1. Introduction
Vascular anomalies are formed by the destruction of the endothelium and adjacent tissues and generally can be divided into vascular tumors and vascular malformations (1). Varicose (vascular varices) are vascular malformations caused by vasodilatation. The most common site of vascular varices is the legs, which often occur in elderly patients. However, it can be present in the oral cavity.
The most common places in the oral cavity are the ventral surface of the tongue and the buccal and retro-commissural mucosae. If this type of vascular malformation develops on the lip, it is called the venous lakes (VLs) (2-4).
VLs of lips and oral cavity are usually dark-blue to violet soft papules or nodules with a maximum diameter of 1 cm, which blanches with pressure. Except for occasional bleeding and aesthetic problems, no other complication has been attributed to these lesions (5, 6). Biologically, VLs are known as vascular lesions; however, clinically, they are similar to malignant lesions such as melanoma, sarcoma, and pigmented basal cell carcinoma (7). There are two hypotheses for VLs formation, the first being solar damage and the second being vascular thrombosis.
These lesions are usually asymptomatic. If they are traumatized (biting, etc.), bleeding can occur, and they may become painful and sensitive (7).
Histologically, a dilated vein includes a thin layer of endothelial cells supported by fibrous tissue in the upper layer (8, 9). The prognosis of VLs is excellent, and patients can be confident that there will be no risk of malignancy. But it does not diminish spontaneously (7). Treatment modalities include surgical excision, infrared coagulation, cryotherapy, sclerotherapy, intense pulsed light, corticosteroids, interferons, radiation therapy, electrocauterization, and laser (10-13). Although managing vascular malformations depends on various factors, such as