1. Background
Carpal tunnel syndrome (CTS) is among the most common peripheral neuropathies causing the median nerve to compress when crossing the carpal tunnel, with an estimated prevalence of about 4 - 5% of the population. Patients suffering from this syndrome mainly complain about paresthesia (pain, numbness, and tingling) in the innervation area of the hand median nerve which could be accompanied by the weakness and atrophy of thenar muscles (1).
The conservative treatment for patients suffering from mild and moderate CTS includes medical treatment, resting splints, and physiotherapeutic methods such as laser therapy, ultrasound therapy, mobilization, and massage therapy. There are contradicting results about the effectiveness of physiotherapeutic treatments, and the best treatment for CTS patients is yet to be specified (2, 3). Among the conservative treatments, laser therapy and ultrasound therapy have the potential to leave biophysical impacts on the nerve tissue (4, 5) and can facilitate the reconstruction of the damaged nerve according to experimental evidence (6, 7). Several clinical trials have reported ultrasound therapy to have beneficial impacts on CTS treatment (8-10). A Cochrane review study has concluded that there is insufficient evidence determining whether ultrasound therapy is more effective in treating CTS compared to placebo or other non-surgical interventions (11), and further research is required to compare the therapeutic effects of ultrasound and other modalities on CTS patients.
Low-level laser therapy (LLLT) is a physiotherapy modality used to treat peripheral nervous damages due to its analgesic and anti-inflammatory effects (12). The efficiency of LLLT in treating CTS was first investigated by Pauda (13) and Weintraub (14); however, neither of these studies had a control group. Afterward, many clinical trials examined the efficiency of LLLT in CTS patients, some of which reported beneficial effects for LLLT in treating CTS (12), while others found no positive impacts (15). A systematic review conducted in 2018 concluded that LLLT is more effective in treating CTS compared to placebo in the short term (16). One of the most recent meta-analysis studies conducted in 2020 has reported that adding low-level laser to splints exerts no significant impact on relieving hand pain and improving its functions compared to the use of splint alone; thus, low-level laser is not suggested to be used alongside splints for treating CTS patients (17).
Few studies have compared the impacts of ultrasound therapy and laser therapy on the treatment of CTS so far. Bakhtiary and Rashidy-Pour (8) and Saeed et al. (18) reported that both ultrasound and laser therapies indicated improvements in the symptoms and hand function of mild and moderate CTS patients, but ultrasound therapy was more influential than laser therapy. In another comparative study, Ahmed et al. (19) reported that both ultrasound and low-level laser were influential in treating mild and moderate CTS patients, and no significant difference was observed between these two modalities.
According to the results mentioned above, both ultrasound and laser modalities have beneficial effects on improving CTS symptoms through various mechanisms. Thus, it would appear that the application of both these modalities together could have a further positive impact on the treatment of CTS patients. No study has investigated the compound effect of these two modalities so far.
2. Objectives
The present study aimed to compare the effects of ultrasound and laser therapies separately and together on pain relief and hand function improvement in mild and moderate CTS patients.
3. Methods
3.1. Study Design
The present study was a single-blind clinical trial with registration number IRCT20190202042581N1. The population included all CTS patients (male and female) referred to the Physiotherapy Clinic of the Rehabilitation Faculty, Hamadan University of Medical Sciences (Iran) from May 2019 to September 2020. The patients were selected from those meeting the inclusion criteria after providing them with the required explanations and obtaining signed consent forms if they agreed to participate. The study acquired the ethical approval of Hamadan University of Medical Sciences, and all the participants entered the study voluntarily and after signing the consent form.
3.2. Participants
The inclusion criteria were being aged 20 - 60 years and having been diagnosed with chronic mild or moderate CTS by a specialist according to clinical results and electrophysiological criteria (The mild type only involves the sensory fibers with no motor fiber involvement, provided that the sensory wave is not absent, i.e. sensory peak latency > 3.6 milliseconds and motor onset latency < 4.1 milliseconds; the moderate type involves both sensory and motor fibers, provided that neither of these two waves is absent, i.e. sensory peak latency > 3.6 milliseconds and motor onset latency > 4.1 milliseconds). The exclusion criteria were suffering from severe CTS according to electrophysiological criteria, the presence of a secondary neuropathy, double-crush syndrome, cervical radiculopathy, thoracic outlet syndrome, previous treatment report of the syndrome by laser or ultrasound, consumption of anti-inflammatory or analgesic medication, history of steroid injection in the carpal tunnel, and diseases associated with thyroid, diabetes, or nervous system neuropathy.
