1. Background
Burns are among the devastating threats to the global health (1). After traffic accidents, falls, and cross-border conflicts, burns claim the fourth rank among the causes of serious injuries worldwide (2). According to a report from the World Health Organization (WHO) in 2018, 180,000 deaths occur annually due to burns, mainly happening in third-world and underdeveloped countries (3). In Iran, burns are among the 20 disorders with the highest mortality and morbidity rates, ranking 11th among men and 10th among women (4). In a comprehensive study conducted in Iran, the number of deaths due to burns across the country was reported to be 80,625 cases over 25 years (5). Studies in some parts of the country have indicated that burns due to flame and hot liquids are more common in young people, women, and less-educated individuals, showing a death rate varying from 27.9 to 34.4% (6).
Hands are necessary for performing daily activities such as taking a bath & showering, dressing, self-feeding, personal hygiene, and toileting (7) but, at the same time, are among the most vulnerable parts of the human body (8). The American Burn Association has included hand burns in the "major injury" category (9). Actually, hand burns account for 6% of all hand injuries. Upon hands’ loss of functioning, people lose 54% of their total performance (8). In addition to creating functional disabilities, hand burns limit patients’ social and professional lives and, therefore, negatively influence their quality of life (10).
Regarding burn-associated functional limitations and social and psychological consequences, burn patients often feel incapable of performing everyday life activities, which makes substantial, negative contribution to their outcome (11). Anxiety, anger, and depression, as common psychological disturbances, can occur at any stage following a burn injury (12). Therefore, it is important to develop a comprehensive therapeutic plan, such as rehabilitation programs, for patients with hand burns (8). Considering advances in treating burns, as well as the extended survival of patients, rehabilitation programs have attained considerable attention for improving patients’ living conditions (13).
Rehabilitation is among the most important strategies in treating patients with hand burns. In addition, passive movements and focused therapy can help treat these patients (9). To this end, the involvement of an interdisciplinary care team, including surgeons, physiotherapists, occupational therapists, nurses, and psychologists, as well as the participation of each team member from the day of admission are required (14). The main focus of rehabilitation is to restore the performance and improve the appearance of burned areas (15). Hand performance is defined as the "ability to use hands in Activities of Daily Living (ADL)" (16). One of the most important goals of burn rehabilitation programs is to restore hand functioning; however, achieving the desired functional levels requires designing, implementing purposeful plans accurately, and monitoring their effectiveness (17). General daily life activities include all those tasks or activities performed by an individual on daily basis in order to maintain personal independence (18).
