1. Background
Cerebral palsy is considered a non-progressive neurodevelopmental disorder that begins in early life (1). Its motor dysfunction is often associated with sensory impairment, perception, cognition, communication, epilepsy, behavior, and secondary musculoskeletal conditions (1-3). The prevalence of cerebral palsy is 1.2 per 1000 live births around the world (4). One of the most common forms of cerebral palsy is hemiplegic, with the prevalence of 1 per 1000 births (5), which is the most common cause of severe motor impairment in childhood (6). Hemiplegia resulting from cerebral palsy is known as a sensorimotor problem affecting postural control (7), muscle coordination, and movement (6). One of the most debilitating symptoms of hemiplegia, which may occur in more than 80% of children suffering from cerebral palsy, is dysfunction of the upper limbs, especially the arms and hands (8, 9). They usually suffer from fine motor skill deficits, weak grip strength, and decreased hand dexterity (10, 11).
Upper limb function in cerebral palsy plays a crucial role in independence, quality of life (12), children’s participation in their activities of daily living (ADLs) (13, 14), social interactions, and exchanging information with others through non-verbal communication; in a way that proper function and control can help express the concepts and convey emotions (15). Hemiplegic cerebral palsy causes problems with contraction, sensation, and muscular strength in the upper limbs, which its effective use of muscles for reaching, grasping, releasing, and manipulating objects is often compromised (16, 17). It also creates problems with self-care, training, and fitness activities, thereby affecting self-confidence, self-esteem, self-concept, and quality of life (18-21). Self-concept involves awareness of one’s own characteristics, such as understanding one’s identity and evaluating one’s characteristics in relation to others (such as general self-confidence or a sense of self-worth and usefulness) (22). In other words, it affects children’s self-image and self-assessment (23). Any difficulty with self-concept in hemiplegic cerebral palsy can affect their health, performance, and quality of life (19, 20, 22-25). On the other hand, there are several treatments to improve the hand function of these children, and finding the most appropriate treatment requires considering 3 criteria: (1) technical results; (2) how treatment affects homework and its role in the child’s life; and (3) the degree of patient self-satisfaction. Despite the therapists’ great attention to the first 2 criteria for determining the appropriate treatment method, the third criterion has not received much attention from therapists (26).
Some systematic reviews have been conducted on the self-evaluation and self-concept in cerebral palsy. For example, Roostaei et al. evaluated the relationship between self-evaluation and functional motor status in cerebral palsy children, showing that despite a significant relationship between those outcomes in people with cerebral palsy, no relationship was found between functional motor status and self-concept in these children (27). In addition, other reviews have stated that the self-concept of these children was significantly decreased compared to healthy children (24, 28). Another study indicated that the self-concept in cerebral palsy was not related to their motor functions (29), or there was no difference in self-confidence between healthy children and those with cerebral palsy (30, 31). Based on the difference in the results of various studies in terms of self-assessment and motor function for individuals with cerebral palsy, more studies are needed due to the importance of these variables in the process of evaluation and treatment of these children. The use of structured evaluations based on a client-centered framework has been proposed as a solution for further participation in treatment (32). In this regard, the child occupational self-assessment (COSA) Scale is an appropriate tool to assess clients’ perceptions, give them a role in identifying goals and treatment strategies, and also measure changes in the results of clients’ self-reports (33). Due to cultural diversity in the levels of self-concept, it is not possible to use the findings of other societies for Iranian culture (34).
2. Objectives
In the present study, we examined the correlation between fine motor skills and occupational self-assessment in 8 to 13-year-old children with hemiplegic cerebral palsy.
3. Methods
3.1. Participants
In this cross-sectional study, an available statistical sample was selected from 8 to 13-year-old children suffering from hemiplegic cerebral palsy referred to occupational therapy centers and schools for physically impaired students in Tehran. Due to the lack of a similar study and the uncertainty of the correlation coefficient, the sample size was determined after a pilot study on 12 children. After determining the correlation coefficient of the pilot study, the following formula was used to calculate the sample size. This calculation showed that 50 participants were required to achieve 80% power for the present study.
β = 0.1; α = 0.05; Zβ = 1.28; Zα = 1.96; r = 0.218
Inclusion criteria were subjects diagnosed with right or left hemiplegic cerebral palsy in the age range of 8 to 13 years and with hand dysfunction diagnosed by a pediatric neurologist, cognitive level estimation using the SPARCLE cognitive test to determine the ability to perform tests by the child (35), and having 1 of 3 levels (I - III) of the hand motor according to the manual ability classification system (MACS) (36). Exclusion criteria were unwillingness to participate in the study, a history of surgery and Botox injections in an individual’s hand during the last 6 months according to family reports and medical records, participation in similar research during the last 6 months to prevent the learning phenomenon, obvious deformity in the upper extremities, defects in the range of motion of upper limb joints that forced children to require special aids in carrying out their ADLs, and levels 4 and 5 of the MACS classification. This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1400.218).