3.3. Procedure
The sample size of the trial was estimated based on the change in hand pain intensity measured by VAS in the study by Saeed et al. (18) with an 80% power and an (α) error of 5%. The mean ± standard deviation of VAS in the ultrasound and laser groups was 4.9 ± 1.46 and 2.6 ± 1.07, respectively. The calculation revealed that a minimum of 15 participants was needed for each group. A total of 45 CTS patients meeting the inclusion criteria were recruited. After they completed the consent form, the participants were divided randomly into three groups of laser therapy (15 patients), ultrasound therapy (15 patients), and a combination of laser and ultrasound therapies (15 patients) using simple random allocation based on a random number table. Patients with bilateral CTS had both hands placed in the same group, and the intervention was the same for both hands. The evaluations were performed separately for the two hands All the participants' anthropometric characteristics such as sex, age, height, weight, the affected hand, and the duration of CTS were collected. The blinding method was as follows: The person measuring the outcome parameters and conducting the statistical analyses had no information of sample groupings, while the patients and the physiotherapist delivering the treatments knew about the groups. For the ultrasound group, pulsed ultrasound with an effective radiation area (ERA) of 5 cm2 (P210 Novin ultrasound device, Novin Medical Engineering Company, Iran) was applied on the wrist canal area (20% duty cycle) with a frequency of 1 MHz and intensity of 1.2 W/cm for five minutes per session (20). For the laser therapy group, infrared diode laser (86X Novin low-level laser, Novin Medical Engineering Company, Iran) with an 808nm length, 500 mW output power, and total intensity of 9 J was applied on five points along the median nerve in the wrist canal area (8). For the ultrasound and laser compound therapy group, laser was applied in the same way as that applied for the laser therapy group, immediately followed by ultrasound with parameters identical to the ultrasound therapy group. The patients in all three groups went through 10 therapy sessions (five days per week). All the patients were prescribed resting splints to be used at night, and could receive no other therapy during the course of the study. The evaluated parameters included pain intensity, the strength of pressing something between the thumb and the index finger (pinch grip), handgrip strength, symptom severity, and the functional state of the hand.
3.4. Measurement of Pain Intensity
The visual analog scale (VAS) was used to evaluate pain intensity. The patients were asked to specify the highest level of discomfort and pain in their finger and hand on the 10-cm analog scale.
3.5. Measurement of Pinch and Handgrip Strengths
Pinch grip and handgrip strengths were measured using a dynamometer (Model SH-5003, SAEHAN Company, South Korea). To measure pinch grip and handgrip strengths, the patients were asked to sit down, and the mean pressure generated in three attempts was calculated and recorded (8). In the dynamometer reproducibility test, the result of intraclass correlation coefficient (ICC) using Munro table (very low: 0.00 - 0.25; low: 0.26 - 2.49; medium: 0.50 - 0.69; good: 0.70 - 0.89; and excellent: 0.90 - 100) showed excellent reproducibility. Studies have indicated that the validity and reliability of the SAEHAN dynamometer are high, and it is considered to be the gold standard for assessing handgrip strengths (21).
3.6. Measurement of Symptom Severity and Functional Status Scales
The Boston Questionnaire (BQ) was employed to evaluate symptom severity and the hand's functional status. The BQ consists of two sections, the first including 11 questions evaluating pain intensity, and the second comprising eight questions assessing the functional status. The validity of the English version of BQ has been confirmed by Levine et al. (22). Each question has five options, ranked from 1 to 5, with 1 indicating the absence of symptoms and 5 indicating the most severe symptoms. The average score of the first 11 questions was recorded as the pain intensity score, and the average score of the last eight questions was recorded as the functional status, with higher scores demonstrating severer symptoms or greater disability. The validity of the Persian version of BQ was confirmed by Rezazadeh in 2014 (23). All the evaluations were performed before the first and after the last therapy session.
