1. Background
Coronavirus disease 2019 (COVID-19) is a global healthcare problem that has affected the lives of many people all around the world. The disease, characterized by symptoms such as fever, cough, and acute respiratory failure, is associated with long-term complications and mortality (1). Its most considerable complications are cardiovascular issues, respiratory problems, neurological involvement, and psychological burdens such as COVID-19-related fear, anxiety, and distress (2). Notably, the morbidity and mortality of COVID-19 seem to be higher in people with chronic diseases such as diabetes mellitus (3, 4).
Type-2 diabetes is one of the most common chronic diseases associated with hyperglycemia and metabolic dysfunction. This systemic disease affects one's immune system and predisposes them to a higher risk for infections, including COVID-19 (5). Self-management can improve one's immune system and prevent the adverse effects of COVID-19 for those with diabetes (6). Self-management is a set of behaviors and activities in which people must regularly engage to control their chronic disease and prevent or delay its complications (7). The most critical Diabetes Self-management (DSM) activities are preparing and eating healthy foods, taking medication, doing exercise and physical activity, caring for feet, doing regular follow-ups, communicating with health professionals, self-monitoring blood glucose, and managing disease complications (8).
Facilitating one's participation in DSM requires identifying its related factors. Individual and family factors are the ones that associate with self-management. Psychological factors such as depression, anxiety, and diabetes distress negatively impact DSM (9). Studies conducted after the COVID-19 pandemic showed that some personal characteristics such as age, gender, and body mass index were associated with the self-management of people with diabetes (10). There was, however, no evidence of the association between COVID-19-related personal and familial characteristics, such as COVID-19 vaccination, the history of COVID-19 infection or hospitalization, and DSM behaviors. Previous research has also shown that negative emotional behaviors such as anxiety and stress were prevalent in the COVID-19 pandemic (11), imposing barriers to DSM (10, 12). Nevertheless, no previous study has examined the association between DSM and diabetes distress, depressive symptoms, and COVID-19-related psychological burden. The novelty of this study is the emphasis on DSM regarding the COVID-19-related personal, familial, and psychological factors, and its exciting results are the focus of this article.
2. Objectives
The present study aimed to identify the association between COVID-19-related personal, familial, and psychological factors and the self-management of people with type-2 diabetes. The research questions are as follows:
(1) Is there any relationship between DSM and one's infection or hospitalization due to COVID-19 or the disease vaccination?
(2) Is there any relationship between DSM and having a high-risk family member or one's family members' infection and hospitalization due to COVID-19?
(3) Is there any relationship between DSM and diabetes distress, depressive symptoms, and COVID-19-related fear, anxiety, and distress?
3. Methods
3.1. Study Design and Setting
This cross-sectional study was conducted from November 2021 to February 2022 in Semnan, Iran. The Semnan University of Medical Sciences Ethics Committee confirmed the study procedure (Ethic number: IR.SEMUMS.REC.1400.200).
3.2. Participants
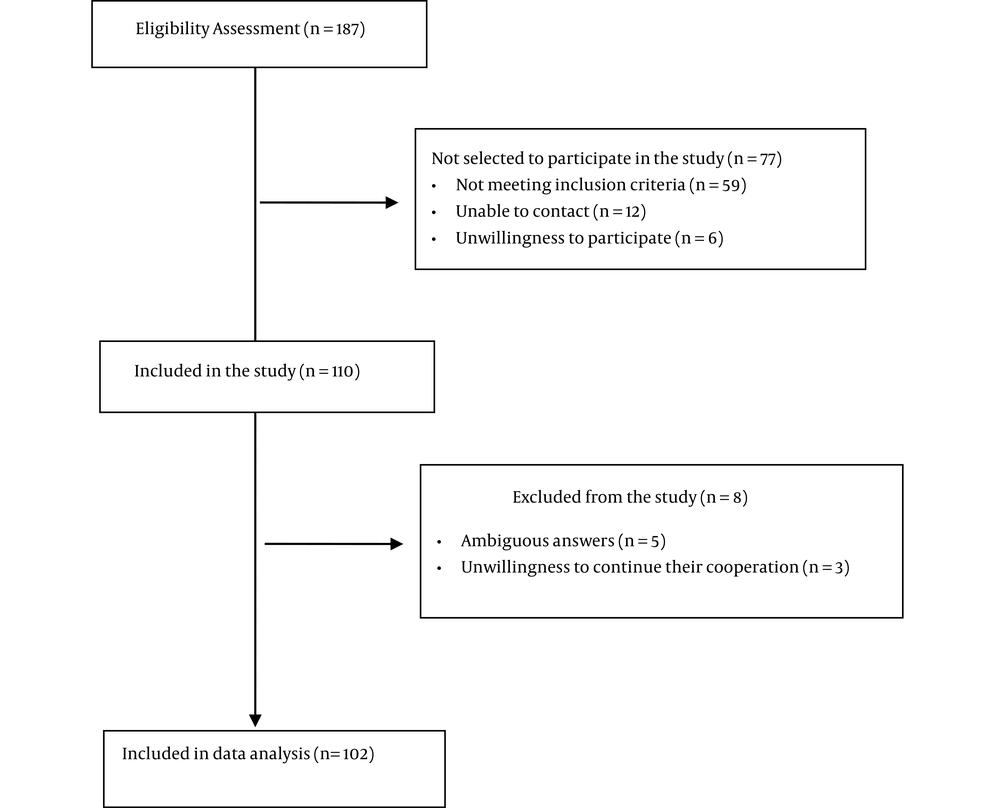
The participants were 102 people with type-2 diabetes selected by simple non-probability sampling (convenience method) from people admitted to the Institute of Endocrinology and Metabolism of Iran University of Medical Sciences. The inclusion criteria were a diagnosis of type-2 diabetes for at least one year, an age of 30 to 65 years, literacy, and no individual or family history of COVID-19 for the past two months. The exclusion criteria were incomplete self-reported information, ambiguity in responding to each item on the scales, and unwillingness to continue cooperation. Figure 1 presents the eligibility criteria for study participants.
