1. Background
Osteoarthritis (OA) is the most common musculoskeletal disorder, affecting almost half of individuals aged more than 65 years in the world (1-3), Resulting in pain of the knee joint and reducing ability to do daily activities (4, 5). One of the conservative knee OA treatments is exercise therapy (6, 7) to reduce pain and improve general mobility and joint function. More intensive exercises can strengthen the muscle around the knee joint with an effective, safe, low-tech, and low-cost treatment available for numerous patients (8).
Adherence in traditional exercise programs is always challenging for therapists, with the effectiveness depending on some factors, including the exercise protocol and patient participation (9). Despite the effect of exercise and exercise therapy on the physical and social health of the elderly with disabilities, participating in exercise and exercise therapy is still weak among them (10, 11). Campbell et al. showed that noncompliance with the practice of physiotherapy is common. From the patient’s perspective, decisions about whether or not to comply are rational but often cannot be predicted by therapists or researchers (12). Less participation in doing exercises and therapeutic exercises might correlate to general factors, such as fear of adverse consequences and lack of motivation (10, 11).
Using supervised exercise sessions, referring for regular consultation with a physician, or attending group exercise classes might help ensure long-time exercise compliance and improve therapeutic outcomes (13). Referral of patients to clinics or group sessions to do therapeutic exercises is cost- and time-consuming and is not always available for elderly patients (14, 15). Regarding the importance of health protocols in the coronavirus disease 2019 (COVID-19) epidemic, especially for the elderly, a method is required to do therapeutic exercises at home without attending medical centers (14). According to other recent studies, telerehabilitation shows a positive impact on patients’ compliance and adherence (16, 17) as the patients’ opinions are important (18). This trial contributes to the scientific-based knowledge regarding the effects of telerehabilitation and increase in participation.
Complicating and challenging exercises lead to a lack of adherence to treatment (19). Increasing the strength of muscles often leads to training simple muscle strength of the quadriceps. Personalizing exercise programs reportedly correlates with high adherence rates (20). For the achievement of maximum patient adherence, personalizing exercise components for a patient with OA in the knee might lead to increasing the adherence rate and the strength of quadriceps muscles.
2. Objectives
The present study aimed to develop a tool based on tracking movement therapy patterns and to increase the rate of participation in therapeutic exercise (ie, patients with OA of the knee do their therapeutic exercises with high attractiveness under the practices and standards considered by a therapist at home). Moreover, this tool is a four-exercise pattern on a map through which participants trace exercise patterns predetermined by the therapist through a light diffuser (or laser light) at home, causing the users to do therapeutic exercises correctly without attending medical centers.
3. Methods
3.1. Instrument Design
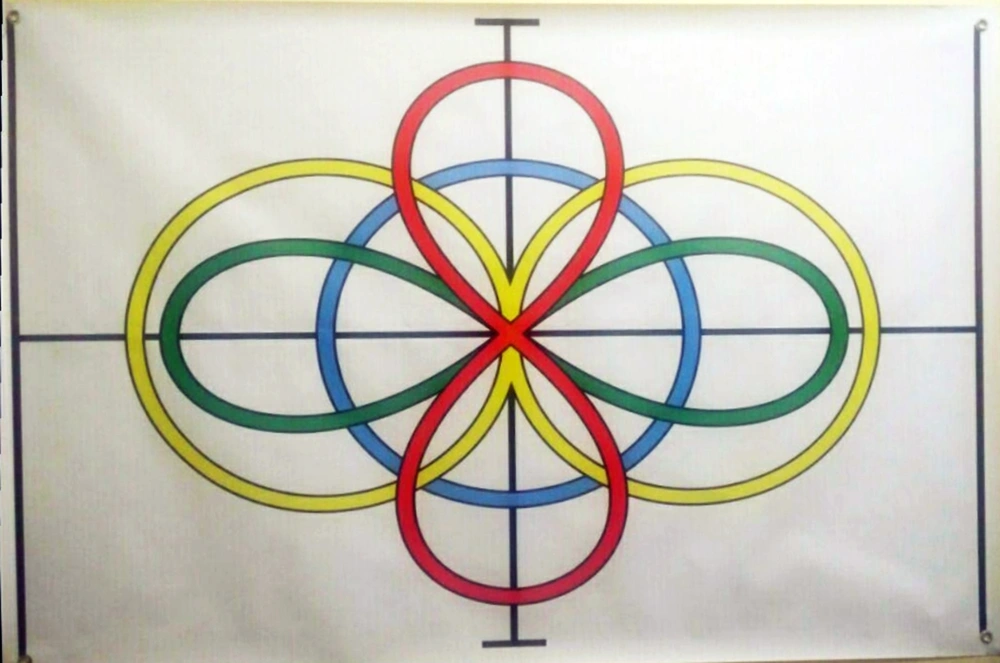
In this pilot study, tracing therapeutic movement patterns using laser light was an invention (registration no.: A61B 5/00). The first part of the tool included four movement patterns designed on a map with a length and width of 1 and 1.5 meters, respectively. A black plus sign (+) divided the screen into four equal parts (Figure 1) that all patterns crossed and intersected the center of the screen. The width of all designs was 2.5 cm. For easier separating, the patterns were classified with color as follow:
(1) Visible in yellow and resembled the Latin number 8 horizontally with an overall size of 114 and 53 cm
(2) A red section corresponding to the Latin number 8 with an overall length of 82 cm and a width of 36 cm