3.2. Procedure
First, we referred to the medical centers providing rehabilitation services for individuals with cerebral palsy; these medical centers were approved by the Organization of the Medical System of the Islamic Republic of Iran. For sampling based on the inclusion and exclusion criteria, children’s parents with hemiplegic cerebral palsy were contacted. Then, with the cooperation of the occupational therapists of these centers, statistical samples were selected. Children’s parents qualified to participate in the project were informed of the research objectives and tests performed on their children, and then their written consent was obtained. A questionnaire completed by the evaluator was used to collect the required demographic information such as age, sex, affected side, and MACS levels of hand skills.
First, the Bruininks-Oseretsky Test of Motor Proficiency (BOTMP) was performed for participants in the “fine motor skills” part of the study by an occupational therapist who had 5 years of clinical experience and was unaware of the study results. The examiner then provided a suitable environment for children to perform the COSA test. The examiner was also available to the children to answer their questions at all stages. If the child became tired, nervous, frightened, upset, or distracted, the test would have been interrupted or stopped to be completed at another time. After administering the COSA questionnaire, the results were interpreted by reviewing the answers with the child and discussing their thoughts on each point.
3.3. Data Collection Tools
The following tools were used to gather data. The demographic questionnaire included age, sex, affected side, and MACS levels of hand skills.
3.3.1. COSA Questionnaire
This questionnaire is a client-directed assessment tool to record children’s and adolescents’ perceptions concerning their occupational competence and the importance of ADLs (33). This self-rating design allows clients to record their understanding of occupational competence and values using simple visual and linguistic cues. Sattari et al. indicated that the Persian version of COSA (21-item) had a good construct validity in terms of attention-deficit hyperactivity disorder (ADHD) in Iran (37). In this questionnaire, each item is scored with 2 scales for competence and values in a 4-point range. The scoring range on the competence scale includes 1 (very difficult for me to do), 2 (it is a little difficult for me to do), 3 (it is not difficult for me to do), and 4 (I do it very well). On the value scale, it includes 1 (It is not very important to me), 2 (it is important to me), 3 (it is very important to me), and 4 (it is most important to me). The average test duration is between 20 and 45 minutes (38).
3.3.2. BOTMP
This test is a set of tests that assesses the motor skills of children aged 4.5 to 14.5 years. The reliability and validity of this test in Iran have been considered on middle school students with a coefficient of 0.78 (39). The complete set of this test consists of 8 subtests (consisting of 46 separate sections), which assess motor skills or gross and fine motor disorders (40). In this study, the fine motor skills section of BOTMP was used, which has 17 items: 1 item evaluates the response speed, 8 items evaluate the control of visual-motor skills, and 8 items evaluate the upper limb speed (hand) and dexterity. For this study, the relationship between these 3 categories of items with occupational self-assessment indices was evaluated in hemiplegic patients.
3.4. Data Analysis
Mean, SD, minimum, and maximum were used to describe the data. Due to the ranking of the data, the Spearman correlation statistical index was utilized to determine the relationship between the variables. The significance level for all analyses was 0.05. Data analysis was performed using SPSS version 22 (SPSS Inc, Chicago, Ill, USA).
4. Results
In this study, 50 children aged 10 ± 1.5 years with hemiplegic cerebral palsy were evaluated based on their demographic characteristics (Table 1). According to the BOTMP questionnaire, the mean and SD of scores related to fine motor skills and its subscales (including motor response, visual-motor control, and the upper limb speed and dexterity of individuals with hemiplegic cerebral palsy) are presented in Table 2.
| Variables | No. (%) |
|---|---|
| Gender | |
| Female | 21 (42) |
| Male | 29 (58) |
| Age (y) | |
| 8 - 9 | 15 (30) |
| 9 - 10 | 4 (8) |
| 10 - 11 | 14 (28) |
| 11 - 12 | 10 (20) |
| 12 - 13 | 7 (14) |
| Affected side | |
| Right | 31 (62) |
| Left | 19 (38) |
| MACS Levels of hand skills classification | |
| Level I | 24 (48) |
| Level II | 14 (28) |
| Level III | 12 (24) |
| Questionnaires and Variables | Minimum | Maximum | Mean ± SD |
|---|---|---|---|
| Scales of Child Occupational Self-assessment Questionnaire | |||
| Competence | 51 | 73 | 60.98 ± 5.69 |
| Values | 40 | 71 | 54.70 ± 8.83 |
| Self-assessment (total) | 91 | 141 | 115.68 ± 14.04 |
| Bruininks-Oseretsky Test of Motor Proficiency | |||
| Response speed | 0 | 8 | 4.04 ± 2.44 |
| Visual-motor control | 24 | 45 | 70.33 ± 6.19 |
| Upper limb speed and dexterity | 20 | 48 | 32.70 ± 7.07 |
| Fine motor skills (total) | 24 | 53 | 37.74 ± 8.44 |
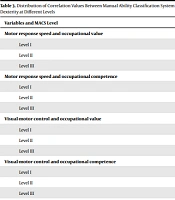
Table 3 demonstrates a significant correlation between subscales of fine motor skills (visual-motor control, motor response speed, upper limb speed, and dexterity) with the score of occupational value and competence at different levels (P < 0.05). The highest significant correlation (80%) was obtained between the upper limb speed and dexterity with occupational competence at MACS level I (P < 0.001), and the lowest value (23.7%) was between visual-motor control and occupational competence at MACS level III (P = 0.045). Also, there was a higher correlation between the upper limb speed and dexterity and occupational competence (correlation coefficient: 80%, P < 0.001) compared to the occupational value (correlation coefficient: 74%, P < 0.001) at MACS level I. Motor response speed (level I correlation coefficient: 71%, P < 0.001), upper limb speed and dexterity (level I correlation coefficient: 80%, P < 0.001) had a higher correlation rate in occupational adequacy compared to the occupational value at MACS level I, but the visual-motor control had a higher correlation at different levels of the occupational value (level I: 66%, P < 0.001; level II: 58%, P = 0.076; and level III: 36%, P = 0.024) than the occupational competence.