3.7. Statistical Analysis
SPSS 16 was used for data analysis. One-sample Kolmogorov-Simonov test indicated that all the studied variables in all three groups were distributed normally (P > 0.05). Hence, one-way analysis of variance (ANOVA) and Tukey's post-hoc test were performed for data comparison across the groups, and a paired t-test was run to compare the data within each group. The significance level was considered as P < 0.05.
4. Results
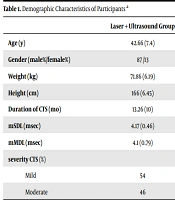
The present study evaluated 84 wrists from 45 patients suffering from CTS (six patients with unilateral and 39 patients with bilateral CTS) who remained in the study unit to the end. Table 1 presents the demographics of the participants. All three groups were compared in terms of demographics, electro-diagnostic indicators, and other variables before treatment, which indicated no significant difference between them (P > 0.05); thus, all three groups were similar in this regard.
| Laser + Ultrasound Group | Laser Therapy Group | Ultrasound Therapy Group | P Value | |
|---|---|---|---|---|
| Age (y) | 42.66 (7.4) | 46.13 (7.7) | 39.7 (10.7) | 0.1 |
| Gender (female%/male%) | 87 /13 | 87/13 | 87 /13 | 0.3 |
| Weight (kg) | 71.86 (6.19) | 76.33 (6.9) | 67.73 (8.58) | 0.1 |
| Height (cm) | 166 (6.45) | 167.5 (5.6) | 165.64 (7.5) | 0.7 |
| Duration of CTS (mo) | 13.26 (10) | 14.46 (11.16) | 13.42 (15.96) | 0.6 |
| mSDL (msec) | 4.17 (0.46) | 4.07 (0.72) | 4.05 (0.57) | 0.8 |
| mMDL (msec) | 4.1 (0.79) | 3.88 (0.66) | 4.3 (0.9) | 0.2 |
| severity CTS (%) | ||||
| Mild | 54 | 54 | 54 | 0.1 |
| Moderate | 46 | 46 | 44 | 0.1 |
Demographic Characteristics of Participants a
There were no significant differences in the dependent variables among groups before the therapy sessions, as presented in Table 2 (P > 0.05). A comparison of the parameters within each group indicated significantly improved pain severity in all three groups of ultrasound and laser combination therapy (P = 0.000), laser therapy (P = 0.000), and ultrasound therapy (P = 0.000) by the end of the 10th session. Besides, pinch grip strength (P = 0.000, P = 0.002, and P = 0.004, respectively) and handgrip strength (P = 0.003, P = 0.01, and P = 0.004, respectively) significantly increased in all three groups after invention, suggesting improved hand grip and pinch grip in all groups. Examination of the two variables measured via the BQ, including symptom severity and hand functional status, revealed that these variables significantly dropped after the intervention (P < 0.05) in all three groups, which shows a decrease in symptoms severity and functional hand disability (Table 2).
| Variables | Laser + US | Laser | US | P Value |
|---|---|---|---|---|
| Hand grip (kg) | ||||
| Baseline | 40.8 (10.3) | 51.3 (30.1) | 37.6 (11.9) | 0.3 |
| Final | 49.6 (17.7) | 56.03 (38.9) | 42.7 (9.2) | 0.2 |
| P value | 0.003 | 0.01 | 0.001 | |
| Pinch grip (kg) | ||||
| Baseline | 10.2 (5.2) | 12.02 (5.2) | 10.2 (3.8) | 0.3 |
| Final | 13.2 (5.6) | 13.8 (5.2) | 11.6 (3.9) | 0.3 |
| P value | 0.000 | 0.002 | 0.004 | |
| VAS | ||||
| Baseline | 7.1 (1.3) | 6.6 (1.7) | 6.7 (1.1) | 0.4 |
| Final | 3.6 (2.3) | 3.4 (1.1) | 3.7 (1.5) | 0.1 |
| P value | 0.000 | 0.000 | 0.000 | |
| SSS | ||||
| Baseline | 39.8 (9.3) | 38.2 (9.5) | 37.07 (7.4) | 0.7 |
| Final | 22.2 (11.5) | 19.9 (6.3) | 20.3 (7.4) | 0.2 |
| P value | 0.000 | 0.000 | 0.000 | |
| FSS | ||||
| Baseline | 28.3 (9.7) | 26.1 (9.6) | 27.4 (8.2) | 0.8 |
| Final | 16 (9.07) | 14.8 (5.7) | 15 (7.6) | 0.1 |
| P value | 0.000 | 0.001 | 0.000 |
Comparison of Variables Within Each Group; Before and After Treatment a
Although the mean changes in pain intensity, pinch grip, handgrip, symptom severity, and functional status were higher in the ultrasound and laser combination therapy group compared to the two other groups (laser therapy and ultrasound therapy), a comparison of the mean values of the parameters across the three groups (Table 3) indicated no statistically significant difference among them (P > 0.05).