(3) Two green oval shapes with an overall size of 104 and 29 cm
(4) The last pattern designed in the blue circle located in the center of the screen with its longitudinal and transverse diameters as 53 and 58 cm, respectively
The second part of the tool included a light diffuser (laser light) with a strap, a rechargeable battery, an on/off switch, and a light outlet. In addition, the light diffuser diameter, length, and width were about 8, 6, and 3 cm, respectively (Figure 2). A strap attached to a light diffuser could fit the instrument to the patients’ knee at different parts of the patients’ limb, such as the head, hands, knees, pelvis, and ankles.
3.2. User-Centered Usability Testing
Based on the International Organization for Standardization ISO standard, usability is considered the use of the product to achieve particular goals, effectiveness, efficiency, and satisfaction by special users in a particular context (21). In the current study, one of the most critical steps was usability testing to collect empirical data by users and learn about the usage, efficiency, tool durability, and safety (22), helpful in identifying problems with existing tools, even with a small number of participants. According to Nielsen, a usability testing of five users should identify up to 80% of potential problems with a particular tool (23, 24). Williams stated that the level of patients’ satisfaction could show the quality of a tool (ie, higher quality leading to higher patient satisfaction) (25).
3.3. Study Design and Participants
This pilot study was conducted at Shahid Beheshti University of Medical Sciences, Tehran, Iran (ethics code: IR.SBMU.RETECH.REC.1399.340), and all participants gave their written consent. A total of 16 patients, including 9 female and 7 male subjects, suffering from medial compartment knee OA were recruited from orthopedic clinics in Tehran. The participants were selected based on convenience and nonprobability sampling methods. The inclusion criteria were the age range of 50-65 years, grades 2 and 3 knee OA based on the Kellgren-Lawrence classification (26), knee pain due to knee OA with a score of more than 4 according to the VAS (Visual Analogue Scale) for at least 3 months, and indication for therapeutic exercises. The exclusion criteria were the exacerbation of symptoms, anti-inflammatory drugs during the study, and hip joint OA. Table 1 shows the subjects’ age, weight, height, and pain intensity before each intervention in each group.
| Variables | Groups | P-Value | |
|---|---|---|---|
| Control Group | Intervention Group | ||
| Age (y) | 58.2 ± 8.07 | 60.1 ± 5.28 | 0.74 |
| Weight (kg) | 87.4 ± 11.04 | 82.8 ± 6.16 | 0.20 |
| Height (cm) | 163.7 ± 8.92 | 161.8 ± 13.68 | 0.47 |
| Pain before intervention (score) | 6 ± 0.75 | 5.5 ± 0.48 | 0.65 |
| Kellgren-Lawrence score | |||
| Stage II | 55% | 45% | 0.05 |
| Stage III | |||
a Values are expressed as mean ± standard deviation unless otherwise indicated.
Outcome measures included the range of motion (ROM) of the knee joint in the sagittal plane, assessment of pain intensity, and participants’ satisfaction with the treatment. In addition, the participants were randomly divided into control and intervention groups.
3.4. Intervention
The prescribed exercises should be done at home by the groups. Accordingly, the control group follows the common home rehabilitation recommendations and exercise autonomously, and the experimental group patients use the tool to do their exercises; both groups have the same pattern of exercise. In both groups, the exercises are supposed to be done at home under the supervision of an online physiotherapist. Due to pandemic COVID-19, follow up sessions were performed online by physical therapist after one face to face training session. The rehabilitation program duration per patient is 4 weeks (30 days) (27). The purpose of these exercises was to strengthen the quadriceps muscles and stretch the hamstrings (28). The participants should have three 60-second stretches with 60 seconds of rest between stretches on the hamstring muscle group (29).