| Variables and MACS Level | Correlation Coefficient | P Value |
|---|---|---|
| Motor response speed and occupational value | ||
| Level I | 0.68 | 0.000 |
| Level II | 0.56 | 0.003 |
| Level III | 0.39 | 0.035 |
| Motor response speed and occupational competence | ||
| Level I | 0.71 | 0.000 |
| Level II | 0.53 | 0.050 |
| Level III | 0.42 | 0.025 |
| Visual-motor control and occupational value | ||
| Level I | 0.66 | 0.001 |
| Level II | 0.58 | 0.076 |
| Level III | 0.36 | 0.024 |
| Visual-motor control and occupational competence | ||
| Level I | 0.53 | 0.004 |
| Level II | 0.45 | 0.041 |
| Level III | 0.23 | 0.045 |
| The upper limb speed and dexterity and occupational value | ||
| Level I | 0.74 | 0.000 |
| Level II | 0.71 | 0.032 |
| Level III | 0.56 | 0.011 |
| The upper limb speed and dexterity and occupational competence | ||
| Level I | 0.80 | 0.000 |
| Level II | 0.77 | 0.007 |
| Level III | 0.49 | 0.025 |
5. Discussion
The current study investigated the correlation between fine motor skills and occupational self-assessment in children with hemiplegic cerebral palsy aged 8 - 13. Based on the findings, the factors of upper limb function at levels I to III of the MACS classification system indicated a significant relationship between fine motor skills (including visual-motor control, motor response speed, upper limb speed, and dexterity) with occupational self-assessment (occupational value and occupational competence). This means that the higher the level of MACS and the better the fine motor skills of children with hemiplegic cerebral palsy, the better they evaluate themselves (in both occupational value and competence).
To compare and interpret the research findings, Ziebell et al. indicated that hand functions (e.g., fine movement and dexterity) have a significant positive correlation with fine motor competence among spastic diplegia children. Thus, these children with a lower level of physical skills have a lower self-competence. These findings agreed with the findings of our study with the difference that our participations were children with hemiplegic cerebral palsy (41). Moreover, other studies have also investigated the relationship between a gross motor function with different self-related areas in cerebral palsy people who had different levels of functional status. In all of these studies, it was stated that cerebral palsy individuals with better functional status had higher self-esteem (21, 42), self-worth (43), or self-perception (41).
A comparison of the correlation of fine motor skills with occupational value and competence showed that fine motor skills were more related to the subscale of occupational competence. Since the value dimension in the occupational model depends on various factors, environmental factors (such as the type of family attitude toward the child) may affect this dimension of self-assessment. Among the factors related to fine motor skills, upper limb speed and dexterity demonstrated the strongest correlation with occupational self-assessment and components of occupational competence and value. Also, comparing these 2 components and their correlation with the upper limb speed and dexterity, the findings indicated that occupational adequacy had a higher correlation with the upper limb speed and dexterity. These 2 variables and their components in ADLs and the school and community environment are very important for these children. Therefore, it may be supposed that upper limb speed and dexterity have a strong correlation with occupational value and competence. On the other hand, Gannotti et al. stated that mobility for adults with cerebral palsy in ADLs scored by the functional independence measure (FIM) is not related to their self-concept (44); this discrepancy is due to the different samples of our study.
Comparing the 2 components of self-assessment (occupational value and competence) in cerebral palsy children, the findings revealed that the average occupational competence scores were higher than the occupational value scores. This means that competence and ability to perform their ADLs and school homework were at an acceptable level, but their understanding of the value of these activities was low. For example, although the child has the necessary competence and efficiency in dressing, he/she has little understanding of the value and sense of independence in doing so.
A cross-sectional study design, small number of samples, and available sampling methodology are some limitations of the present study, making the results non-generalizable to all children of cerebral palsy. Therefore, for a deeper understanding of the effect of self-assessment on these children, it is suggested that future studies with larger sample sizes, random sampling methodology, level of children’s education, and statistical regression tests be performed to determine the role of these factors.
5.1. Conclusions
Findings showed that to improve occupational self-assessment of cerebral palsy children, special attention should be paid to progress the function of the upper extremity through occupational therapy interventions. Facilitating the upper limb function of these children can lead to improved quality of life, strong sense of self-efficacy, and greater independence.