1. Context
Shoulder pain is a musculoskeletal problem and a common cause of presenting to clinics (1). Shoulder pain interferes with occupation and daily activities by limiting the range of motion and causing shoulder impairment (2). Neer defined shoulder impingement syndrome (SIS) as pressure on the rotator cuff tendons and associated tissues in the subacromial space (3). As the most prevalent diagnosis in shoulder pain (4), SIS causes disability and degrades quality of life (5). SIS can seriously damage the rotator cuff and joints (6). Different anatomical and biomechanical factors have been reported for the multifactorial etiology of SIS (7). Normal shoulder function depends on the coupled and coordinated movement of the glenohumeral and scapulothoracic joints and requires the proper orientation and control of scapular movements on the thorax, which is crucial for the optimal scapular and rotator cuff muscular activity and humeral movements (8, 9). Changes in a component of the shoulder girdle affect the kinematics of the entire chain and cause shoulder malfunction (10). Normal scapulothoracic motions during upper limb elevation include upward rotation, posterior tilting and external rotation (11). Impaired scapular kinematics can decrease the rotator cuff strength and subacromial space and increase the risk of SIS (12).
Despite the numerous studies conducted on scapular kinematics in SIS, the findings were inconsistent in terms of differences in scapular kinematics between patients with SIS and asymptomatic subjects (13, 14). A systematic review conducted in September 2015 on the effect of musculoskeletal shoulder conditions on scapular kinematics did not include meta-analyses and revealed increases in scapular posterior tilt and external rotation during abduction and decreases in scapular upward rotation during scapular plane elevation in SIS (13). This review included studies recruiting athletes or non-athletes and those evaluating scapular kinematics in a static position or dynamic movements. According to sport-specific adaptations in athletes and dynamic nature of arm movements (15, 16), reviewing articles on non-athlete patients with SIS and evaluating scapular kinematics during dynamic arm elevation are crucial. Given the growing body of literature on scapular kinematics, conducting a systematic review and meta-analyzing the data for a decisive conclusion appeared essential.
2. Objectives
This systematic review and meta-analysis aimed to compare scapular kinematic patterns between patients with SIS and asymptomatic individuals during arm elevation.
3. Data Sources
This review was performed based on the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) (17). The protocol of this study was registered at the International Prospective Register of Systematic Review (PROSPRO) (CRD42020177286) (18).
3.1. Information Sources
A.H. searched databases such as PubMed, Scopus, Web of Science, Ovid, Embase and PEDRO from January 1995 to June 2021. Hand-searching was also conducted through the references of the included articles.
3.2. Search Strategy
The keywords used included “subacromial pain syndrome” and “scapular kinematic”, and their synonyms were obtained using medical subject heading (MeSH) terms, free text word and expert comments. Appendix 1 provides The PubMed search syntax. Appropriate changes were made in the basic search syntax to optimize the search strategy for the other databases.
4. Study Selection
4.1. Selection Process
The inclusion criteria for selecting the articles comprised being observational and written in English, recruiting asymptomatic subjects and patients with SIS, diagnosing SIS based on the clinical evaluations performed by professionals and physicians, comparing scapular kinematics during arm elevation between patients with SIS and healthy individuals, outcomes such as scapular kinematics, i.e. upward rotation, external rotation and posterior tilt, measured using a motion analysis system (electromagnetic, marker-based or inertial sensors) during dynamic arm elevation in at least one plane of movement (sagittal, frontal, or scapular). The excluded articles consisted of those addressing nonspecific shoulder pain, rotator cuff rupture or scapular kinematics in a static position or during daily activities such as reaching, grasping and hair combing or recruiting non-adults, athletes or cadavers.
After completing the search, the articles were imported into EndNote and duplicates were removed. Two reviewers, i.e. A.H. and S.SH. screened the titles and abstracts to determine eligible studies for the next stage. A.H. and S.SH. then confirmed the eligibility criteria by reviewing the full text of the articles.
4.2. Study Risk of Bias Assessment
Two of the authors assessed the risk of bias in the included articles using the modified Downs and Black checklist, which helps have moderate-to-good interpreter reliability (19). The maximum total score of this checklist is 15 and every item is scored as 1: good description or 0: unclear or no description. The articles receiving a score of at least 12 were considered high quality, 10 - 11 moderate quality and at most 9 low quality (20). Any disagreements between the two authors in the selection and risk of bias assessment were resolved through discussion. A third reviewer resolved the conflict in case the two reviewers did not reach agreement.
