1. Background
The ankle joint is most likely to be injured during exercise and among ankle disorders, lateral ligament injury is the most common to the extent that 85-90% of all sprains occur in the lateral ligament (1). Although the initial symptoms associated with lateral ankle sprains are generally resolved in a short time, many patients continue to report residual problems, such as pain, instability, and feelings of the ankle’s giving way (2). These residual symptoms have been reported during the last 6 to 18 months after the initial injury and have been observed in 55% to 72% of patients (3). Postural control requires the integration of visual, vestibular, and somatosensory input. Somatosensory input combines contributions from cutaneous, articular, and musculotendinous receptors. Afferent information gathered from these 3 sources is processed within the central nervous system and used to control motor commands. Deficient contributions from any of the afferent receptors can lead to diminished postural control. Postural-control deficits have been found repeatedly in patients with lateral ankle sprains (4). Consistent with this finding, Hertel and Corbett investigated postural control changes in single-leg standing in 17 patients with lateral ankle sprains using a force plate. They stated that postural stability is significantly weakened on the first day up to two weeks after injury (5). According to previous studies, balance is one of the main factors affecting ankle instability. According to Arastoo et al. people with instability in their ankle joint exhibit balance impairments when performing functional activities. This is because of the impaired function of sensory neurons in these individuals. Such impairment extends from the ankle joint to the central and peripheral nervous system. It also affects the function of motor neurons, leading to the perturbation of postural control while performing dynamic and functional activities (6). Testerman and Vander Griend also studied ankle instability in 10 athletes with unilateral ankle sprains using a Biodex device. They found that patients' injured leg was less stable than their healthy leg (7). In general, humans use different strategies to maintain and recover their balance when faced with sudden perturbations, depending on their severity. They include fixed-support strategies (e.g. ankle and hip strategies where the displacement of the center of gravity (COG) is controlled without a change in the base of support) and change-in-support strategies (displacement of the COG is controlled with a change in the base of support) (8). In this regard, Riemann stated in a review study that these patients, use hip strategy for postural control, rather than ankle strategy (9).
According to literature review, there are many studies on the balance of patients with ankle sprains, but there has been no study on the balance in the form of goal-oriented movements. In other words, participants in other studies were asked to just try to keep the center of mass at a base of support when standing on the Biodex device (7, 10, 11), while this balance is maintained in no targeted manner. Thus, previous studies have mostly evaluated afferent or efferent fibers alone, but the aim of the present study was to evaluate afferent and efferent fibers, and central processing, meaning that the plate of the Biodex device on which the patient stands is unstable and the patient must receive feedback from the sensory fibers, then the central processing must be done and be able to perform a task in a goal-oriented movement. In fact, with this task, all three items are evaluated together. Moreover the present study compares the injured and healthy foot specifically and more precisely in 6 directions.
2. Objectives
The present study aimed to compare goal-oriented movements and differentiate them in healthy and unhealthy legs of people with ankle sprains.
3. Methods
This is a cross-sectional study performed in the Neuromuscular Rehabilitation Research Center of Semnan University of Medical Sciences during the years 2018 - 2019 The present study was approved by the Ethics Committee of Semnan University of Medical Sciences with the code of ethics IR.SEMUMS.REC.1397.075.
3.1. Participants
Participants were selected from patients with unilateral ankle sprains who had been referred to physiotherapy centers under the supervision of Semnan University of Medical Sciences. Also, the non-probability sampling method was used to select patients. A total of 35 patients (21 males and 14 females) with a mean age of 22.57 ± 2.51, the height of 169.97 ± 9.35 cm, and weight of 70.20 ± 15.55 Kg were included according to inclusion and exclusion criteria. The injured and healthy legs were evaluated as the experimental and control groups, respectively.
Inclusion criteria included (1) no reported pain at the beginning of the study (both legs) (12); (2) no history of injury to the healthy ankle and history of sprain to another ankle of participants in the last 6 months (grade II of ankle sprain based on the anterior drawer test and talar tilt test); (3) a history of 2 times giving way in the injured foot in the last 6 months (1, 11); and (4) the ability to painless complete weight-bearing by patients(both legs) (13). Exclusion criteria also included (1) any history of musculoskeletal disorders (fracture, dislocation) and any type of neurological disorders (both legs); (2) any visual and vestibular system disorders (14); (3) any history of lower limb surgery (both legs); and (4) any systematic disorders such as diabetes (13). Moreover, we excluded participants who used the drugs affecting balance such as sedative or/and hypnotic. At baseline, sufficient explanations were given to the participants about how to perform the test and all participants signed an informed consent form to participate in the study.
3.2. Measurement
Biodex balance system (model: 950-302, Shirley, New York, USA), a digital scale, and tape measure were used to perform the study and collect data.
To analyze the reliability of the studied variables, the reliability coefficient tests were performed as test-re test. A total of 10 patients were randomly selected and re-measured one week after the first valuation. Their results show good to excellent credibility of the balance index.
