1. Background
Assessment of head posture is a part of the orthopedic physical examination (1). Poor posture is a risk factor for musculoskeletal diseases (2). Conversely, musculoskeletal balance and minimal stress or strain on the body effectively maintain proper posture (1). One of the popular types of poor posture is forward head posture (FHP) (1), which is considered as a forward projection of the head in the sagittal plane concerning the trunk (3). FHP is common in patients with neck disorders (2). Sitting in front of computers for an extended period can result in FHP (4). The association of FHP with shoulder pain, neck pain, headache, temporomandibular disorders, and cranial and facial pain has been reported (5, 6). Craniovertebral angle (CVA) is one of the most prevalent methods for evaluating FHP (1). CVA examines head position to the seventh cervical vertebra (C7) (7). CVA can indicate the severity of FHP, and previous studies have confirmed its validity and reliability (8, 9).
Some researchers have hypothesized that FHP changes the length and strength of the cervical muscles, shortens the posterior muscles of the neck, and lengthens the anterior muscles of the neck (10). Shortening and elongation of muscle can decrease the muscle’s ability to produce tension (11). Longus colli (LCo) is a vital muscle to control the head and neck (12) and stabilize the neck vertebra (11); it is also one of the muscles affected by FHP (11). Biomechanical changes in FHP may alter the thickness and function of neck muscles.
Muscle thickness measurement can demonstrate the strength and function of the muscle (13). Ultrasonography is considered a cost-effective, reliable, and accessible method to evaluate muscle thickness (14). Some previous studies compared the dimension of LCo in subjects with and without FHP (11, 15, 16).
2. Objectives
However, the relationship between LCo resting muscle thickness and CVA is poorly known. Because of the increased prevalence of FHP and associated musculoskeletal disorders of FHP, the present study aimed to measure the correlation between CVA and resting muscle thickness of LCo in women with and without FHP. The results of the current study can improve knowledge about FHP and lead to better management of FHP.
3. Methods
The present case-control study was conducted on 70 asymptomatic women (age range: 20 - 40 years) at the Biomechanics Laboratory of Rehabilitation Sciences Faculty of Shahid Beheshti University of Medical Sciences, Tehran, Iran, in 2016. The ethical committee approved the study protocols (Shahid Beheshti University of Medical Sciences, code: REC.2015.529, 1/4/2015).
After checking the CVA measured by photographic images, the subjects were assigned into two equal groups (n = 35 each) of FHP and control. Subjects with CVA greater than 48 degrees were assigned to the control group, and those with CVA less than 48 degrees into the FHP group (6).
The exclusion criteria were: radicular pain of upper extremity, neck, or shoulder pain; history of cervical surgery; history of neuromuscular or musculoskeletal disorders; severe thoracic kyphosis; shoulder or neck injuries; history of facial trauma or surgery; participation in sports activity; hearing impairments; prolonged respiratory disorders over the last five years; visual disorders not corrected by glasses; recurrent middle ear infections in the last five years; and disorders of the central nervous system or temporomandibular joint (3). The following formula was used to determine the sample size:
N = (Z1-α/2+z1-β)2 (α12+α22)/(µ1-µ2)2
α: 0.05, β: 0.1, power: 90%, α1: 1.81, α2: 2.34, µ1:2.86, µ2: 4.6 (17).
3.1. Evaluation of CVA
The researcher described the procedures of the study to the subjects, and all participants signed an informed consent form prior to data collection. The demographic data were collected, and a digital camera (Sony, DSC WX80, Japan) was used to measure the neck and head posture. A digital camera was on a fixed base at a distance of 1.5 m from the subjects. The height of the camera was to the level of the subject’s shoulder (18). The subjects were standing in a natural standing position feeling comfortable while distributing body weight evenly between feet and °maintaining this position (18). A self-balanced position was used to standardize neck and head posture. For this purpose, the subjects moved the neck and head into full extension and flexion, and gradually reduced movement until full stop of the movement. Subjects maintained the habitual posture of the neck and head (18).