5. Data Extraction
The standard data extraction was performed by describing the article’s characteristics, i.e. first author’s name, publication date and sample size, describing the participants in terms of BMI, dominant hand, gender and mean age, determining the diagnostic criteria for SIS, test procedure and kinematic outcome measures and explaining the significant results and mean degree of scapular upward/downward rotation, scapular anterior/posterior tilting and scapular internal/external rotation during arm elevation (flexion, extension and scaption). The two authors independently extracted the data. Efforts were made to obtain missing data from the corresponding authors and unavailable mean and standard deviation values were calculated using the other available data. The data were manually extracted by digitizing the diagrams using the WebPlotDigitizer application (https://automeris.io/WebPlotDigitizer/) for the articles that did not report numerical data.
5.1. Synthesis Method
The random-effect model was used to evaluate 95% confidence intervals and to calculate pooled effect sizes (ES) reported as standardized mean difference. Cohen’s d ES was used and interpreted as follow, small (0.2 - 0.5), moderate (0.5 - 0.8), and large (> 0.8). The presence of heterogeneity was assessed by I 2 statistics. The heterogeneity considered very high if I2 ≥ 75%, high I2 ≥ 50%, moderate 25 < I2 < 50 and low I2 ≤ 25%. In case of high heterogeneity across studies to find the source of heterogeneity, sensitivity analyses including leave-one-out approach by omitting each study and subgroup analyses based on direction of movement (flexion, abduction and scaption) and degree of arm elevation (30, 60, 90, 120) was performed.
A symmetric funnel plot was used to assess the publication bias and Egger’s regression test to examine funnel plot asymmetry at a one-tailed significance level of P > 0.05. The trim-and-fill method was employed to adjust for missing studies in case of publication bias.
6. Results
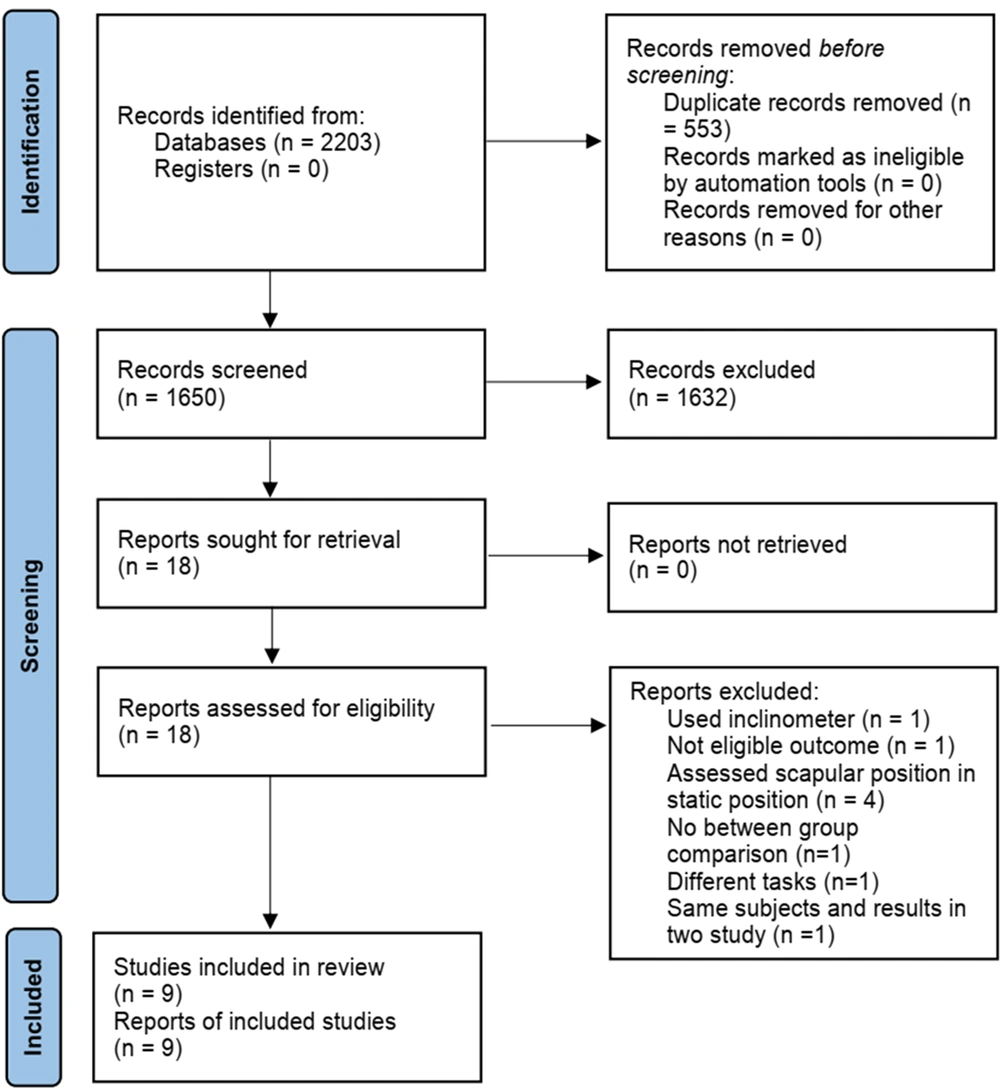
After eliminating the duplicates, 1650 out of 2203 retrieved articles remained for screening their title and abstract. Eighteen articles underwent a full text review and nine ineligible ones were excluded. Manual search did not include any studies and nine eligible articles were ultimately included in this systematic review as per Figure 1.
