1. Background
Diabetes mellitus (DM) is a serious, long-term disease with a major impact on the well-being of individuals, families, and societies worldwide. Diabetes claims for four million deaths per year (1), and its prevalence is rising to 10.2% (578 million persons) by 2030 and 10.9% (700 million persons) by 2045 (2). This rising trend is attributed to aging, obesity, hypertension, immigration, and urbanization (3). In line with the increasing prevalence of diabetic mellitus in the world (2), Iran is also experiencing an increase in the risk factors of diabetes, including aging (4, 5) and lifestyle-related factors (6).
Diabetes, if left untreated, may lead to relapses, side-effects, and more severe complications such as ulcers and infections (7). The improper management of diabetic foot ulcers (DFU) eventually leads to amputation (8) and its relevant problems, including reduced quality of life and economic burdens (9-12). Accordingly, preventive measures and timely treatment are of great significance (13).
About 60% (14) of patients suffer from some degree of amputation. Mortality rates associated with developing a diabetic ulcer (DU) are estimated to be 5% in the first 12 months and 42% in five years (15). Diabetes complications may lead to long-term hospitalization (16), progressive therapy (17), and even death (18). To save limited hospital resources and given the preferences for prevention, the development of community-based care management is considered a priority (19, 20). Care management is defined as “a set of activities designed to assist patients and their support systems in managing medical conditions and relevant psychosocial problems more effectively” (21). Care management dates back to the 21st century, which was introduced to solve the dichotomy between management and care delivery in practices (22). To address the burden management of chronic diseases such as diabetes effectively and equitably, integrated approaches must be applied in strategies and interventions (23) proposed in some other studies (24, 25).
In this regard, the DFU care management encompassing outpatient care, self-management, and prompt treatment (9), could reduce the need for hospitalization (26). Good glycemic control and active investigation against the peripheral arterial disease (PAD) are important in reducing infection and amputation risks (27). Beiranvand's study shows that despite patients and families’ positive attitudes, they have poor knowledge and care performance (28). Socio-cultural factors influence self-management; therefore, policy-makers and care providers must re-evaluate this process (29). To improve diabetes management, multidisciplinary teams are added to the prevention and treatment process (30). The National Diabetes Prevention and Control Program is implemented in Iran for the early diagnosis and appropriate treatment (31, 32). One relevant study showed that this program positively influenced participants (33).
Accordingly, it is necessary to obtain adequate information about diabetes care management, the consequences of relevant programs and care challenges, and factors affecting wound creation. Researchers have decided to explore the experiences of patients, families, managers, and care providers about DU; hence a qualitative study seems necessary to understand the depth of their experiences.
2. Objectives
This study sought to collect profound experiences about diabetic ulcer care management with an emphasis on community-based care.
3. Methods
3.1. Research Design
This research was carried out using the qualitative content analysis method during 2017 - 2018, in Semnan Province, Iran.
3.2. Participants
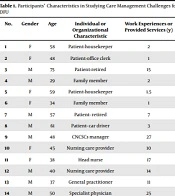
The main participants included those suffering from diabetic ulcers, who were willing to share their experiences, and another group of participants were purposefully selected based on the extracted data. The participants were ensured of information confidentiality and their voluntary participation in the study. In this regard, their informed written consent forms were collected. Fourteen participants were purposively selected from CNCSCs, outpatient clinics, physician offices, and hospitals according to the data (Table 1). The participants who were chosen from community-based care centers and hospitals, either as clients or care service providers, played a critical role in the DFU care management process.
| No. | Gender | Age | Individual or Organizational Characteristic | Work Experiences or Provided Services (y) |
|---|---|---|---|---|
| 1 | F | 58 | Patient-housekeeper | 2 |
| 2 | F | 48 | Patient-office clerk | 1 |
| 3 | M | 75 | Patient-retired | 15 |
| 4 | M | 29 | Family member | 2 |
| 5 | F | 59 | Patient-housekeeper | 1.5 |
| 6 | F | 34 | Family member | 1 |
| 7 | M | 57 | Patient- retired | 7 |
| 8 | M | 61 | Patient- car driver | 3 |
| 9 | M | 48 | CNCSCs manager | 27 |
| 10 | F | 45 | Nursing care provider | 10 |
| 11 | F | 38 | Head nurse | 17 |
| 12 | M | 40 | Nursing care provider | 14 |
| 13 | M | 37 | General practitioner | 11 |
| 14 | M | 50 | Specialist physician | 25 |
Participants’ Characteristics in Studying Care Management Challenges for DFU
3.3. Data Collection
The data were collected using some general questions such as “how did you recognize the emergence of the ulcer?" Interviews were followed with some semi-structured questions as follows: "what did you do after recognizing the ulcer?", "can you explain more about the follow-up of ulcer treatment?" or "what do you mean by ulcer care?" (34). The interviews lasted from 25 to 65 minutes, with an average of 40 minutes. Data collection continued as long as hidden data were discovered, and no new code was extracted.