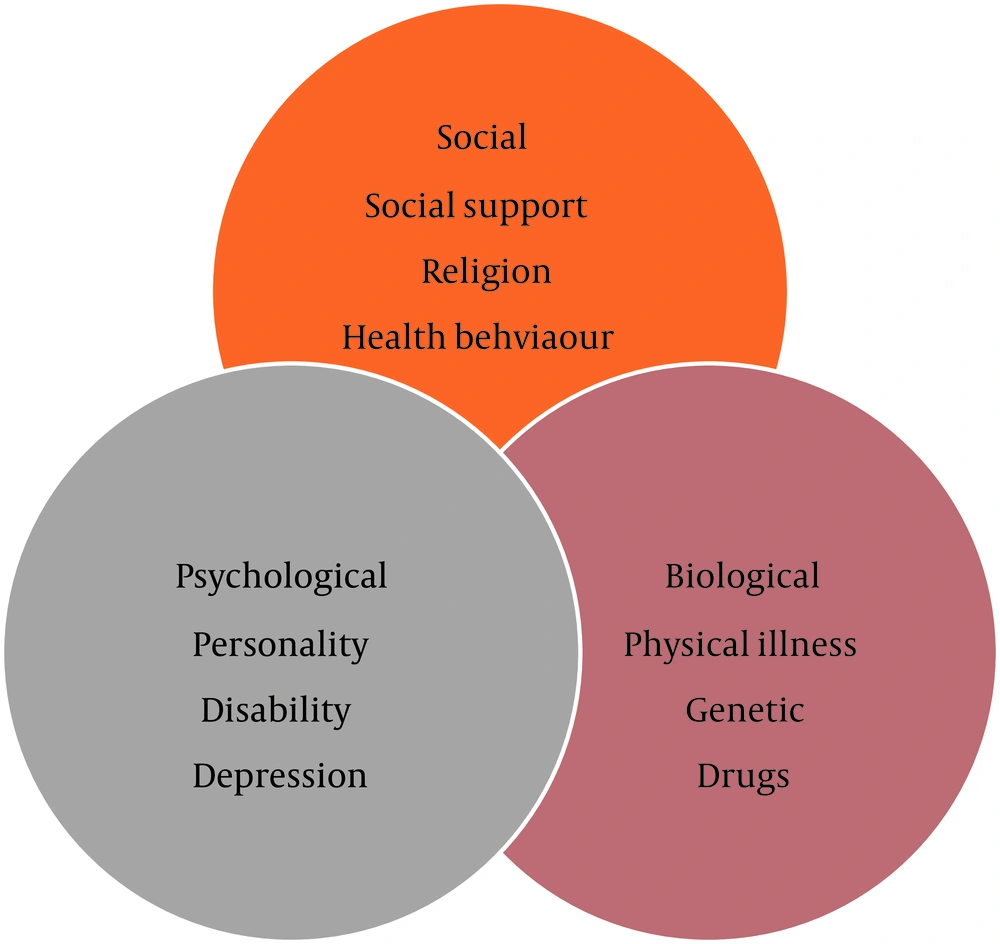
Rehabilitation is an active program aimed at preparing the patient to return to the desired condition in all circumstances (19). During rehabilitation programs, nurses play key roles in establishing a relationship between the patient and his/her family, and other members of the health team. Nurses are also involved in the careful examination of the patient's condition to reduce complications (3, 20). To this end, adopting a rehabilitation nursing model based on biological, psychological, and social-medical features, as well as capable of incorporating biological, psychological, and social parameters into health perception, disease management, and health service provision is necessary (Figure 1) (21, 22). The implementation of such models encourages the patient to effectively take part in self-care and boosts the patient’s responsibilities in controlling the disease’s complications. In addition, these models help people maintain their independence and improve their performance (6).
Regarding the extensive effects of burns on the victim’s physical functioning, studies have mainly focused on wound healing approaches, surgical treatments, anxiety management, self-management training, and mental self-image improvement. A study has shown that patient education could be an effective factor in boosting patients’ awareness and alleviating their anxiety (23). Nevertheless, many of these methods are not systematic (24). A rehabilitation model has been found to significantly enhance the physical, mental, and social functioning of patients with hand burns (22). Regarding psychosocial performance, patients with hand burn have been reported to be vulnerable to depression, anxiety, and a variety of other psychological problems, affecting their daily life activities (25).
In a study by Rouzfarakh et al., the effects of rehabilitation training through social media on the quality of life of burn patients were investigated. Their study results showed that the mean scores of patients in both intervention and control groups were improved in terms of simple abilities, hand functioning, emotional performance, body image, interpersonal relationships, sensitivity to heat, adherence to treatment regimens, and occupational performance (3). Li et al. examined the effects of a rehabilitation nursing program on hand burn patients' overall health and showed that patients in the intervention group acquired higher scores than patients in the control group in terms of general health, as well as physical, mental, and social performance (22).
2. Objectives
The present study’s aimed to evaluate the effect of a rehabilitation nursing program on hand burn patients’ daily functioning.