3.3. Procedure
The research team explained the research purpose to the participants and received their verbal consent before entering the study. Each participant was interviewed over the telephone for about 20 - 30 minutes. Their personal and familial information was received and recorded in the personal and familial information questionnaire. The other study variables included depressive symptoms, self-management behaviors, COVID-19-related psychological distress, anxiety, fear, and diabetes-related distress, which were then assessed. The reason for the research team to use different psychological questionnaires was to assess multiple aspects of one's psychological burden. To facilitate answering, we asked the participants to write down the scoring items of each questionnaire and then choose the answer among them. The questionnaires with similar content were not stacked in a row to avoid participants' fatigue. It was also possible for the evaluator to end the call and make another after a short break if needed.
3.4. Assessments
3.4.1. Personal and Familial Information Questionnaire
This questionnaire included personal data including age, gender, height, weight, education, diabetes duration, the number of doses of COVID-19 vaccine injection, and the number of times one got COVID-19 or was hospitalized due to the disease. It also asked about one's family information, including the number of family members with chronic diseases and their family members' infections or hospitalizations due to COVID-19.
3.4.2. Diabetes Self-management Questionnaire (DSMQ)
It is a 16-item questionnaire that assesses one's perception of participation in various activities related to diabetes management in four subscales of blood glucose management, regimen control, physical activity, and health care use. Each question is answered on a four-point Likert Scale from 0 (does not apply to me) to 3 (applies to me very much). Scoring the questionnaire and its subscales involves dividing the sums of item scores by the maximum possible score on that item, multiplied by 10. Accordingly, a score closer to 10 indicates more desirable self-management (13). This questionnaire is known to have good psychometric properties in its original (Cronbach’s alpha = 0.84) and Persian versions (Cronbach’s alpha = 0.72, Intra-class correlation coefficient = 0.72-0.81) (13, 14).
3.4.3. Diabetes Distress Scale (DDS)
It is a 17-item questionnaire that measures one's concerns and worries about living with diabetes and its management in four subscales of emotional, physician-related, regimen-related, and interpersonal distress. Each question is answered on a six-point Likert Scale from 1 (not a problem) to 6 (serious problem). The questionnaire scoring requires calculating the mean total and subscale scores, and a lower score indicates a less experience of diabetes distress (15). Previous studies have reported acceptable internal consistency for the original (Cronbach's alpha = 0.93) and Persian versions (Cronbach's alpha = 0.77) of this questionnaire (15, 16).
3.4.4. Patient Health Questionnaire (PHQ)
It is an eight-item questionnaire to assess depressive symptoms in different populations, including diabetics. Each question is answered on a four-point Likert Scale from 0 (not at all) to 3 (nearly every day). Scoring the questionnaire involves calculating the sum of the scores; a lower score represents less depression (17). The original (Cronbach’s alpha = 0.89, Intra-class correlation coefficient = 0.84) and Persian versions (Cronbach’s alpha = 0.86) showed acceptable internal consistency (17, 18).
3.4.5. COVID-19-Related Psychological Distress Scale
It is a 14-item questionnaire that assesses the severity of psychological distress caused by COVID-19 in the general population. Each question is answered on a five-point Likert Scale from 1 (strongly disagree) to 5 (strongly agree). The overall score of the questionnaire is obtained from the sum of the scores, so a higher score shows the greater intensity of psychological distress associated with COVID-19. Both original (Cronbach's alpha = 0.88) and Persian versions (Cronbach's alpha = 0.91) of the questionnaire showed acceptable psychometric properties (19).