3.4.1. Control Group
The control group (n = 8) did the conventional exercises for 4 weeks with conventional practices, such as static stretching (30) and straight-leg-raise (SLR) exercises, done in the supine position. The lower limb was raised and stayed by the patient with a straight knee for 10 seconds and then returned to the initial position (31). In the first stage, the participants did static stretching exercises with a 5-minute rest and repeated the SLR exercise 30 times. Activities lasted for 20 minutes, and the participants performed exercises every day for 4 weeks.
3.4.2. Intervention Group
The intervention group (n = 8) did stretching exercises using the instruments of the physical therapist in a nonweight-bearing position for 4 weeks. The patients received a map pattern, a knee strap, and a light diffuser and did 15-minute exercises every day for 4 weeks with the tool attached to their knees. Additionally, the participants attached the laser under the patella with a strap and map pattern on a wall, lying on a soft mattress 2 m from the map. They also performed the exercises in two stages as follows:
(1) The participants did static stretching exercises with tracing red and blue patterns; since the blue pattern was shorter than the red one, the blue and red patterns were traced for 60 seconds three times with a 60-second rest between stretches, respectively.
(2) The participants did SLR exercises with tracing yellow and green patterns by moving the leg while maintaining the knee extension position; since the green pattern was shorter than the yellow one, the blue and yellow patterns were traced 30 times with a 5-minute rest between stretches.
3.5. Outcomes Measures
The outcome measurements, including demographic data, radiographic evaluation, and pain before the intervention, were evaluated for all participants. The primary outcome measures were the ROM of the knee joint in the sagittal plane and the assessment of pain intensity. The secondary outcome measure was participants’ satisfaction with the treatment.
3.5.1. Primary Outcome Measures
3.5.1.1. Range of Motion
This project evaluated the ROM of the knee joint in the sagittal plane (flexion and extension) based on Norkin measurements by a standard plastic goniometer in the supine position (32), and the participants’ ROM was reassessed after each training session. For the measurement of ROM, the participants were placed in a supine position with knees flexed as much as possible, and then its angle was measured three times with a goniometer. Gogia et al. evaluated the reliability and validity of plastic goniometers in ROM knee (33). The participants were asked to straighten their knee in the same position with the maximum power without the help of hands to measure the knee extension. The examiner then measured the knee extension angle and tested it three times to reduce the measurement error.
3.5.1.2. Pain
In the present study, the VAS was used to measure pain with a scale ranging from 0 to 10 for pain severity (ie, 0 - 10 as a continuum between no pain and worst pain, respectively) (34).
3.5.2. Secondary Outcome Measure
Satisfaction: At the end, the participants were asked to complete a questionnaire of satisfaction with four items, and answers could be according to the Likert Scale (35). Further, a 6-point Likert Scale was used (36), where each item scored from 0 (the tool is undesirable for the addressed aspect) to 5 (the tool is excellent for the addressed aspect). A score of 2.5 was selected as the competence threshold (24, 35).
3.6. Randomization and Blinding
The participants were randomly allocated to the multiple exercise group or the control group with block randomization. An independent researcher (who carried out no other assessments) performed this allocation. The information of this randomization remained concealed for the assessors up to finishing outcome assessments.
3.7. Sample Size Estimation and Statistical Analysis
The sample size was estimated based on the active knee flexion ROM as the outcome measure. According to a power of 90%, a two-sided significance of 0.05, and a dropout rate of 10%, a sample size of 16 patients was needed (37). All the participants completed the study successfully, and a 95% confidence interval was considered for ROM. The Kolmogorov-Smirnov statistical test was used to evaluate the agreement of variables with normal distribution. Furthermore, the Mann-Whitney U test, a non-parametric test, was utilized to compare the results of pain intensity, ROM, and satisfaction questionnaire data between the two groups using SPSS software (for Windows, version 22). The intragroup comparison was also performed using the Wilcoxon signed-rank test.