3. Methods
3.1. Study Design
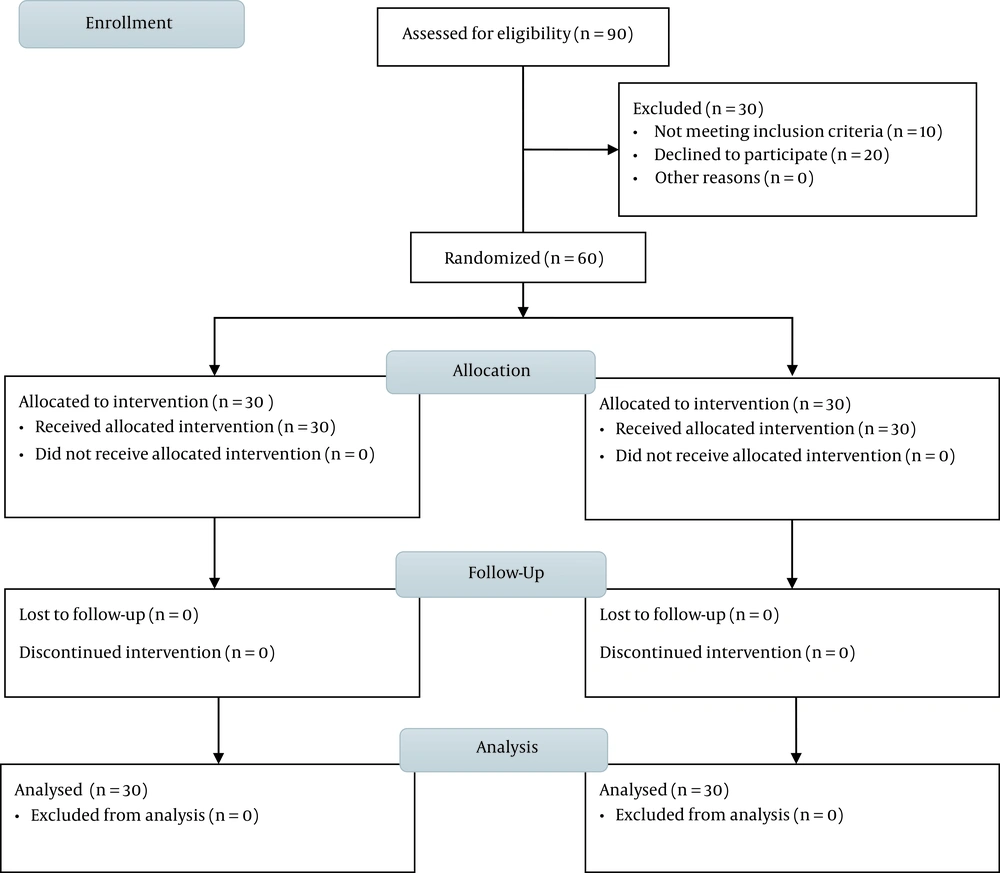
The present randomized, controlled trial was conducted to examine 60 hand burn patients referred to the Shahid Motahari Educational and Medical Center of Tehran from November 4, 2020, to April 19, 2021 (Figure 2). The sample size was determined by considering a 95% confidence interval, the study power of 80%, and a moderate Cohen effect on the subjects’ daily functioning through comparing the control vs. intervention groups (E.S = 0.5). Taking into account a 10% drop-out rate, these values were inserted into the relevant formula, and a sample size of n = 30 per group was achieved.
3.2. Inclusion Criteria
Burning of the dominant hand (with or without the involvement of the opposite hand), deep partial- or full-thickness burns, age of over 18, lack of a history of mental disorders, having reading and writing literacy, and willingness to participate in the study were regarded as inclusion criteria.
3.3. Exclusion Criteria
Patients with serious damage to the muscles of the upper limbs, tendons, skeleton, and nerves, those with severe cardiac disorders, patients who fainted before burning, individuals with pulmonary and cerebral problems, and, finally, those reluctant to continue participation in the study were excluded.
3.4. Ethical Considerations
Due to the nature of the intervention, there was no blinding in this study. The study’s protocol was approved by the Ethics Committee of Iran University of Medical Sciences (IR.IUMS.REC.1399.715) and registered at the Iranian Registry for Clinical Trials (IRCT20201207049634N1).