6.1. Risk of Bias Assessment
Table 1 presents the risk of bias summary of the included articles. High quality was assigned to 11% of the included studies, moderate quality to 33% and low quality to 56%. A high risk of bias was observed in the majority of the articles in sampling and controlling confounders such as arm dominancy and type of activity. Some of the included study did not report the time/location of recruitment and some recruited their subjects from a local health center or hospital that did not represent the entire population.
| Study | 1 a | 2 b | 3 c | 5 d | 6 e | 7 f | 10 g | 11 h | 12 i | 16 j | 18 k | 20 l | 21 m | 22 n | 25 o | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ludewig and Cook (21) | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 10 |
| McClure et al. (22) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 10 |
| Lawrence et al. (23) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 10 |
| Keshavarz et al. (24) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 9 |
| Kolk et al. (25) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 12 |
| Turgut et al. (26) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 9 |
| Rossi et al. (27) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 9 |
| Rosa et al. (28) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 9 |
| Rossi et al. (29) | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 9 |
A Summary of Risk of Bias Assessment of the Included Studies
6.2. Overview of Participant Characteristic and Methodology Consideration
According to the summary in Table 2, most of the studies defined SIS as pain in the lateral area of the shoulder with painful arch and at least three positive impingement signs (the painful arch tests in flexion or abduction, Neer or Jobe test, Hawkins-kennedy test, and painful resisted lateral rotation). Kolk et al. performed MRI to exclude participants with other diagnoses such as complete rotator cuff tear, calcific tendonitis and labrum pathology (25). The SIS symptoms in the articles were found to last one or six weeks, or at least three months. The majority of the studies failed to provide information on the dominance distribution or reported mismatch between the two groups in this regard. McClure et al. (22) and Rossi et al. (27), however, reported matched limb dominance between groups. Range of motion of over 130° in arm elevation was considered an inclusion criterion in four of the studies (21, 26, 28, 30). The other studies did not report the minimum range of elevation for inclusion.