The test was performed in such a way that the participants stood on one leg on the Biodex device while the second toe was at a 10-degree angle to the outside and the hands were crossed on the chest. The level of difficulty of the Biodex force plate was selected 10 (numbers 12 and 1 show is the most stable and most unstable levels, respectively). Patients were then asked to look at the screen in front of them and move the cursor to specific points on the screen and then the device would confirm and the next direction would appear on the screen. The six distinct points on the screen included anterior, posterior, medial, lateral, anterolateral, and posterolateral directions. This test was performed three times separately for each healthy and unhealthy leg and 5-minute rest was considered between tests. The duration of each test depended on the degree of instability of the patient, so that participants with more instability spend more time performing the test. Finally, the mean data were recorded for analysis.
3.3. Statistical Methods
A study by Rahnama et al. (1) was used to estimate the sample size. Therefore, with mean of 2.69 ans standard deviation of 0.65 for mediolateral stability index in patients with functional ankle instability and a 90% confidence interval, the sample size was estimated at 35 people. Kolmogorov-Smirnov statistical test was used to investigate the normal distribution of data and a t-test was used to compare between healthy and unhealthy legs. P-value- < 0.05 was considered as the significance level in all tests.
3.4. Statistical Findings
Table 1 shows the distribution of anthropometric variables among participants.
| Variables | Mean ± SD | 95% Confidence Interval | |
|---|---|---|---|
| Lower | Upper | ||
| Age (y) | 22.57 ± 2.512 | 1.198 | -1.198 |
| Weight (kg) | 70.20 ± 15.556 | 7.420 | -7.420 |
| Height (cm) | 169.97 ± 9.357 | 4.463 | -4.463 |
Table 2 shows the reliability of the measuring methods of the studied variables.
| Variables | Healthy Leg | Injured Leg | CI (Lower, Upper) | ||
|---|---|---|---|---|---|
| ICC | P Value | ICC | P Value | ||
| Overall score | 0.736 | 0.057 | 0.760 | 0.014 | 0.940, 0.034 |
| Time | 0.859 | 0.043 | 0.837 | 0.030 | 0.935, 0.059 |
According to the Table 2, indices measured in the present study have acceptable credibility.
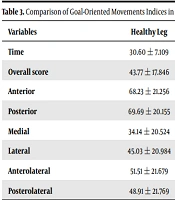
Table 3 shows the values obtained from the indices of goal-oriented movements in healthy and injured legs.
| Variables | Healthy Leg | Injured Leg | 95% CI (Lower, Upper) | P Value |
|---|---|---|---|---|
| Time | 30.60 ± 7.109 | 36.49 ± 11.860 | -9.068, -2.704 | 0.000 |
| Overall score | 43.77 ± 17.846 | 30.71 ± 16.568 | 10.777, 15.337 | 0.000 |
| Anterior | 68.23 ± 21.256 | 54.63 ± 22.436 | 5.793, 21.407 | 0.005 |
| Posterior | 69.69 ± 20.155 | 67.74 ± 19.634 | -6.967, 10.853 | 0.389 |
| Medial | 34.14 ± 20.524 | 27.74 ± 20.282 | 1.087, 11.713 | 0.020 |
| Lateral | 45.03 ± 20.984 | 34.31 ± 24.503 | 5.690, 15.738 | 0.000 |
| Anterolateral | 51.51 ± 21.679 | 47.97 ± 19.484 | -3.029, 10.114 | 0.281 |
| Posterolateral | 48.91 ± 21.769 | 46.06 ± 18.950 | -3.439, 9.153 | 0.363 |
According to the Table 3, a significant difference was observed in the anterior, medial, and lateral directions in the healthy leg compared to the unhealthy leg (P < 0.05), but there was no significant difference between healthy and unhealthy legs in posterior, posterolateral and anterolateral directions (P > 0.05).
4. Results
According to the data interpretation, there is a significant difference between healthy and unhealthy legs in terms of quality and duration of goal-oriented movements. The results show that the duration of goal-oriented movements on the Biodex device in the injured leg is approximately 6 seconds longer than the healthy leg and the quality score of the movements in the injured leg is approximately 13% less than the healthy leg.
5. Discussion
The present study aimed to compare goal-oriented movements in healthy and injured legs in patients with a unilateral ankle sprain. The results showed a significant difference between the healthy and injured legs of the participants in terms of the overall score of the stability index, especially, in the anterior, medial and lateral points, meaning that the stability of the injured leg was lower than the healthy leg in these points.