3.5. Study Procedure
After obtaining the necessary approvals, the researcher referred to the research environment (i.e., Shahid Motahari Educational and Medical Center) to recruit patients with hand burns based on the inclusion criteria. The patients were recruited through a continuous sampling process. After explaining the study’s objectives, the patients were requested to fill out and sign an informed consent form.
The participants were randomly assigned to the control and intervention groups adopting the block randomization method and using blocks with the size of four. Each patient was assigned with a unique code, and the block lists were assigned with a number of 1 to 6. Then a colleague, who was not involved in the research, was requested to randomly select a number between one and six for 30 rounds. By doing so, the order of the blocks was specified, and the complete list of assignments from 1 to 60 (for both the control and intervention groups; 30 per group) was characterized. Each time, the prepared assignment list was provided to a colleague who was not involved in the study to record patients’ names in the list. Thus, participants were randomly divided into the control and intervention groups, while the researcher and participants were unaware of group assignments. Finally, the assignment list was provided to the researcher. Participants in both groups were provided with a demographic questionnaire as well as the General Activities of Daily Living (GADL) questionnaire in order to gather pre-test data.
3.6. The GADL Questionnaire
The GADL questionnaire contains three dimensions (i.e., self-care, home-care, and daily-care) and 13 questions to determine whether or not the patient is able to do minor household chores, use the phone (make and receive calls), prepare her own meals, do the laundry, and iron clothes by himself/herself. Each question is answered on a 3-point Likert scale from dependent (score = 0), needing help/somehow dependent (score = 1), and independent (score = 2). The overall score ranges from 0 to 16, and each subject is placed under one of the dependent (scores between 0 and 7), needing help (scores between 8 and 11), and independent (scores between 12 and 16) groups based on the score obtained. Paula et al. assessed the validity and reliability of the instrument and reported a reliability coefficient of 0.80 (26). The validity of the tool was confirmed through the translation and back-translation methods and according to the viewpoints of five professors from the Nursing Faculty of Iran University of Medical Sciences. The instrument’s reliability was checked in a pilot study with 20 participants, and a Cronbach’s alpha coefficient of 0.76 was achieved.
3.7. Intervention
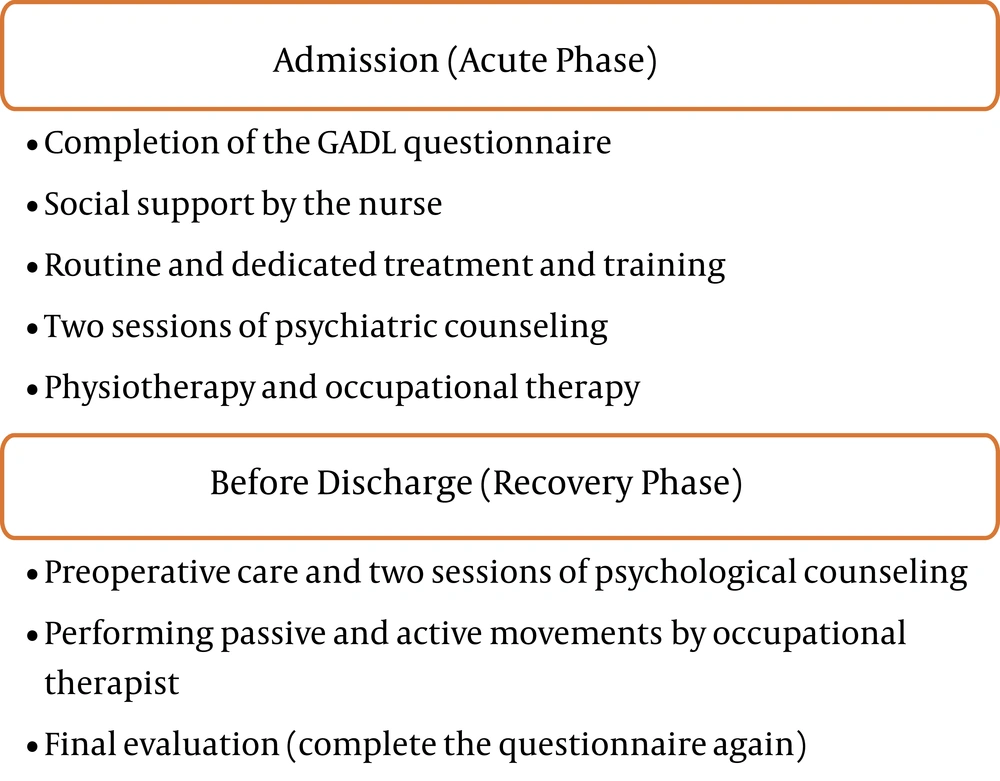
The participants in both the intervention and control groups completed the GADL questionnaire in two stages: at the time of admission and before discharge. All patients received routine therapeutic-rehabilitation programs at the care center. Patients in the control group only received routine nursing care. The rehabilitation nursing intervention lasted five weeks, and was delivered following two steps by a team consisting of a nurse, a physiotherapist, and a psychologist, who all were working at the same center (22).