For measuring CVA, the C7 spinous process and tragus of the ear were marked. Three pictures from the lateral view of each side of the subjects were taken to assess FHP. The CVA was calculated using Image J tools. The point between the horizontal line passing through C7 and a line amplifying from the ear’s tragus to C7 was calculated (1). If both sides’ average CVA was less than 48°, the subject was assigned to the FHP group (6). Since previous studies considered CVA less than 48° - 50° as FHP, we considered CVAs less than 48° as FHP (6).
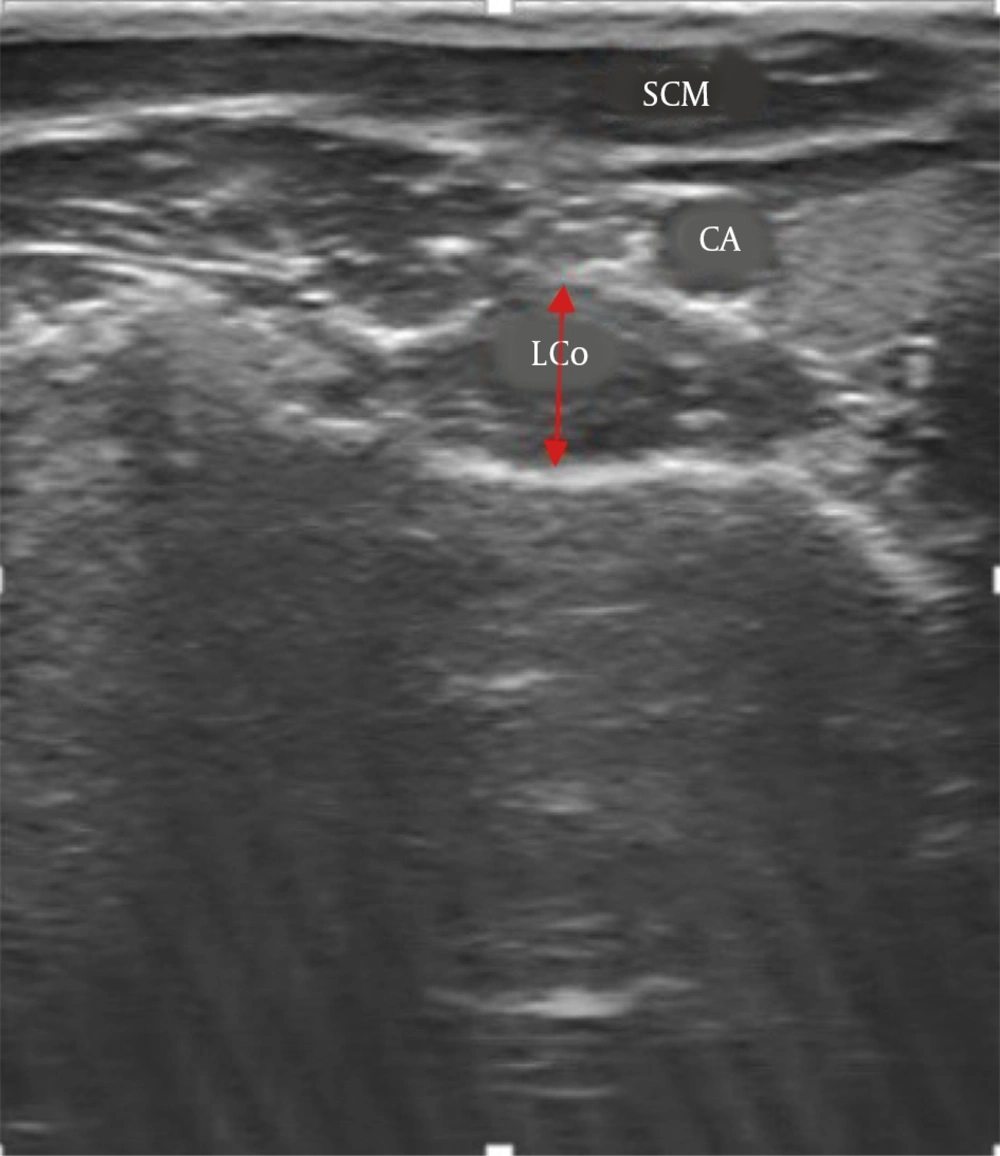
3.2. Ultrasonography of LCo
Images of LCo muscle were taken by B-mode 7.5 MHz ultrasonography (Ultrasonic scanner, HS 2100, Honda Electronic Co., Japan) with a linear probe (7 cm). The subjects were sitting in the relaxed state on a chair, while knees and hips were at 90° flexion, neck and head were in the neutral position, arms were in the resting position by sides, and hands and forearms were on the thigh. Since the position change of subjects during ultrasonography could alter muscle thickness, the position of subjects was monitored during ultrasonography. For visualizing LCo muscle, the probe was placed transversely at the level of the sixth cervical vertebra. Three images of LCo were captured. For obtaining each image of LCo, the probe of ultrasonography was removed from the skin and repositioned (18). Subjects were right-handed, and LCo images were taken on the right side of subjects (Figure 1). The thickness of the LCo was measured using ultrasonography on each image. For thickness measurement, we did not include the facial outline. A cursor was placed on the inside edge of the superior fascia at the thickest portion of the muscle. Then a vertical line was drawn to the inside edge of the inferior fascia (19). The average thickness obtained from three ultrasound images was used for statistical analysis.
3.3. Statistical Analysis