| Study’s Characteristics | Participants’ Characteristics | Task and Test Procedure | Outcomes Measures | Reliability | Significant Results |
|---|---|---|---|---|---|
| Ludewig and Cook (21) (USA) | 26 healthy, 26 SIS | Test position: standing Task: scaption in 3 condition no external load, 2.3 and 4.6 kg load | Scapular muscle EMG activity, 3D motion of scapula and humerus | ICC between day: 0.93 - 0.98 | Decrease UR in 60° arm elevation and PT in 120°. Decrease ER in loaded elevation. Increase UT and LT EMG activity in 61°-90° and 91°-120°. |
| McClure et al. (22) (USA) | 45 healthy, 45 SIS | Test position: standing Task: scaption, flex, ER with the arm at 90 degrees of elevation in the frontal plane | Shoulder ROM and muscle force, thoracic posture, shoulder kinematic | NR | Increase UR in 90° - 120° flexion and 90° scaption. Increase PT in 120° scaption. Increase clavicular elevation in 90° - 120° flexion. Increase clavicular retraction in 120° scaption. |
| Lawrence et al. (23) (USA) | 12 healthy, 10 SIS | Test position: standing Task: scaption, flexion, abduction | Kinematic of Scaplothoracic, acromioclavicular and sternoclavicular joints | ICC Within day Control: 0.83 - 0.98 SIS: 0.76 - 0.96 | Decrease UR in 30° and 60° of elevation in frontal and scapular plans. Decrease Sternoclavicular protraction in all phase planes and angles. Decrease Sternoclavicular elevation in 30° scaption. |
| Keshavarz et al. (24) (Iran) | 13 healthy, 15 SIS | Test position: sitting Task: scaption, flexion, abduction with 1 kg external load. | scapular translation and ROT | ICC intra-rater reliability 0.64 - 0.94 SEM: 3.2 - 5.7 mm and 2.9° - 8.8° | Decrease UR in 30° - 90° abduction and 30° scaption. Decrease PT at 30° flexion Decrease scapular lateral translation in 90° and 110° abduction |
| Kolk et al.(25) (Netherlands) | 34 unilateral SIS | Test position: sitting Task: bilateral abduction | scapular kinematic in affected and non-affected side and in affected side after sub-acromial anesthetic | NR | Increase IR in 110°-120° abduction. Increase IR and decrease PT in 110° - 120° abduction after anesthetic |
| Turgut et al. (26) (Turkey) | 37 healthy, 29 unilateral SIS | Test position: standing Task: bilateral Flexion | scapular kinematic in control and SIS group in both side | ICC Within day without removal of sensor 0.88-0.97 | Decrease UR in 120° and PT in 60°, 90° and 120° compare to control and in all angle compare to asymptomatic side. Decrease ER and UR in dominant side of control group. scapular movement was more asymmetrical for IR and UR in individuals with SIS when compared with healthy controls |