(1) Admission (acute phase): This step included the pre-wound healing period and encompassed one to three days after admission. In this step, the participants completed the demographic and GADL questionnaires under the supervision of the researcher. During this phase, the nurse established the initial relationship with patients according to their physical and mental conditions. Also, social support was provided to the patients according to their age, level of education, and abilities to obtain information directly or through the family. Moreover, the patients and their families were provided with regular, targeted health training to boost their self-confidence, help them understand their role in the rehabilitation, and encourage patients to walk and communicate. In this regard, successful examples of rehabilitation were noted to create confidence and positive attitudes in patients towards therapeutic procedures and therapists, including the physiotherapist and psychotherapist, who were involved in providing social support to the patients.
At this phase, health education included providing information about the skin’s normal function, common types of burns, size and degree of burns, wound-healing duration, hand surgery procedures, signs of scar hyperplasia, common bodily disorders after burns, body functions after burns, and strategies to deal with common disabilities through rehabilitation exercises.
In this phase, two 30-50-minute psychological counseling sessions were also held. The specialist initially communicated with the patient by creating a positive atmosphere so that the patient could express his/her thoughts, feelings, and concerns over the disease. The counselor helped the patient become aware of and deal with the existing situation in order for reducing his/her suffering. The main objective during this phase was to address the patient’s stressful and psychological reactions following burns, such as the depressive mood caused by the feelings of uselessness, loneliness, and suicidal thoughts. Simultaneously, hand rehabilitation movements were delivered by the physiotherapist, and the range of motion was gradually increased (compatible with the patient’s tolerance and to a limited extent to avoid bleeding) to 10 - 15 minutes per session, twice daily.
(2) Before discharge (recovery phase): This phase was initiated from the beginning of wound recuperation after skin grafting and continued for four weeks. At this stage, the GADL questionnaire was completed again. Also, two more psychological counseling sessions were held, each lasting from 30 to 50 minutes. Therapeutic measures included guiding patients on how to tolerate the situation, helping them to react emotionally, encouraging them to express their thoughts and feelings, and allowing them to handle inappropriate emotional reactions. At this stage, the focus was on patients’ psychological problems such as anxiety, low self-esteem, abnormal mental self-image, confusion, and helplessness towards the future, as well as unbearable pain and undesirable body image.