3.4.6. Coronavirus Anxiety Scale
It is a five-item questionnaire that assesses the non-functional anxiety associated with COVID-19. Each question is answered on a five-point Likert Scale from 0 (never) to 4 (usually every day). The questionnaire scoring involves calculating the sum of the scores, and a higher score indicates more COVID-19-related anxiety (20). This scale provided acceptable internal consistency in its original (Cronbach’s alpha = 0.93) and Persian versions (Cronbach’s alpha = 0.91) (20, 21).
3.4.7. Fear of COVID-19 Scale
It is a seven-item questionnaire that assesses the severity of one's fears about the COVID-19 pandemic. Each question is answered on a five-point Likert Scale from 1 (strongly disagree) to 5 (strongly agree). Scoring the questionnaire needs to calculate the sum of the scores, and a higher score represents more fears about COVID-19. This questionnaire reported good psychometric properties (Cronbach's alpha = 0.82, Intra-class correlation coefficient = 0.72) and is valid and reliable in the Iranian population (22).
3.5. Statistical Analysis
3.5.1. Power Analysis
Regarding a 5% prevalence of type-2 diabetes in the Iranian population (23), a precision error of 5%, and an Alpha error of 5%, the required sample for this study was calculated to be 72 people according to the following formula. However, our sample size exceeded this number.
3.5.2. Data Analysis
The data were analyzed by SPSS-18 software. Qualitative values were described by numbers and percentages, while means and standard deviations described the quantitative ones. The Kolmogorov-Smirnov test confirmed the normal distribution of all quantitative data. The Pearson correlation test determined the bivariate correlations between the variables. The variables with a significant and higher correlation with self-management were then entered into a multivariate linear regression analysis. The Variance Inflation Factor (VIF) was also conducted to test for collinearity among the variables. A P-value of 0.05 or less was considered statistically significant.
4. Results
4.1. Demographic Characteristics of the Participants
A total of 102 people with type-2 diabetes (63 females and 39 males) with a mean age of 57.22 ± 6.58 years participated in this study. Of them, 51% did not report any history of COVID-19 infection, and 92.2% were not hospitalized due to the disease. Also, 62.7% of the subjects received all three doses of the COVID-19 vaccine. There was only one report of family member infection with COVID-19 in 57.4% of the participants, while 94.1% had no history of family hospitalization due to the disease (Table 1).
| Demographic Variables | Values |
|---|---|
| Age (y) | 57.22 ± 6.58 |
| Gender | |
| Male | 39 (38.2) |
| Female | 63 (61.8) |
| Education b | |
| High school or less | 58 (57.4) |
| Diploma | 32 (31.7) |
| Associate's degree | 6 (5.9) |
| Bachelor's degree | 2 (2) |
| Master's degree | 3 (3) |
| Body mass index (kg/m2) | 27.89 ± 4.89 |
| Diabetes duration (y) | 13.41 ± 7.88 |
| Treatment regimen | |
| Oral medication only | 55 (53.9) |
| Insulin only | 12 (11.8) |
| Both oral medication and insulin | 33 (32.4) |
| Number of times one got COVID-19 | |
| 0 | 52 (51) |
| 1 | 41 (40.2) |
| 2 | 8 (7.8) |
| 3 | 1 (1) |
| Number of one's hospitalizations due to COVID-19 | |
| 0 | 94 (92.2) |
| 1 | 8 (7.8) |
| Doses of COVID-19 vaccine injection | |
| 0 | 2 (2) |
| 1 | 0 (0) |
| 2 | 36 (35.3) |
| 3 | 64 (62.7) |
| Number of times one's family got COVID-19 b | |
| 0 | 35 (34.7) |
| 1 | 58 (57.4) |
| 2 | 7 (6.9) |
| 3 | 1 (1) |
| Number of one's family members' hospitalizations due to COVID-19 | |
| 0 | 96 (94.1) |
| 1 | 6 (5.9) |
| Number of one's family members affected with chronic diseases | |
| 0 | 25 (24.5) |
| 1 | 33 (32.4) |
| 2 | 26 (25.5) |
| 3 | 15 (14.7) |
| 4 | 2 (2) |
| 5 | 1 (1) |
| Self-management behaviors (DSMQ total score) | 6.83 ± 1.57 |
| DSMQ subscales | |
| Blood glucose management | 6.90 ± 2.08 |
| Control of regimen | 6.01 ± 2.19 |
| Physical activity | 7.36 ± 2.30 |
| Health care use | 6.80 ± 1.79 |
| COVID-19-related psychological distress | 44.24 ± 10.87 |
| Coronavirus anxiety | 0.78 ± 2.02 |
| Fear of COVID-19 | 18.13 ± 6.80 |
| Diabetes-related distress (DDS total score) | 1.97 ± 0.97 |
| DDS subscales | |
| Emotional distress | 1.86 ± 1.11 |
| Physician-related distress | 2.11 ± 1.39 |
| Regimen-related distress | 2.05 ± 1.01 |
| Interpersonal distress | 1.80 ± 1.26 |
| Depressive symptoms (PHQ-8 score) | 6.47 ± 5.50 |
Abbreviations: DSMQ, Diabetes Self-management Questionnaire; DDS, Diabetes Distress Scale; PHQ, Patient Health Questionnaire.