Data were analyzed using SPSS software version 16. The normality of the variables was checked using the Shapiro-Wilk test. The independent sample t-test and the Mann-Whitney test were used for variables with and without normal distribution, respectively. The correlation coefficient was calculated for assessing the relationship between CVA, demographic data, and LCo thickness. A P-value < 0.05 was considered as significant.
4. Results
Table 1 represents the demographic data, CVA, and thickness of LCo in both groups, and Table 2 shows the correlation between them. Our results indicated a non-significant correlation between CVA, demographical data, and thickness of LCo between the two groups.
| Variable | Mean (SD) | Confidence Interval | P-Value |
|---|---|---|---|
| Age, y | 0.89 | ||
| Control | 25.18 (5.52) | -2.32 - 2.67 | |
| FHP | 24.94 (5.13) | ||
| Height, m | 0.87 | ||
| Control | 1.63 (0.04) | -0.028 - 0.02 | |
| FHP | 1.63 (0.06) | ||
| Weight, kg | 0.76 | ||
| Control | 60.72 (10.09) | -4.09- 5.18 | |
| FHP | 60.17 (9.35) | ||
| BMI, kg/m2 | 0.81 | ||
| Control | 22.81(3.7) | -1.53 - 1.95 | |
| FHP | 22.6 (3.59) | ||
| CVA, degree | 0.000 | ||
| Control | 54.26° (1.88°) | 9.68 - 11.33 | |
| FHP | 43.76° (1.55°) | ||
| LCo | 0.8 | ||
| Control | 12.82 (2.46) | -1.08- 1.4 | |
| FHP | 12.67 (2.75) |
Abbreviations: BMI, body mass index; CVA, craniovertebral angle; FHP, forward head posture; LCo, longus colli; SD, standard deviation.
| Variable | Group | Age | Height | Weight | BMI | Thickness of LCo |
|---|---|---|---|---|---|---|
| CVA | FHP | -0.12 (0.49) | -0.01 (0.9) | 0.1 (0.56) | 0.04 (0.74) | 0.02 (0.82) |
| CVA | Control | -0.15 (0.36) | 0.06 (0.7) | 0.07 (0.65) | 0.03 (0.83) | -0.001(0.9) |
Abbreviations: BMI, body mass index; CVA, craniovertebral angle; FHP, forward head posture; LCo, longus colli.
5. Discussion
As far as the researchers of this study investigated, there is no study to evaluate the relationship between CVA and LCo thickness in women with FHP. Forward translation of head in FHP may result in the smaller thickness of LCo compared to the control group. No significant relationship was observed between resting muscle thickness of LCo and CVA in women with FHP, meaning that a lower CVA or higher FHP is not correlated with a lower resting muscle thickness of LCo.