Active and inactive hand rehabilitation exercises were also performed by the physiotherapist during this phase. In the first week, the physiotherapist used upper extremity joint (finger) repair tools to deliver hand rehabilitation movements (e.g., palm pressure and finger pressure) three times a day (15 to 30 minutes), by assigning priority to passive hand movements. Active and inactive hand movements were combined during the second week, initiated with projects involving practicing of daily activities, such as practicing Activities of Daily Living (ADL) (e.g., grabbing a rubber ball or a bed bar, dressing, washing, and eating). These activities were practiced at least two hours per day in the ward. Performing active and inactive movements was continued until the third week when training for strengthening finger muscle was initiated. During the fourth week, the ADL training and a combination of functional hand rehabilitation exercises were performed three times a day (30 minutes each time) in addition to performing active hand movements practiced in previous week. The GADL questionnaire was completed again 1-2 days before discharge (Figure 3).
3.8. Data Analysis
SPSS version 16 software was used to analyze the data. Descriptive statistics, such as frequency distribution tables and numerical indices were initially used to present the data, then, inferential statistics such as the independent and paired t-test, chi-square test, and analysis of covariance (ANCOVA) were performed. The statistical significance level in this study was set at P < 0.05.
4. Results
In this clinical trial, 15 men and 15 women were assigned to two intervention and control groups. The mean age was 36.53 ± 14.65 years in the control group, while it was 34.1 ± 13.23 years in the intervention group. Majority of the individuals in the two groups were married and had high-school diploma or college degrees. Half of the individuals in the two groups were employed, and the other half were unemployed, retired, or students. Most of them in the two groups had an average income. Majority of the individuals in the two groups had second-degree burns. Also, most of them had burns on their dominant hand. Overall, there were no significant differences between the two study groups regarding the participants’ demographic characteristics.
Prior to the implementation of the rehabilitation program, two groups were comparable in terms of Activities of Daily living (ADL) in the self-care dimension (Table 1, P = 0.366). The result of paired t-test showed that the mean pre- and post-intervention scores of this dimension were not significantly different in the control group, but this difference was statistically significant in the intervention group, suggesting a significant boost after the intervention (P < 0.001).
| Variables | Control | Intervention | P-Value b | F | η2 |
|---|---|---|---|---|---|
| Self-care | 17.814 | 0.245 | |||
| Before intervention | 6.3 ± 3.45 | 5.59 ± 2.49 | 0.366 | ||
| After intervention | 6.2 ± 3.16 | 8.57 ± 2.11 | < 0.001 | ||
| P-value c | 0.873 | 0.001 | |||
| Home care | 32.018 | 0.368 | |||
| Before intervention | 4.24 ± 2.67 | 2.7 ± 2.23 | 0.018 | ||
| After intervention | 4.33 ± 2.55 | 6.35 ± 1.85 | < 0.001 | ||
| P-value c | 0.815 | 0.001 | |||
| General care | 21.974 | 0.285 | |||
| Before intervention | 5 ± 2.95 | 5.26 ± 2.08 | 0.688 | ||
| After intervention | 5.033 ± 2.61 | 7.25 ± 1.32 | < 0.001 | ||
| P-value c | 0.938 | 0.001 | |||
| Overall daily functioning | 37.478 | 0.405 | |||
| Before intervention | 15.57 ± 8.39 | 13.56 ± 5.95 | 0.29 | ||
| After intervention | 15.56 ± 6.81 | 22.17 ± 4.97 | < 0.001 | ||
| P-value c | 0.996 | < 0.001 |
a Values are expressed as mean ± SD. η2 = partial eta-squared.
b Independent t-test
c Paired t-test results
There was a significant difference between two groups regarding the home care dimension at pre-test (P = 0.018). The results of ANCOVA also revealed a significant difference between two groups after the intervention (i.e., a higher mean score in the experimental group, indicating higher post-intervention performance in this group (P < 0.001)). According to the results from the paired t-test, the pre-test and post-test scores in this dimension were comparable in the control group, but a significant difference was detected in the experimental group (P < 0.001).