| Rossi et al. (27) (Brazil) | 25 No pain, 25 No pain + SD, 25 SIS, 25 SIS + SD | Test position: standing Task: Flexion | scapular kinematics in SIS and in asymptomatic participants with and without SD | NR | Pain and no pain (no SD) had less PT throughout the elevation in comparison to the No Pain + SD group. Pain + SD group had less PT throughout the arm-lowering phase than the No Pain + SD group. During the arm-lowering phase asymptomatic participants with SD had different scapular motion and showed increased PT compared to symptomatic participants with SD |
| Rosa et al. (28) (Brazil) | 28 No pain, 27 No pain + PCT, 25 SIS, 25 SIS + PCT | Test position: standing Task: Flexion | Scapular kinematics and humeral translations Shoulder IR and ER ROM, ER strength, and pain and SPADI | ICC Within day for humeral translation: 0.85 | Decrease scapular ER. Increase PT in comparison with PCT. Decrease humeral ant translation than the other group. Groups without PCT had greater IR ROM. |
| Rossi et al. (29) (Brazil) | 50 healthy, 47 SIS | Test position: standing Task: bilateral abduction | Scapular kinematic (3 ROT and 3 translation and angular velocity) | Between day ICC: control: 0.58- 0.88 SIS: 0.54 - 0.85 SEM: Control: 3.37° - 6.79° SIS: 3.62° - 7.44° | Decrease PT in elevation and lowering phase. Increase forward/backward translation in lowering phase. Change anterior tilt angular velocity. |
Summary of the Included Studies
6.3. Meta-analysis
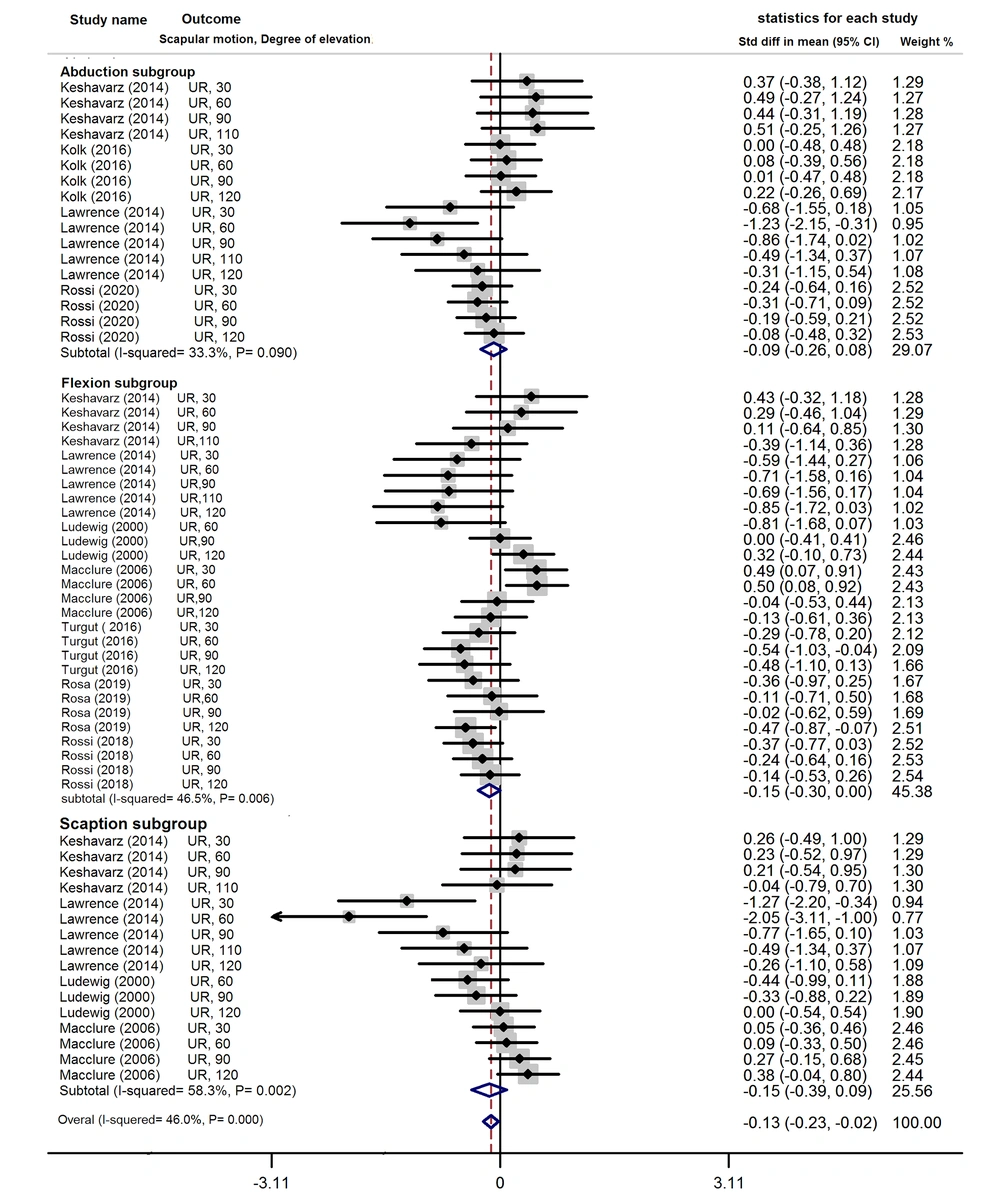
6.3.1. Upward Rotation
A low effect size and moderate heterogeneity were obtained from a meta-analysis of scapular upward rotation [SMD = -0.13, 95% CI= -0.23 to -0.02 (I2 = 46%)] (Figure 2). The subgroup analysis of the arm movement direction showed a lower upward rotation in the sagittal plane and a low effect size [SMD = -0.15, 95% CI = -0.30 to 0.00 (I2 = 46.5%)] in the patients with SIS than in the healthy subjects. No differences were observed between the groups in the abduction (SMD = -0.09, 95% CI = -0.26 to 0.08) and scaption (SMD = -0.15, 95% CI = -0.39 to 0.09) and low heterogeneity was obtained in the abduction and scaption among the studies [(I2 = 33.3%, I2 = 58.3%]. The Funnel plot and Egger’s test revealed potential publication bias (P = 0.005). The trim-and-fill analysis also showed no missing studies.