Some researchers have performed the postural evaluation using a Biodex device in patients with ankle sprains (7, 10, 11). The results show that the more difficult the test, the greater the difference in balance performance between the injured and healthy legs (7) or between the group with ankle instability and the control group (10, 11, 15). According to the results, it was observed that in some directions, lower limb function is not appropriate, which may be secondary to sensory or motor disorders or central processing. Previous studies have shown weakness in some lower limb muscles in patients with ankle sprains (16-18) and since muscles have Fx, FY, and FZ components, the combination of these components causes proper function in the motor directions. The muscles passing through the ankle joint are responsible for joint stability during static and dynamic activities. Therefore, weakness in the activity of these muscles can affects postural control and balance in different directions. Since tibialis anterior and peroneus longus muscles act on the frontal plate (as invertor and evertor respectively), changes in the activity of these muscles are can related to the postural control in the mediolateral direction. More tibialis anterior muscle activity and reduced peroneus longus muscle activity in people with ankle sprain disrupt the muscular balance and weaken postural stability in the mediolateral direction. This argument also is valid in relation to gastrocnemius and soleus muscles with tibialis anterior muscle. The gastrocnemius and soleus muscles activity decreased as plantar flexor of ankle, and the tibialis anterior muscle activity increased as dorsiflexor of ankle. Given the fact that both dorsiflexion and plantar flexion are performed on the sagittal plane, the changes in the muscles activity cause a muscular imbalance in the anterior-posterior direction and decrease the postural control in this direction (16). In another study, Rahnama et al. investigated the balance in 15 individuals with functional ankle instability and 15 healthy individuals using a Biodex device. They stated that the postural stability in overall and mediolateral indices is weaker in patients as compared to the control group (1). Rozzi et al. compared the one-leg standing performance using a Biodex device in 13 patients with functional ankle instability and 13 healthy individuals and stated that patients with poor postural stability had a weaker overall index than controls (10). In another study, Mettler et al. investigated the effect of 4-week balance training on people with chronic ankle instability and the change in the center of pressure using a force plate device. They stated that the center of pressure is in the anterior part more frequently, which shifts to the posterior part after performing balance exercises. A change in the center of pressure has occurred on the sagittal plane. The researchers hypothesized that the anterior positioning associated with ankle instability before balance training was due to a more dorsiflexed talocrural joint and a more supinated subtalar joint; both of these represent the joints’ closed-packed positions as associated with the most mechanically stable joint congruency. However, this positioning moves the COP closer to the lateral border of support and consequently decreases the amount of time available for postural corrections in this direction (4). In another study Becker et al. found that patients with functional instability also showed significantly increased lateral loading of the unstable foot. They suggested this to be due to reduced peroneal strength during the stance phase as the result of a proprioceptive deficit caused by injury (19). However, Thompson et al. suggested that the change could also be a means of compensating for the lack of sensory input from the damaged lateral ligaments by stretching the soleus muscle and thus increasing muscle-spindle sensitivity. By increasing the sensitivity of the soleus muscle spindle, those with CAI may be able to better adjust to postural perturbations (20). Besides, Pope et al. proposed that persons with chronic ankle instability (CAI) adopt the closed-packed position as a protective compensation to provide more postural stability by limiting (or ‘‘freezing’’) movement degrees of freedom at the ankle and subtalar joints in the presence of sensorimotor deficits associated with CAI (21). Therefore, the results of the mentioned research are consistent with those of the present study. When investigating ankle sprains, another important variable is reaction time, which is an essential element in joint protection against sudden unexpected excessive movement requiring fast and coordinated muscle action (22). The time latency from the onset of ankle inversion to the onset of the peroneus longus response is known as peroneal latency (23). Consistent with the results of the present study, which showed that the duration of goal-oriented movements in the injured leg was approximately 6 seconds longer than that in the healthy leg, van Cingel et al. compared muscle latency using an isokinetic dynamometer device in 11 subjects with chronic ankle instability and 11 healthy subjects. They stated that the time latency of peroneal muscles increases in patients (22). Several other studies have also confirmed an increase in peroneal latency in individuals with ankle instability (24-27). Finally, the results of the present study show that the overall balance index score in the unhealthy leg is about 13% lower than in healthy legs. In a similar study aimed at investigating balance using a Biodex device in 30 athletes with ankle sprains, Akbari et al. found that the static balance in the involved leg was 12.7 percent lower than in the healthy leg, and this balance problem could be due to impaired proprioception (28).
5.1. Conclusions
Impaired postural control is associated with an increased risk of an ankle injury. Therefore, accurate evaluation of stability indices in these patients seemed necessary and according to the results of this study, it can be stated that the goal-oriented movements in the anterior, medial and lateral directions in the injured leg are more affected than the healthy leg and using these findings an appropriate rehabilitation program can be selected for patients to prevent further injury and recurrence.
5.2. Limitations and Suggestions
Due to problems and time constraints, people with unilateral ankle sprain were included in the present study, so it was not possible to compare between a healthy person and a patient.
- The results of the present study cannot be generalized to people with a bilateral ankle sprain. Therefore, it is recommended to compare the goal-oriented movements between people with lateral ankle sprains and people with both healthy legs.
- Since the rehabilitation process in these patients must be completed, it is recommended that therapeutic exercises be taught to patients and their importance be emphasized.
- It is suggested that researchers in future studies examine the association between impaired motor directions with motor or sensory impairment or central processing.