| Variables | Laser + US | Laser | US | P Value |
|---|---|---|---|---|
| Hand grip (kg) | 8.7 (13.7) | 4.7 (8.1) | 5.1 (6.8) | 0.2 |
| Pinch grip (kg) | 2.9 (2.2) | 1.8 (2.7) | 1.3 (2) | 0.06 |
| VAS | -3.4 (1.8) | -3.2 (1.9) | -2.9 (1.3) | 0.6 |
| SSS | -17.5 (9.9) | -18.2 (10.9) | -16.7 (7.3) | 0.6 |
| FSS | -12.33 (8.4) | -11.3 (10.3) | -12.4 (5.1) | 0.9 |
Comparison of Mean Changes from Baseline Values Between the Three Groups a
5. Discussion
There are several medical interventions for CTS treatment, but there is still no agreement regarding the best treatment method (3, 24). The present study sought to compare the results of laser and ultrasound therapies separately and together in treating patients suffering from mild and moderate CTS. The results revealed that the parameters of pain intensity, handgrip strength, pinch grip strength, and the BQ score (evaluating symptom severity and hand functional status) significantly improved in all three groups after the intervention; however, no significant difference was observed between the groups despite the higher improvements observed in the ultrasound and laser combination therapy group. These results indicate that both laser and ultrasound therapies are effective in improving the symptoms and hand function of patients suffering from CTS, and none is favored over the other. However, the combination of these two treatment methods may be more effective in improving patients’ symptoms and their hand function.
The results observed in the ultrasound group are consistent with those of previous research (11, 21). According to Page et al. (11) and Ansar et al. (20) regarding the impact of pulse ultrasound and corticosteroid injection, four weeks of ultrasound resulted in significantly higher hand strength and symptom improvement in CTS patients compared to corticosteroid injection. Furthermore, Oztas et al. (25) reported that continuous ultrasound with various intensities (0.8 and 1.5 mW/cm2) has a significant impact on the improvement of patient's symptoms and median nerve conduction velocity. Given that pulse ultrasound has anti-inflammatory and mechanical impacts compared to continuous ultrasound, the difference between this and the present study could be due to the type of ultrasound used. The present study utilized pulse ultrasound which has anti-inflammatory and mechanical effects, while Oztas employed continuous ultrasound that has thermal but no anti-inflammatory influence (26).
The results observed in the laser therapy group are consistent with the studies by Lazovic et al. (27), Jiang et al. (28), Chang et al. (15), Tascioglu et al. (29), and Evcik et al. (30). These studies have reported that low-level laser results in significantly better pain relief and symptom improvement in CTS patients compared to placebo. On the contrary, Cheung et al. (17) reported in their systematic review that both low-level laser and resting splints were effective in reducing CTS symptoms, while low-level laser did not yield better results regarding pain relief, symptom improvement, and hand function compared to splints. The existence of different results regarding the impact of laser therapy in treating CTS may be due to the use of a wide range of laser parameters such as laser power, wavelength, duration of radiation, and application area, and agreement on the most influential laser parameters for treating CTS is yet to be achieved.