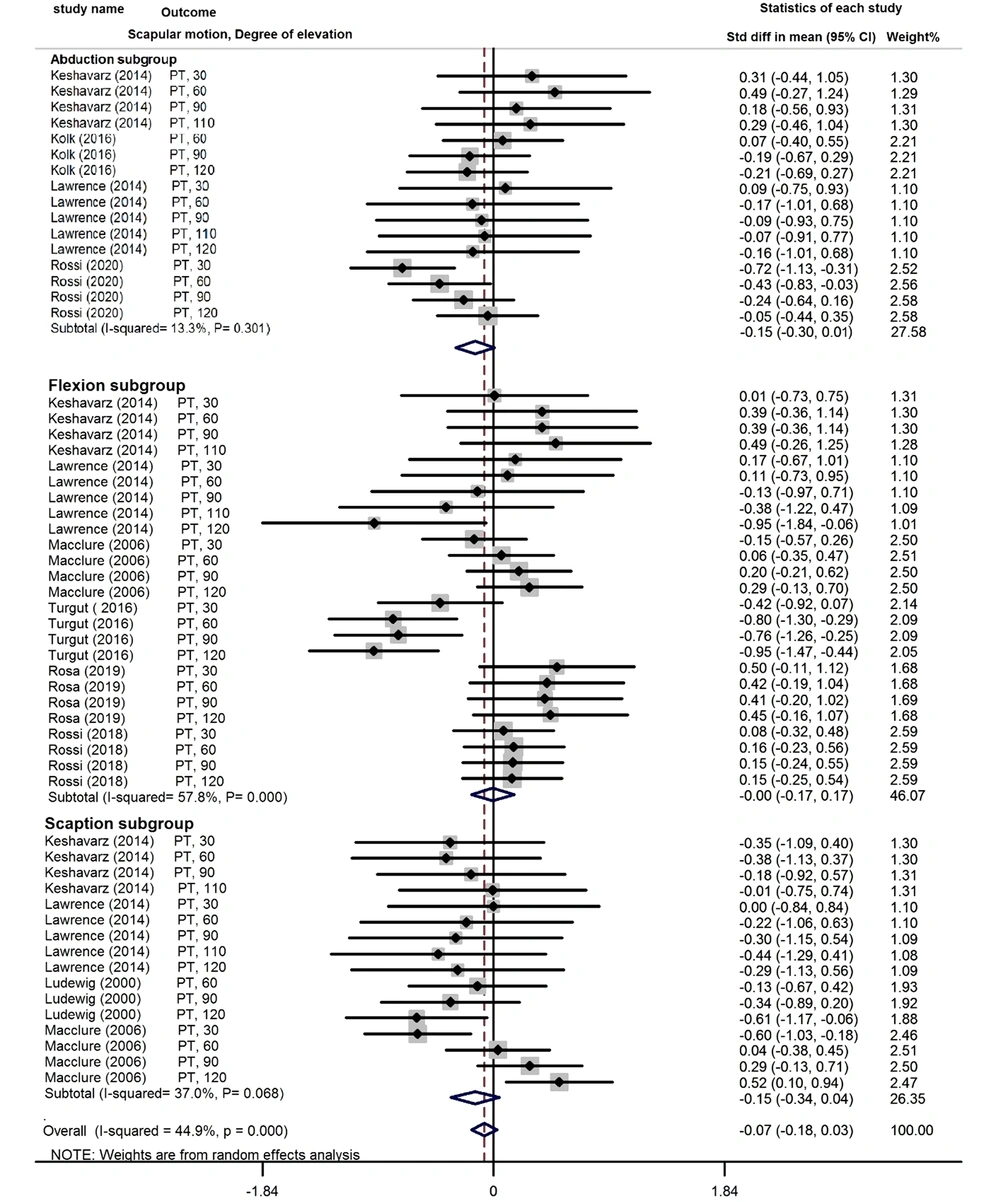
6.3.2. Posterior Tilt
The overall effect size estimated for scapular posterior tilt with moderate heterogeneity showed no differences between the patients with SIS and healthy subjects during arm elevation (SMD = -0.07, 95% CI = -0.18 to 0.03 I2 = 44.9%) (Figure 3). The subgroup analysis of the arm elevation direction revealed no significant differences in the posterior tilt between the patients with SIS and asymptomatic subjects during flexion (SMD = -0.00, 95% CI = -0.17 to 0.17 I2 = 57.8%), abduction (SMD = -0.15, 95% CI = -0.30 to 0.01 I2 = 13.3%) and scaption (SMD = -0.15, 95% CI = -0.34 to 0.04 I2 = 37%). The Egger’s test also showed no publication bias (P = 0.896).