3.4. Data Analysis
During the data collection phase, the data analysis process was also performed according to Graneheim and Lundman's five-step approach (35). In this regard, interviews were transcribed verbatim. To be immersed in the data, the researcher listened to the interviews and reviewed the text of the manuscripts several times to extract the meaning units from the participants' statements and specify them in the form of codes (ie, meaning units). The codes were also classified based on semantic and conceptual similarity and became concise as much as possible (ie, abstracting). The units of analysis and their subcategories were decreased (ie, sorting). Finally, the data were placed in the main categories, which were more general and conceptual, and the themes were abstracted (ie, formulating themes).
Meanwhile, Guba and Lincoln's criteria were used to reinforce the rigor of data (36). To evaluate the credibility of the findings, the extracted codes were checked by some participants and modified if necessary. The researchers had prolonged engagement and spent about two years collecting and analyzing data. To assess confirmability, all the interview texts, the codes, and categories were reviewed and approved by the authors and two faculty members, who were not the research team members. To confirm dependability, the research steps were recorded accurately in detail. The participants were selected with maximum variation to observe acceptability and transferability.
4. Results
Table 1 shows the participants’ characteristics in studying care management challenges for DFU.
Most participants had diabetes for about ten years, and they had been affected by diabetes ulcers at least once or twice. Two main categories emerged in this study were as follows:
(1) "Dispersion in preventive measures" with the following subcategories: ‘vague perception of disease symptoms’, ‘inability in self -management’ and ‘low-efficient preventive care’,
(2) "Gradual access to outpatient services" with the following subcategories: ‘gradual expansion of outpatient ulcer care’, the’ complexity of financial transactions’, ‘improving inter-sectorialsectoral cooperation’ and ‘ambiguous professional boundaries’ (Table 2).
| Main Category (Theme) | Category | Subcategory |
|---|---|---|
| Dispersion in preventive measures | A vague perception of disease symptoms | Exacerbation of disease caused by comorbidities |
| Variety of underlying factors in the onset of symptoms | ||
| Intermittent onset of symptoms | ||
| Inability in self-management | superficial familiarity of patient and his/her family about care and drugs | |
| Late awareness of onset of diabetic ulcer symptoms | ||
| Low efficient preventive care | Recurrence of ulcer by injuries | |
| Exacerbation of symptoms due to inadequate prevention measures | ||
| Hospitalization due to inadequacy of outpatient care measures | ||
| Gradual access to outpatient services | Gradual expansion of outpatient services of ulcer care | Relative expansion of nurses' capabilities in ulcer care |
| Gradual expansion of outpatient centers of ulcer care | ||
| Complexity of financial transactions | Gradual transparency of tariffs | |
| Complaints about costs of outpatient services | ||
| Expansion of insurance coverage for wound care | ||
| Improving inter-sectorial cooperation | Increase in referrals of patient to nursing centers | |
| Gradual tendency of physicians to refer patients to nursing centers | ||
| Ambiguous professional boundaries | Ambiguity in activity boundaries | |
| Focus of patient and family’s demands on general ulcer care |
Participants’ Experiences About Care Management Challenges for DFU
4.1. Dispersion in Preventive Measures
According to participants' experiences, several factors cause diabetes ulcers, the most important of which are carelessness and physical injuries. Moreover, the severity of these symptoms fluctuates and sometimes increases and sometimes decreases. In general, patients' statements were ambiguous about the onset of symptoms.
" To some extent, I could not feel my feet while wearing socks. I ignored my toes until I saw an ulcer between them" (A patient No. 8).
The improper examination of vulnerable parts and insufficient attention to the symptoms can increase the severity of ulcers. Lack of training for patients and their family was the main cause of inappropriate self-management.
"… they (patients or families) do not receive enough training about the early symptoms of ulcers. Even when the ulcer is emerged, they treat it in their own way even though they do not have appropriate skills in this case" (A medical specialist No. 14).
In addition to nurses and physicians, many patients report that ulcer care is provided based on personal interest or others’ suggestions. This issue may sometimes even lead to a favorable outcome; however, the infection is exacerbated in many cases.
"Last time, my toes were ulcerated, and I poured dry tea leaf on them because I had heard it was useful, and sometimes I dried ulcers by a hairdryer, which provided acceptable results. However, I have recently tried them several times, the ulcer got deteriorated, and I went to the doctor" (A patient No 7).
4.2. Gradual Access to Outpatient Services
Outpatient services for diabetic ulcer care in clinics, doctors' offices, and even patients' homes are significantly expanding. Referral to CNCSCs is based on the recommendations of the physician and some members of the treatment team, following the initial or even after long-term ineffective ulcer management. Despite the community-based activities of nurses, they do not focus on prevention. Patients and families are not eager for classical education and sometimes refer to web-based information. They are not familiar with nurses' abilities and do not trust them completely.