size, location, esthetic, stages of growth, and behavior, most are self-limiting (12). Surgical treatment is conventional but controversial as there is a high risk of bleeding. In contrast, the laser, a novel and low-risk method can ablate superficial vascular lesions (13). In this study, the effectiveness of coagulation properties of 940-diode laser is investigated considering its advantages, such as the low risk of bleeding, patients’ comfort, and fast and scar-less wound healing properties.
2. Case Presentation
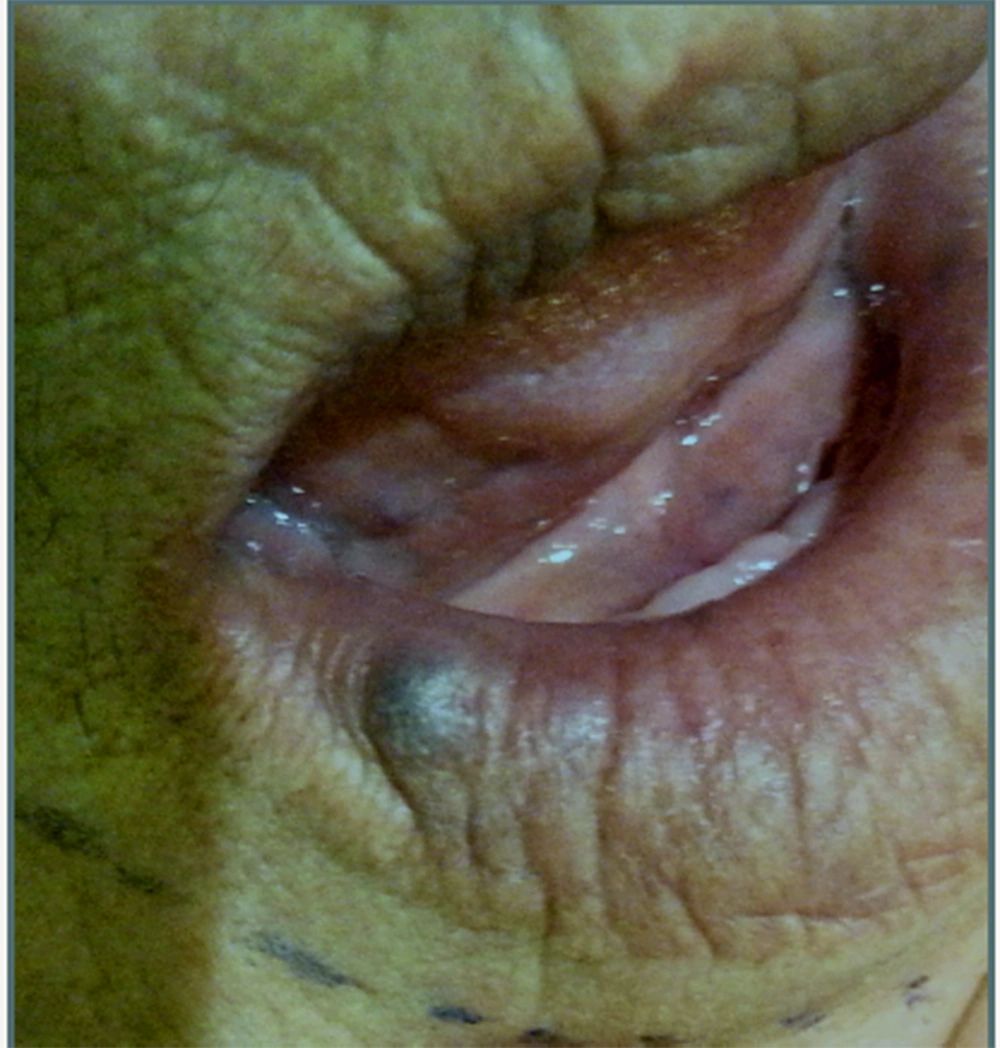
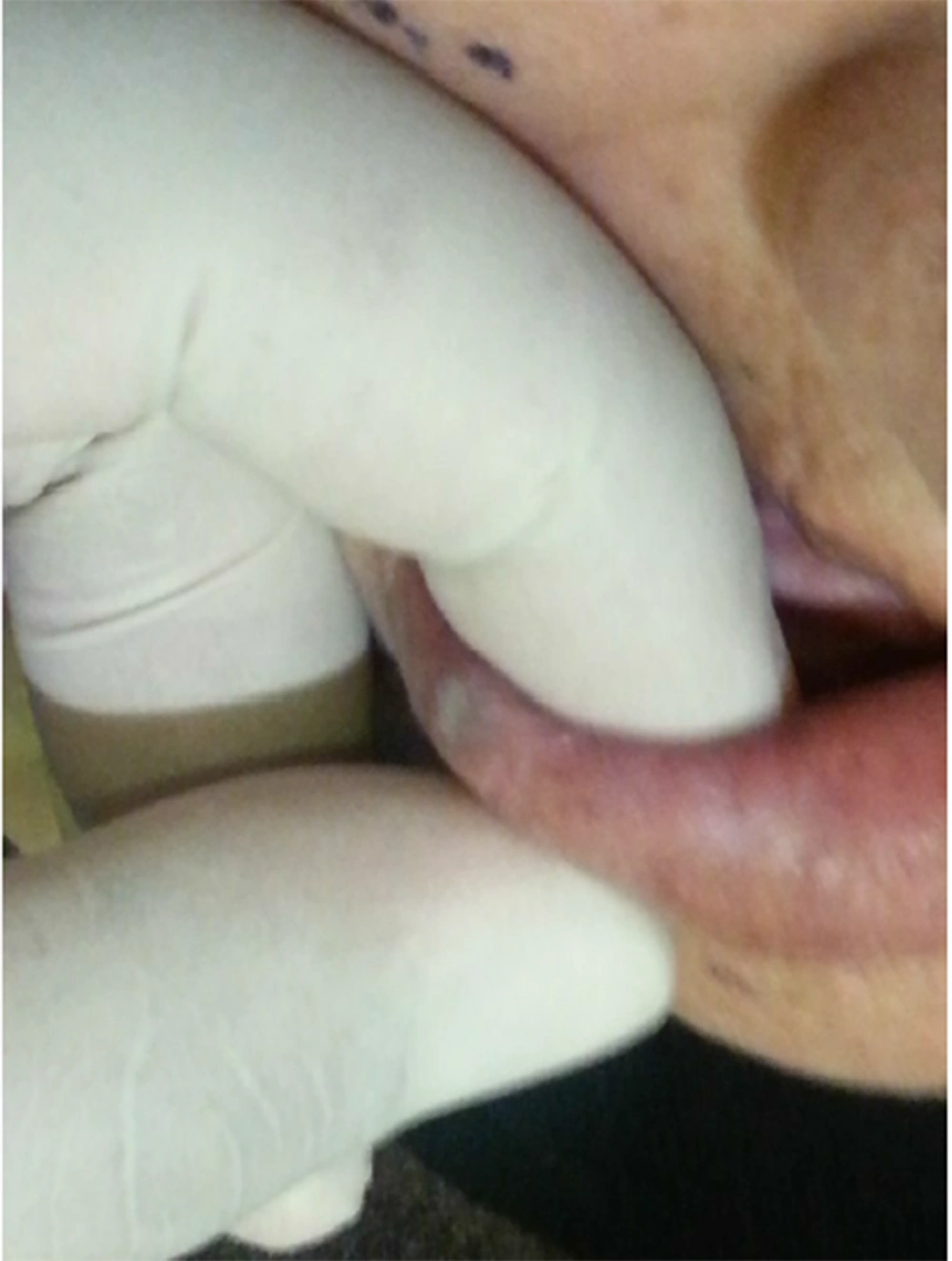
The patient was a 70-year-old woman admitted to the dental clinic of Semnan University of Medical Sciences, Iran, for a dental examination. Extra- and intra- oral examinations were performed for the referred patient. Lip examination revealed a violet sessile nodule with a smooth surface, with a 1cm dimension on the left side of the lower lip’s vermilion. The vascular nature of this lesion was proven through diascopy. Considering the high prevalence of venous varices on the lips, it was considered the first diagnosis (Figure 1). This lesion had been presented for several years without treatment, as it had remained asymptomatic. However, it was noticeable on the patient’s face and caused aesthetic problems. The lesion sometimes became traumatized by her teeth and had transient episodes of enlargement. After obtaining informed consent, the lesion was treated in one session without local anesthesia by non-contact and uninitiated 940 nm diode laser (Biolase, 2 W), with 400 nm fiber and 8 mm distance from the lesion (Figure 2). The time required to treat the lesion was 90 seconds. Immediately after treatment, coagulation occurred, then the lesion size decreased. Moreover, significant discoloration to light gray was noted (Figure 3). The lesion entirely disappeared in the following three-week follow-up (Figure 4).