Although both interventions used in this study (ultrasound and laser therapies) had beneficial effects on CTS treatment, a comparison of the two groups' results indicated no significant difference between these two interventions for CTS symptom improvement. In other words, both laser and ultrasound therapies are effective in improving the symptoms and hand function of patients suffering from CTS, and none is favored over the other. These findings are consistent with the results of Bakhtiary and Rashidy-Pour (8) who compared the therapeutic effects of low-level laser and ultrasound in CTS patients. One group went through 15-minute ultrasound therapy sessions of pulsed ultrasound with the intensity of 1w/cm2 and the frequency of 1 MHz on the carpal tunnel, whereas the other group went through laser therapy sessions with a wavelength of 830 nm and total intensity of 9 J along the median nerve. Both therapies were effective, but ultrasound therapy led to significantly better results in improving CTS symptoms compared to laser therapy. Our study indicated that both ultrasound and laser therapies are effective, but the lack of a significant difference between the two treatment methods (as that reported by Bakhtiary and Rashidy-Pour) might be due to the number of sessions and duration of ultrasound; 15 minutes of ultrasound along the carpal tunnel for 15 sessions was used in Bkhtyari’s study, but five minutes of ultrasound for 10 sessions was used in our study. A comparative study conducted by Ahmed et al. (19) examined the impact of ultrasound and low-level laser in the treatment of CTS patients, and their findings were consistent with ours. They used a wavelength of 904 nm, power of 20 mW, and total energy of 4.8 J along the median nerve for laser therapy, and pulse ultrasound with a frequency of 1 MHz and intensity of 1 W/cm2 for 15 minutes on the carpal tunnel for ultrasound therapy. Both low-level laser and ultrasound modalities were effective in treating patients suffering from mild and moderate CTS, and there was no significant difference between the two methods of treatment. Recently, Rayegani et al. (31) conducted a meta-analysis on the impact of laser and ultrasound therapies on treating CTS patients and compared the two treatments. According to them, a significant difference was found between the two methods, and both methods resulted in similar impacts on the improvement of CTS symptoms.
To the best of our knowledge, no study has yet examined the impact of the combination of laser and ultrasound therapies in treating CTS, and the present study concluded that the combination of these two modalities may be more effective in treating CTS patients compared to using each of them individually. However, no statistically significant difference was observed. In this study, all the variables were evaluated immediately after the last session. Since the therapeutic effects of the interventions performed may appear a few weeks after the end of the treatment, the lack of follow-up may explain the non-significant differences between the three groups. In addition, the lack of significant results across groups may be due to the small sample size; thus, subsequent studies are recommended to recruit a larger sample.
The exact mechanism of ultrasound and low-level laser's beneficial impacts in treating CTS is yet to be known. According to the findings of previous research (6, 7), ultrasound can stimulate the tissue and leave anti-inflammatory effects. Thus, the mechanism of ultrasound's therapeutic impacts on CTS symptoms could be associated with reducing the pressure inside the carpal tunnel, alleviating the inflammation around the nerve, and accelerating damaged tissue recovery given the CTS pathophysiology (32-34). Regarding low-level laser, there is evidence suggesting that it relieves pain and reduces inflammation locally by stimulating microcirculation, blocking pain enzymes, and activating endorphin enzymes (35-37). Therefore, the beneficial effects of low-level laser in treating CTS symptoms appear to be associated with its analgesic and anti-inflammatory effects. It seems that the simultaneous use of both these modalities on the carpal tunnel can activate the mechanisms related to each modality in this area. Therefore, a combination of laser and ultrasound may exert a cumulative effect, producing an even more effective treatment regime and superior and longer improvement. However, more studies are required on the mechanisms of ultrasound and laser combination. The simultaneous application of these modalities may induce a greater effect on pain relief and improvement of CTS symptoms through two distinct mechanisms, as observed in this study.
5.1. Limitations
It was not possible to have a control group due to ethical considerations. Hence, future studies are recommended to be conducted with a larger sample, more therapy sessions, follow-up, and recording the electromyographic data.
5.2. Conclusions
Overall, although ultrasound and laser therapies could each be effective in reducing the pain and improving the functional performance of mild and moderate CTS patients over the short term, the combination of these two modalities in each therapy session may have a better impact on treatment. However, further studies are required to discover the long-term impacts and the durability of the effects of these two modalities and their combination.