtained on the baseline, after providing the tDCS, and after the final stage of the protocol (GT). LORETA analysis was used to elucidate electrophysiological changes before and after performing the protocol. In line with previous studies on biomarkers of depression (22), pre-treatment QEEG maps were typical for many depressed patients and showed Alpha increase, especially in frontal areas (as shown in Figure 2A) as well as an area of dysregulation in the left superior frontal gyrus (Brodmann area 6) on LORETA imaging (Figure 3, [top]). Following tDCS sessions, noticeable improvement in Alpha dysregulation was observed (Figure 2B). The third QEEG brain map and LORETA analysis were obtained after completion of GT sessions (Figure 3 [down] and Figure 2C). This final analysis showed that the previous effects are maintained after four months from ACT to the finalization of GT. Overall, the patient’s brain maps exhibited a marked correction of previously elevated frontal Alpha activity in a stable fashion.
QEEG maps before (baseline), during (after tDCS), and after the final edge of the protocol (GT). A, baseline QEEG brain map data shows excessive alpha power in frontal areas; B, there is a significant reduction of previously (pre-treatment) increased alpha in frontal areas and a major decrease in Alpha power can be seen in Z Score FFT absolute power; C, this final map was acquired after GT treatment and shows the outcome of previous treatments maintained during 5 months. (QEEG compares the data of the patient with normal controls with color-coded maps based on SD).
Images of voxel-by-voxel brain regional analysis using LORETA comparing before and after triangular protocol in the alpha band. Pre-treatment analysis shows an area of electrical dysregulation in the precentral gyrus, BA 6 (top). The lower part of the picture shows the resolution of previously identified dysregulation after the triangular protocol.
2.7. Clinical Data
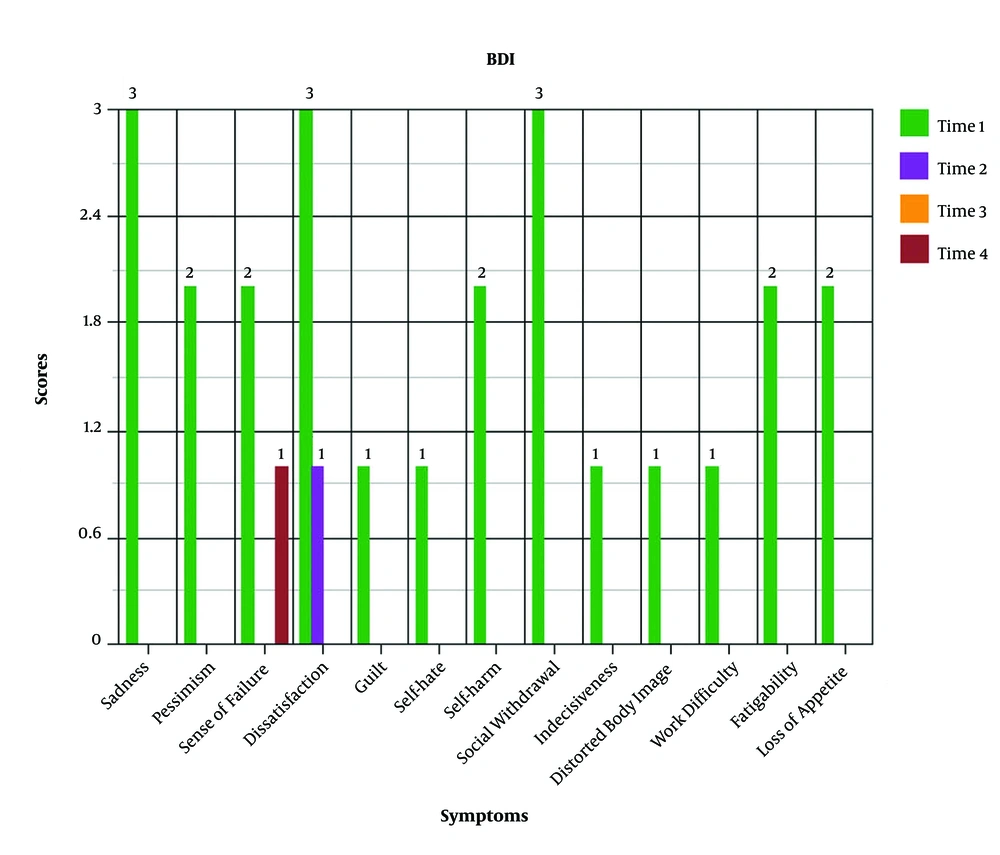
According to the BDI-SF and AAQ-II, the levels of depression symptoms and psychological inflexibility were decreased, respectively (Table 2). Among 13 items of BDI (i.e. sadness, pessimism, sense of failure, dissatisfaction, guilt, self-hate, self-harm, social withdrawal, indecisiveness, distorted body image, work difficulty, fatigability, and loss of appetite), a dramatic decrease was observed for sadness and social withdrawal just after tDCS (stage 1, Figure 4). The decreasing trend was maintained after ACT and GT (stages 2 and 3). Among several stages of the project (baseline, DC, ACT, and GT), AAQ dramatically decreased after ACT (Figure 5). Similarly, the observation was maintained after the third edge of the triangle protocol.