3. Discussion
This study was designed for treatment of a VL lesion with a 940 nm diode laser using its coagulation properties. Regarding this, it is a noteworthy point that vascular lesions are divided into several groups; VLs types of these vascular lesions appear as dark blue to violet papules or nodules, most commonly in the face on lips (in the craniofacial region) of older men (5, 14). The progression of this lesion is exacerbated by exposure to sunlight (5). Most patients seek treatment due to aesthetic and bleeding problems (15).
Accordingly, there are several treatments depending on the type, location, behavior, size, esthetic, stage of growth, and depth of vascular lesions (8, 12). Several studies have been conducted to treat VLs on lips. In these studies, various methods, including surgical excision with a blade, infrared coagulation, electrocauterization, cryotherapy, sclerotherapy, laser therapy, intensive pulsed light, corticosteroids, interferons, and laser therapy, were used. The choice depends on the risks and benefits associated with each method (12, 13, 16).
In some cases, due to the size and the location of the vascular lesions, practitioners chose surgical excision. They reported that after the surgery, there were no clinical or radiographical signs of recurrence (17, 18).
On the other hand, others believe excision is a challenging treatment plan for these lesions because of the high chance of recurrences (13). Notwithstanding this, other methods also have disadvantages. For example, corticosteroids have several systemic side effects; therefore, they should only be exploited in particular cases. Although radiotherapy can ablate the lesion, it causes tissue atrophy, particularly on the skin. Cryotherapy and laser can be used for superficial lesions (13).
Soni et al. attempted to treat intraoral hemangiomas through intra-lesion injection of sclerosing agents. They repeated the injection after three weeks and six months and reported that the lesion had almost disappeared (19).
For small lesions, sclerotherapy may be sufficient by intralesional injection of sclerosing agents, such as 95% ethanol, which stimulates fibrosis.
In larger lesions, after sclerotherapy, excision surgery is performed, but it is not pleasant to patients because of pain, swelling, and anesthetic injection (20). Due to the problems mentioned for other methods, such as pain, discomfort, delayed wound healing, and bleeding, and considering the advantages of diode laser, such as fast recovery and lack of pain and bleeding during and after the treatment, we choose the 940 nm diode laser in this case, and observed no adverse effects (1).
In 2016, Mlacker et al. reported that the application of surgical procedures is associated with pain, bleeding and scarring, and delayed recovery (21). The high-intensity diode laser for treatment of VLs, because of its depth of penetration, is more effective than other types of laser, which was also reported by Voynov et al. in 2016 (7). It is poorly absorbed by water and penetrates to a depth of 4 or 5 mm in the tissue (21). Azevedo in 2013 demonstrated that high-intensity diode laser can prevent tissue changes or discoloration, which is usually caused by CO2 lasers (2). It should be mentioned that Migliari et al. reported that using ND-YAG laser for treating VLs is not as effective as the diode laser. They treated 60 patients and observed that healing was completed after 2 to 4 weeks (6).
Diode laser is less invasive than surgery and minimizes bleeding, inflammation, and scarring. The advantages of the diode laser are the lower cost and ease of use compared with other types of lasers. The diode laser can be used to treat soft tissue lesions, such as fibroma, epulis fissuratum, and soft tissue vascular lesions (22, 23). It should be considered, however, that the most commonly used method in all previous studies was a combination of surgery and sclerotherapy, which is a practical method, and few studies have used laser. Surgical treatment is controversial, though, because of the high risk of bleeding and scar formation. In contrast, the laser can be used for superficial vascular lesions as a novel and low-risk method; patient satisfaction is higher than other methods due to the lack of bleeding and pain (13). Because of the aesthetic concerns of the patient and the advantages of diode laser for treatment of these lesions, in this study, a case of VLs was treated using the coagulation property of 940-diode laser, and satisfactory outcomes were observed in the shortest time.
3.1. Conclusions
Using the coagulation properties of the laser to eliminate venous lakes, in comparison with other methods, is advantageous because of the lack of bleeding and pain for the patient, and the shorter healing time.