As for the general care dimension, baseline scores showed no significant difference when two groups were compared (P = 0.688). According to the results of ANCOVA, however, the participants in the intervention group – compared to those in the control group – obtained a significantly higher mean score in this dimension (i.e., a better performance) after the intervention (P < 0.001). The comparison of pre-test and post-test scores by the paired t-test revealed a significant increase of the mean score in the intervention group (P < 0.001), but no significant increase of the mean score was detected in the control group.
As for the ADL score, there was no significant difference between the study groups before the intervention (P = 0.29). According to the results of ANCOVA, the mean score in this dimension was significantly higher (suggesting better performance) in the experimental group compared to the control group after the intervention (P < 0.001). Comparing pre-test and post-test scores showed a significant increase in the intervention group (P < 0.001), but no increase was observed in the control group (P < 0.001).
5. Discussion
The present study was conducted to investigate the effectiveness of implementing a rehabilitation nursing program in upgrading the daily functioning of hand burn patients. The results showed that the post-intervention mean score of daily functioning was significantly improved in patients in experimental group in comparison with those in the control group. In other words, the implementation of the rehabilitation nursing program was found to improve the daily functioning of patients with hand burns regarding the three dimensions of self-care, home-care, and general performance.
Although many studies have evaluated the effects of various interventions on ADLs and upper limb performance in burn patients (27, 28), there are few studies addressing the role of rehabilitation nursing models in improving ADLs in burn patients (29). Aghajanzadeh et al. assessed the effectiveness of occupational-based rehabilitation therapy in improving the performance of patients with hand burns, which showed a significant difference in the mean DASH score before and after the intervention, suggesting that the intervention was effective in diminishing the challenges faced by patients during daily activities (1). In their study, Mohammadi et al. investigated the effects of implementing an empowerment program based on the Health Belief Model on the daily life activities of patients with the acute coronary syndrome. Their study results showed that implementing the empowerment program during hospitalization increased the mean score of daily activities in the patients participating in the rehabilitation program compared to their control counterparts (30). Najafi et al. conducted a study on burn patients and demonstrated that range-of-motion (ROM) exercises improved daily performance and physical, psychological, and social quality of lives in patients with second-degree burns (31). Likewise, the results of a study by Grisbrook et al. indicated that ROM exercises remarkably improved daily activities in burn patients (32).
Our study results revealed that the intervention group had a significantly higher mean score in the self-care dimension (i.e., a better performance) compared to the control group. In this line, Elsherbiny et al. explored the effects of a rehabilitation program on the quality of life of burn patients and reported that the early implementation of this intervention, as a part of the therapeutic plan, may have been beneficial for burn patients (33). Furthermore, Li et al. suggested that sports movements may have improved the physical health dimension of quality of life in burn patients (22).
At present, health policymakers are more inclined to adopt cost-effective healthcare strategies. Implementing low-cost interventions such as rehabilitation nursing programs can significantly reduce the rehospitalization rate and improve patients’ quality of life. Self-care, general care, and ADL are important indicators of the effectiveness of rehabilitation programs in boosting the functioning of hospitalized burn patients. The rehabilitation nursing intervention implemented in this study was found to significantly improve all three performance dimensions in patients with hand burns. However, this study was limited to investigating patients with hand burns; therefore, it was recommended that similar studies should be carried out to examine patients with burns of other body parts. It was also suggested that longer follow-up periods should be considered in future studies in order to draw more accurate conclusions.
5.1. Limitations
This study faced some limitations. First, it was not feasible to blind the participants due to the nature of the intervention. Second, the patients were not supervised during recess until the second phase of the study; during this time, therefore, they may have received information about hand burns from other sources (e.g., mass media) or have been influenced by misconceptions. Question and answer sessions were held at the end of each training class to identify these beliefs and correct them. Finally, no follow-up was performed in this study.
5.2. Conclusions
It was concluded that implementing the rehabilitation nursing model significantly improved physical and mental functioning, social relationships, and general health in patients with hand burns. Overall, our findings re-stressed the need for implementing and delivering a proficient, standard, and comprehensive educational rehabilitation program to improve the performance of burn patients.