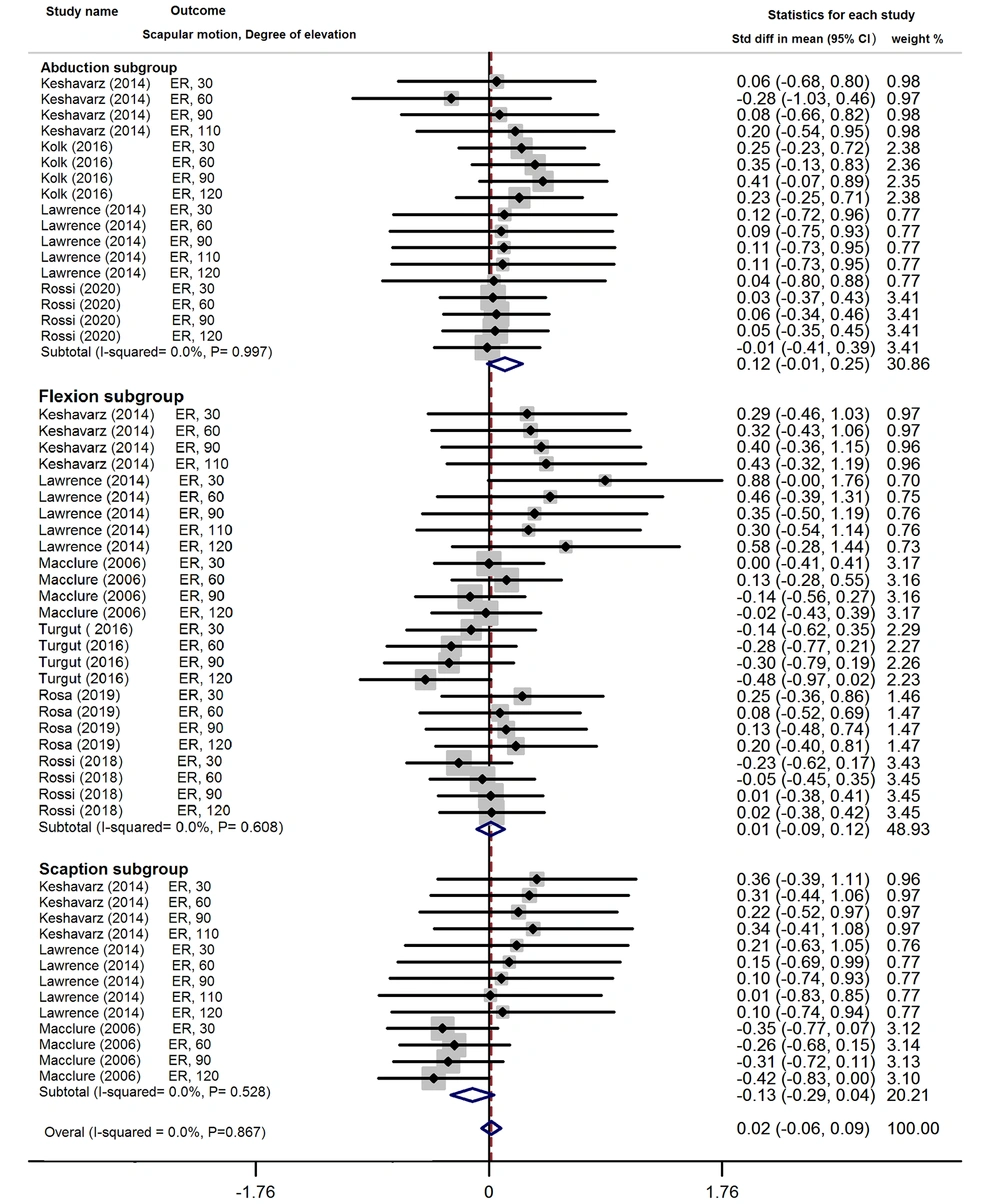
6.3.3. External Rotation
No significant differences were found between the healthy subjects and patients with SIS in terms of scapular external rotation during arm elevation (SMD= 0.02, 95% CI= -0.06 to 0.09) (Figure 4). The subgroups analysis of each direction showed no significant differences in the flexion (SMD = 0.01, 95% CI= -0.09 to 0.12, I2=0%), abduction (SMD= 0.12, 95% CI= -0.01 to 0.25) and scaption (SMD= -0.13, 95% CI= -0.29 to 0.04). A low heterogeneity among the studies was obtained in scapular external rotation in three planes of arm elevation (I2 = 0%). The funnel plot and the Egger’s test showed publication bias (P < 0.001). The trim-and-fill method used to retrieve five missing studies changed the effect size to -0.075 (95% CI -0.14, -0.004) after adjustment for publication bias.
Sensitivity analyses and the subgroup analysis based on degree of arm elevation did not decrease heterogeneity. Standardized mean differences were also insignificant along all directions of arm elevation for these groups.