| Measures | Time 1 | Time 2 | Time 3 | Time 4 |
|---|---|---|---|---|
| Beck depression inventory-short form | 24 | 0 | 1 | 0 |
| Acceptance and Action questionnaire-II | 36 | 20 | 22 | 18 |
aTime 1, baseline; time 2, transcranial direct current stimulation (tDCS); time 3, acceptance commitment therapy (ACT); and time 4, group therapy (GT).
3. Discussion
There is plenty of evidence concerning novel treatments for major depression, as a prevalent disorder of our era (1). ACT, GT, and tDCS are among these interventions, which are particularly useful for amelioration of depressive symptoms (8, 28). However, for those who receive these interventions (which are carried out separately or concurrent), the risk of depression relapse is high. To the best of our knowledge, combining the effects of different therapies in succession for the MDD was explored very rarely in related literature. The results of the present case report, with a succession of tDCS, ACT, and GT, were promising, as the triangular protocol showed remarkable improvements in both electrophysiological and clinical measurements.
From the electrophysiological perspective and based on previous results associated with alpha reduction in prefrontal areas (which was also observed in EEG assessment of our patient), at the first stage, we used tDCS to increase prefrontal activity. QEEG analysis after this period revealed remarkable changes in the electrophysiological activity of the patient, as reported in previous studies (29, 30). In addition, dramatic changes were observed in most of the depression symptoms. Our findings are consistent with Khayyer et al. (31) showed that non-invasive electrical stimulation of the frontal lobe decreased depression scores. This can be explained by the active role of the left frontal area, especially DLPFC, in developing depression (32). Additionally, locations of stimulation were based on the specific and sensitive QEEG measurements used in the present study. However, applying tDCS couldn’t increase “satisfaction” (one of the BDI subscales) as intended, and that is why ACT was started for the patient. On the other hand, to induce effects beyond tDCS, which are desirable, especially to achieve therapeutic effects in clinical studies, a psychotherapy intervention was suggested.
As brain activity was changed following tDCS, we supposed it was time to work on mental reconstruction using ACT techniques. These techniques target cognitive fusion and experiential avoidance, which are prevalent among depressive people. We observed that the patient’s psychological flexibility mostly increased after receiving ACT, which consequently led to higher levels of satisfaction. This result is similar to the findings of Karlin et al. (11), who reported that ACT was effective in improving depressed veterans. Meanwhile, the patient’s second QEEG showed a more alpha decrease in the frontal areas of the brain. A possible interpretation is that neuromodulation, along with talk therapy, seems to have set the stage for a synergistic effect of biology and psychology. In a similar vein, mindfulness, diffusion, acceptance, and other ACT exercises have influenced brain regions related to attentional control, emotional regulation, and self-awareness (15). There are some indications that the reactivity of the emotional brain systems between the frontal executive and the limbic system might be modulated by mindfulness (33).
It has been suggested that chronic or more severe recurrent forms of depression present a weaker response to purely psychological treatments (18), and that in patients with severe depression, combined therapy is superior to sole psychotherapy. There is also evidence that about 50% of patients who were recovered by the end of psychotherapeutic treatment suffered a relapse within two years (34). Given the chronic nature of depression and the high chance of relapse, GT was applied as a maintenance treatment. In line with Vittengl et al. (35), CBT was effective in reducing relapse in depression. Accordingly, the third QEEG of the patient demonstrated more frontal activity following GT. This outcome may be explained by improving frontal functions such as social abilities, problem-solving, and impulse control. This is the third edge of the triangular protocol, which was related to social competencies.
This study is the first demonstration for therapeutic and relapse prevention of combining three methods of treatment (from brain stimulation to CBT methods) in succession for depression. Each of the treatments considers different aspects of depressive disorder, and their schedules were based on different outcomes. While future research should consider these different aspects of the disorder simultaneously, the present investigation shall be considered as only a clinical case study, rather than a robust clinical study design.
Based on the positive results of the study, it might be important for future research with larger samples to consider the proposed protocol and provide further evidence that this method may be an effective and long-lasting treatment.