4. Results
The obtained results showed that knee joint flexion and extension ROM in both groups was significantly increased after therapeutic exercises (P < 0.05). Table 2 shows the intragroup and intergroup results of ROM and pain intensity assessments. The results of the intergroup comparison showed a significant difference between the two groups in terms of the flexion angle (P = 0.011); nevertheless, no significant difference was observed between the two groups in terms of the extension angle (P = 0.425). According to the VAS, the median pain intensity during rest and activities significantly reduced in both groups after the intervention (P < 0.05).
| Analysis | Flexion | Extension | Pain in Rest Condition | Pain in Activity Condition | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control Group | Intervention Group | Control Group | Intervention Group | Control Group | Intervention Group | Control Group | Intervention Group | |||||||||
| IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | |
| Before | 4.5 | 116.5 | 3 | 116 | 1.5 | 3.5 | 3 | 4.5 | 2 | 5 | 0 | 6 | 2.5 | 7.5 | 1 | 8.5 |
| After | 3 | 118 | 2.5 | 120 | 2 | 3 | 2 | 3.5 | 1 | 3 | 1.5 | 4.5 | 1 | 4.5 | 1 | 5.5 |
| P-value (intragroup) | 0.033 | 0.018 | 0.033 | 0.059 | 0.027 | 0.011 | 0.016 | 0.010 | ||||||||
| P-value (intergroup) | 0.011 | 0.425 | 0.044 | 0.010 | ||||||||||||
Abbreviation: IQR, interquartile range.
Table 3 shows the average score for each item of the satisfaction questionnaire in each group and the results of comparing the scores between the two groups based on the Mann-Whitney U test. A score above the optimal threshold (2.5) was considered for each item. In this regard, a significant difference was observed between the two groups (P = 0.002).
| Groups | Items | Mean | Median | |||
|---|---|---|---|---|---|---|
| Item 1 | Item 2 | Item 3 | Item 4 | |||
| Control | 3.2 | 3.8 | 4.1 | 4 | 3.72 | 3.95 |
| Intervention | 4.6 | 4.5 | 4.2 | 4.6 | 4.47 | 4.55 |
| P-value | 0.002 | |||||
5. Discussion
Telerehabilitation attracts increased consideration from society (ie, the research community and commercial market) (38). The present study aimed to compare two traditional and trace tool methods of exercise therapy in pain and ROM improvement in subjects with knee OA. The obtained results revealed that knee joint ROM in the sagittal plane increased in both groups after the exercises, and there was a significant difference between the intervention and control groups regarding the ROM of knee flexion. No significant difference was observed between the two groups in terms of the extension angle that can be due to the limited ROM of the knee extension, indicating that both treatments led to improvements in joint ROM. Therefore, the changes in ROM were small without any differences between the two groups. On the other hand, the better results of the intervention group than the control group in increasing the ROM of flexion showed that participants’ adherence to the treatment method had a direct effect on the treatment results.
Based on the satisfaction questionnaire findings, all participants were assigned a score higher than the optimal threshold for every item. The highest score was related to item no. 1 (ie, the easy use of the treatment) in the intervention group (ie, the tool had a simple design for its users). Therefore, numerous users who cannot understand complex tools can easily perform their exercises with the studied tools. On the other hand, the results of the satisfaction questionnaire showed that item no. 4 (ie, willingness to use the tool in the continuation of the treatment process) received an average score of 4.6 (about 92% satisfaction). Consequently, the tool can result in increasing the number of participants in exercises.
The findings of the intergroup comparison showed a significant difference between the two groups, with a higher median score in the intervention group than the control group. Therefore, the laser treatment method was more successful than the conventional method. The participants were more inclined to continue the treatment process using the studied method than the conventional method.
The results showed that the progression of a patient with OA at a long time (3 - 6 months) with an exercise plan depends on different factors, including locally available facilities, time, money, comorbidities, age, and social support (39). Since exercises with tools designed in this study do not require any clinical travel and high costs, it had the better follow-up of patients with OA in doing therapeutic exercises and saving time with better availability.
In a review study conducted on the effectiveness of the telerehabilitation method (ie, virtual reality [VR]) in patients with knee OA, the effectiveness of VR-based rehabilitation was unclear; however, interventions based on VR were promising in managing pain and postural and proprioception training (40). In addition, VR-based rehabilitation is an expensive method, leading to financial problems for the users.
Some limitations are placed on the present study, such as the small number of participants and only evaluation of clinical outcomes, not laboratory outcomes, derived from limitations caused by COVID-19. The long-term effect of the studied tool on participants regarding the exercises resulted in confirming the tool’s effectiveness. Additionally, the effect of tracing movement patterns should be investigated during therapeutic exercises in other groups of patients with musculoskeletal disorders who require ongoing therapeutic exercises. Finally, the efficiency of the studied tool should also be evaluated on other relevant parameters, such as gait parameters.
5.1. Conclusions
The studied tool in tracking movement therapy patterns could result in increasing knee joint ROM significantly and decreasing pain in comparison to conventional exercises while performing therapeutic exercises in patients with knee OA. Patients were more inclined to use this method through the studied tool for doing exercises than conventional methods.