The present study targeted only women with a moderate degree of FHP (mean CVA: 43.76°), and FHP might not lead to morphological changes in these subjects as expected, which may justify the non-significant correlation between CVA and resting muscle thickness of LCo. Change of resting muscle thickness of LCo may be a late consequence of FHP or appear in subjects with chronic or severe degrees of FHP. This insignificant association can also be attributed to the subjects’ lack of pain, because pain can lead to muscle atrophy (11).
Since postural testing is an essential aspect of the clinical diagnosis techniques for cervical pain, in this report, the investigators concentrated on one of the abnormal postures (1). Sitting tasks and flexed spine posture in computer and desk work have increased in most working environments, and these postures may induce FHP (1). Also, there is a correlation between neck posture and disability in cervical disorders. Postural correction should be considered as an essential part of managing and preventing neck pain (12).
In the present study, the authors used CVA to assess FHP because this angle is widely used for objective measurement of FHP (1). Moreover, we measured CVA in a standing position to eliminate the thoracolumbar spine’s effects on the cervical spine’s posture. Other parts of the spine’s posture can influence CVA in the sitting position, resulting in confusion with the FHP (1). The mean value of CVA in standing position was 54.26° in women without FHP, which was consistent with the results of some previous studies (1, 6).
We measured the resting muscle thickness of the LCo because this muscle is an essential muscle for adjusting and maintaining the posture of the cervical spine (12), and it has a primary postural function for controlling the intervertebral motion of the cervical spine (1).
Since no studies have evaluated the correlation between CVA and resting muscle thickness of LCo in FHP, it was impossible to compare the findings of the current study with some previous studies. Ishida et al. (12) evaluated the correlation between neck slope angle and thickness of deep cervical flexor (DCF) muscles in 42 healthy males. CVA was measured in a sitting position, and the thickness of DCF muscles was assessed in a supine position. According to the findings, there was a moderate positive correlation between muscle thickness and CVA, and subjects with lower CVA had smaller muscle thicknesses (12). The results of the current study in the control group were inconsistent with the results of Ishida et al. This discrepancy can be due to the ultrasonography and CVA measurement locations. The present study used a sitting position for ultrasonography and a standing position for CVA evaluation, while their study used a supine position for ultrasonography and a standing position for CVA evaluation.
In another study, Subbarayalu et al. studied the relationship between pain intensity, disability, CVA, and performance of DCF muscles in 84 patients with postural neck pain. The results revealed a very weak and positive correlation between CVA and DCF muscles’ performance (2).
According to the results of the current report, there was no significant correlation between CVA and demographic data between the two groups. This finding is not consistent with the results of a study conducted by Shaghayegh Fard et al. (1), which indicated a significant inverse correlation between CVA and body mass index (BMI) in a standing position. This inconsistency might be related to the gender of participants because the subjects of the current study were only women, while Ahmadi et al. included both men and women.
Although our study is the first report to evaluate the relationship between CVA and thickness of LCo in women with FHP, like any scientific research, it had some limitations. First, since the current study was done on asymptomatic women with a moderate degree of FHP, the findings may not be generalized to men with FHP or women with more severe degrees of FHP, or symptomatic women with FHP. Second, the present study only measured the correlation between CVA and resting muscle thickness. Further research is needed to evaluate the correlation between CVA and the thickness of LCo during muscle contraction. The correlation between CVA and strength or endurance of LCo muscle in subjects with and without FHP can also be investigated. Further research is needed to evaluate the correlation between CVA and the thickness of LCo during muscle contraction. The correlation between CVA and strength or endurance of LCo muscle in subjects with and without FHP can also be investigated. Other studies can also be designed to evaluate the correlation between CVA and thickness of LCo in different degrees of FHP. Similar studies can also be conducted on symptomatic FHP patients with neck pain and headache.
5.1. Conclusions
According to our results, a lower CVA is not correlated with the smaller thickness of LCo muscle.