7. Discussion
Except for scapular upward rotation, scapular movement was generally insignificantly different between the subjects with and without SIS during arm elevation as the meta-analysis conducted. The two groups were not different in scapular external rotation and posterior tilt in all directions and degrees of arm elevation. The low scapular upward rotation obtained was in line with the reports by Keshavarz et al. (13) and Timmons et al. (31). In contrast, Keshavarz et al. (13) reported a high scapular posterior tilt in SIS, and Timmons et al. (31) reported a lower scapular external rotation in patients with SIS than in asymptomatic subjects. The inconsistency among the results of different studies can be attributed to differences in the type of motion, i.e. static or dynamic, and study population, i.e. athletes or non-athletes. Given differences in scapular kinematics between athletes and non-athletes and between static positions and dynamic movement (15, 16), the present systematic review addressed non-athletes and included articles that evaluated scapular kinematics during dynamic arm elevation for a decisive conclusion. Moreover, the results revealed that differences in the scapular upward rotation between the patients with SIS and asymptomatic individuals can be affected by the plane of arm elevation. Previous studies showed that dyskinesia is more obvious during arm elevation in sagittal plane and symptomatic individuals represent dyskinesia in this plane of movement (32, 33).
According to theoretical knowledge, scapular kinematic alterations such as decreased scapular upward rotation, posterior tilt and external rotation cause subacromial compression (12, 34). This review, however, found differences between the patients with SIS and asymptomatic individuals only in terms of upward rotation of the scapula. Given SIS as a multifactorial condition that is not exclusively caused by biomechanical factors (35), different methodological factors can mask scapular kinematic differences between two groups. The results of most of the included articles could have been affected by their high risk of bias in controlling confounders such as matching the groups based on type of activity, arm dominancy and BMI. Given differences in scapular kinematics between the two sides, research suggests a lower scapular upward rotation and posterior tilt on the non-dominant than the dominant side (36, 37). The results of comparing patients with SIS and asymptomatic subjects can be therefore affected by the dominant side, which was not controlled in most of the studies. A significantly higher scapular upward rotation during arm elevation was reported in individuals with BMI > 27 kg/m2 compared to in those with BMI ≤ 23 kg/ m2 (38). In contrast, the majority of the included articles failed to address the potential effects of BMI on the results.
A systematic review showed changes in scapular kinematics in the rotator cuff tear and found more tissue damage to cause more scapular dysfunction (39). The majority of the studies included in the present review used clinical tests to diagnose SIS. These tests only ruled out glenohumeral instability, cervical referral pain and frozen shoulder and failed to identify the exact tissues involved and differentiate between rotator cuff tendinopathy and tear (12), which might have affected the results. Failing to investigate postural alignment, especially spinal thoracic curvature and rounded shoulder, and pectoralis muscle length in any of the studies might have also changed scapular motions and orientation in the healthy individuals (40). Moreover, selection bias associated with the sampling method might have influenced the results.
The scapular kinematic alterations reported in asymptomatic individuals with normal arm movements might have caused negligible between-group differences (41). The other limitations comprised inherent between-individual variations and including patients with SIS and without shoulder range of motion limitations.
Several articles were found to have identified the effect of fatigue on scapular kinematic alterations during repeated movements (42, 43); nevertheless, none of the studies compared scapular kinematics between patients with SIS and asymptomatic subjects under these circumstances. Repeated movement and examining the kinematics of the scapula in fatigue conditions may present the between-group differences obviously, which is suggested for future studies. The present findings can assist clinicians in gaining knowledge of scapular kinematic alterations during arm elevation in patients with SIS. These patients should be treated by considering numerous effective factors in scapular kinematics.
The limitations of the present systematic review included retrieving only articles published in English and peer-reviewed journals, which can cause publication bias. The subjects of the included studies were non-athlete, however, some of the studies did not exclude overhead workers. Therefore, the results might have been also affected by the population type. Sample size was not justified by power analysis in most of the included studies. As a result, the external validity of the finding compromised.
8. Conclusions
According to the present review, scapular upward rotation between the patients with SIS and asymptomatic individuals was significantly different and can be affected by the plane of arm elevation. No differences in scapular external rotation and posterior tilt were observed along any directions and degrees of arm elevation between the two groups. Between-group differences might have been overlooked as a result of the high risk of bias in the included studies. The high-quality studies addressing confounders were required to provide a definitive conclusion on the relationship between SIS and scapular kinematics.