"I was not familiar with CNCSCs providing care for the ulcer. When I was going to the doctor's office, I saw its sign, but I did not think they could help so much until the doctor referred me to them" (A patient No. 3).
The specialized nursing care centers are gradually developing, and inter-sectorial interactions of health providers are expanding; however, unfamiliarity with other care providers and negative competition slow down this process.
"The work agreement has been formed between nursing centers and some hospitals, but until now, it has not been well implemented…" (a manager of CNCSCs No. 9).
Another point is that hospital admissions for other medical reasons, such as fractures or injuries, sometimes cause inconsistency and negatively impact the ulcer healing process.
"My father was admitted for a fracture of the leg and, because of the focus on the fracture, unfortunately, they (the therapeutic team) neglected to take enough care of the previous ulcer" (A family member No. 4).
Insurance coverage is expanding; however, there exist some problems, especially for new dressing cost coverage, leading to low affordability and dissatisfaction. However, some of these care providers' failure to comply with financial fairness also contributes to this situation.
"Despite its effectiveness and rapid recovery, the new dressing method really does not do it, mainly because it is not covered by insurance as such I sometimes need the family to provide dressing materials" (A nurse No.10).
In some cases, the patient and his/her family do not recognize the legal boundaries of the nurse and the physician’s activities. These ambiguities even lead to problems such as complaints to the court.
"By the advice of one of my relatives, I went to one of the nursing centers. The nurse working there immediately began to debride the ulcer surface using a saw-like machine. After that, I felt the ulcer was getting worsened, and I did not go there anymore. I even wanted to complain about it" (A patient No. 7).
Nursing centers spare efforts to receive advice from physicians and sometimes introduce themselves as technical assistants; however, this cannot completely resolve ambiguous legal problems.
5. Discussion
The findings revealed that low prevention infrastructures and behaviors lead to creating ulcers, inadequate care, delays in referring to specialized centers, and eventually hospitalization. Fortunately, various community-based services have been reinforced in the DU care. Similar to Gitarja’s study in Indonesia (24), developing the role of nurses in new ulcer care methods is effective and promising. However, treatment-oriented approaches, insufficient trust in nurses, and some legal issues negatively influence prevention, referral, and care processes. Smith-Strom et al. found out that timely diagnosis, the rapid pursuit of the healing process, and the referral of patients were critical for diabetic foot ulcer management (37). Our study indicated that patients and families pay not enough attention to ulcer signs, and even after ulceration, they focus on improper self-management in many cases. In line with the present study, Abbas in Africa showed that defective self-medication and late referrals to health care centers were some of the challenges in managing diabetes wound care (25). The low supervision of health care providers on this process usually leads to exacerbated and prolonged treatment. Other studies also show that improper self-management is one of the main causes of inadequate care. Accordingly, self-care and herbal therapy should be done scientifically despite their usefulness. Few adverse effects can be achieved through careful diagnosis and follow-up in the form of primary care and by facilitating timely access to more specialized care services (38).
In contrast to the weakness of outpatient services, hospitalization (39), the improper care management strategy (38), and amputations (40) in developing countries, outpatient services for ulcer care are acceptable in Iran. However, in comparison to developed countries (19), they are slowly going toward team-work formation. Meanwhile, previous studies have indicated that nursing care is mainly based on work experiences (41). Improving nurses' and paramedics' knowledge in the academic and working process is one of the requirements in improving the quality of patient care (42). This issue was emphasized in Abass's study despite poor infrastructures (25).
Participatory approaches and new technologies have effectively established an association between patients and families and physicians and nurses in improving and families' care management abilities (43). Like developed countries, these positive approach would lead to multidisciplinary and preventive approaches in our country (44).
Unlike developing countries (24), insurance coverage is expanding; however, financial interactions are still complicated and accompanied by restrictions such as inadequacy in covering outpatient treatment and medications (45). Accordingly, the transparency of financial transactions and an increase in insurance coverage can effectively increase the affordability of community-based DUC services.
5.1. Limitations
Given the qualitative study method, the generalization of the findings to other care environments and conditions is limited. Furthermore, the lack of access to private hospitals may be another limitation of this study.
5.2. Conclusions
Even though the self-care capacity of patients and families is not at the desired level, the development of the care capacity, especially among nurses, and the use of new care methods are considered as acceptable techniques. However, this situation should be reinforced by creating holistic approaches and applying existing capacities. To achieve optimal and preventive community-based care, there is a need to raise public awareness, improve legal infrastructure, and clarify the professional domain of activities. In addition to the preventive measures, technology and facilities should be utilized for the timely diagnosis, care, and referral of patients.