a The results are shown as means ± standard deviations or numbers (percentages).
b The valid percent was reported due to missing data.
4.2. Bivariate Correlations Between the Study Variables
4.2.1. Personal Factors
Regarding the DSMQ subscales, the number of times one got COVID-19 or was hospitalized due to the disease had a negative and weak correlation with the regimen control. Doses of COVID-19 vaccine injection were positively and weakly related to physical activity and health care use (Table 2). This variable was also weakly correlated with age (r = 0.324, P = 0.001), one’s family members’ hospitalizations due to COVID-19 (r = - 0.311, P = 0.001), depressive symptoms (r = - 0.250, P = 0.011), total DDS score (r = - 0.228, P = 0.021), and interpersonal distress (r = - 0.242, P = 0.015).
| Variables | DSMQ Total Score | DSMQ Subscales | |||
|---|---|---|---|---|---|
| Blood Glucose Management | Control of Regimen | Physical Activity | Health Care Use | ||
| Age | 0.305** | 0.245* | 0.258** | 0.132 | 0.243 |
| Body mass index | - 0.116 | - 0.031 | - 0.076 | - 0.199 | - 0.131 |
| Diabetes duration | - 0.043 | 0.013 | 0.007 | -0.195* | 0.028 |
| Number of times one got COVID-19 | - 0.113 | 0.012 | - 0.203* | - 0.025 | - 0.098 |
| Number of one's hospitalizations due to COVID-19 | - 0.148 | 0.049 | - 0.302** | < 0.001 | - 0.181 |
| Doses of COVID-19 vaccine injection | 0.170 | 0.098 | 0.065 | 0.207* | 0.228* |
| Number of times one's family got COVID-19 | - 0.208* | - 0.158 | - 0.211* | - 0.120 | - 0.045 |
| Number of family members' hospitalizations due to COVID-19 | - 0.215* | - 0.082 | - 0.195* | - 0.177 | 0.175 |
| Number of family members with chronic diseases | - 0.161 | - 0.62 | - 0.201* | 0.014 | - 0.136 |
| COVID-19-related psychological distress | - 0.013 | 0.005 | - 0.118 | - 0.038 | 0.027 |
| Coronavirus anxiety | 0.068 | 0.090 | 0.077 | 0.035 | - 0.039 |
| Fear of COVID-19 | - 0.169 | - 0.106 | - 0.179 | - 0.141 | - 0.109 |
| DDS total score | - 0.563*** | - 0.469*** | - 0.416*** | - 0.413*** | - 0.339*** |
| DDS Subscales | |||||
| Emotional distress | - 0.352*** | - 0.215* | - 0.278** | - 0.369*** | - 0.200* |
| Physician-related distress | - 0.410*** | - 0.408*** | - 0.295** | - 0.197* | - 0.318*** |
| Regimen-related distress | - 0.655*** | - 0.512*** | - 0.510*** | - 0.416*** | - 0.368*** |
| Interpersonal distress | - 0.354*** | - 0.340*** | - 0.224* | - 0.400*** | - 0.128 |
| PHQ-8 score | - 0.426*** | - 0.227* | - 0.257** | -0.596*** | - 0.254** |
Abbreviations: DDS, Diabetes Distress Scale; PHQ, Patient Health Questionnaire.
a * Pearson correlation with P-value ≤ 0.05; ** Pearson correlation with P-value ≤ 0.01; *** Pearson correlation with P-value ≤ 0.001.
4.2.2. Familial Factors
The number of one's family members' infections or hospitalizations due to COVID-19 had a weak and negative correlation with the DSMQ total score. Regarding the DSMQ subscales, having more high-risk family members with chronic diseases and one's family members' infections or hospitalization due to COVID-19 was negatively and weakly correlated with the regimen control (Table 2). One’s family members’ hospitalizations due to COVID-19 was also weakly correlated with depressive symptoms (r = 0.306, P = 0.002), total DDS score (r = 0.304, P = 0.002), and physician-related (r = 0.275, P = 0.005), regimen-related (r = 0.270, P = 0.006), and interpersonal distress (r = 0.261, P = 0.008).
4.2.3. Psychological Factors
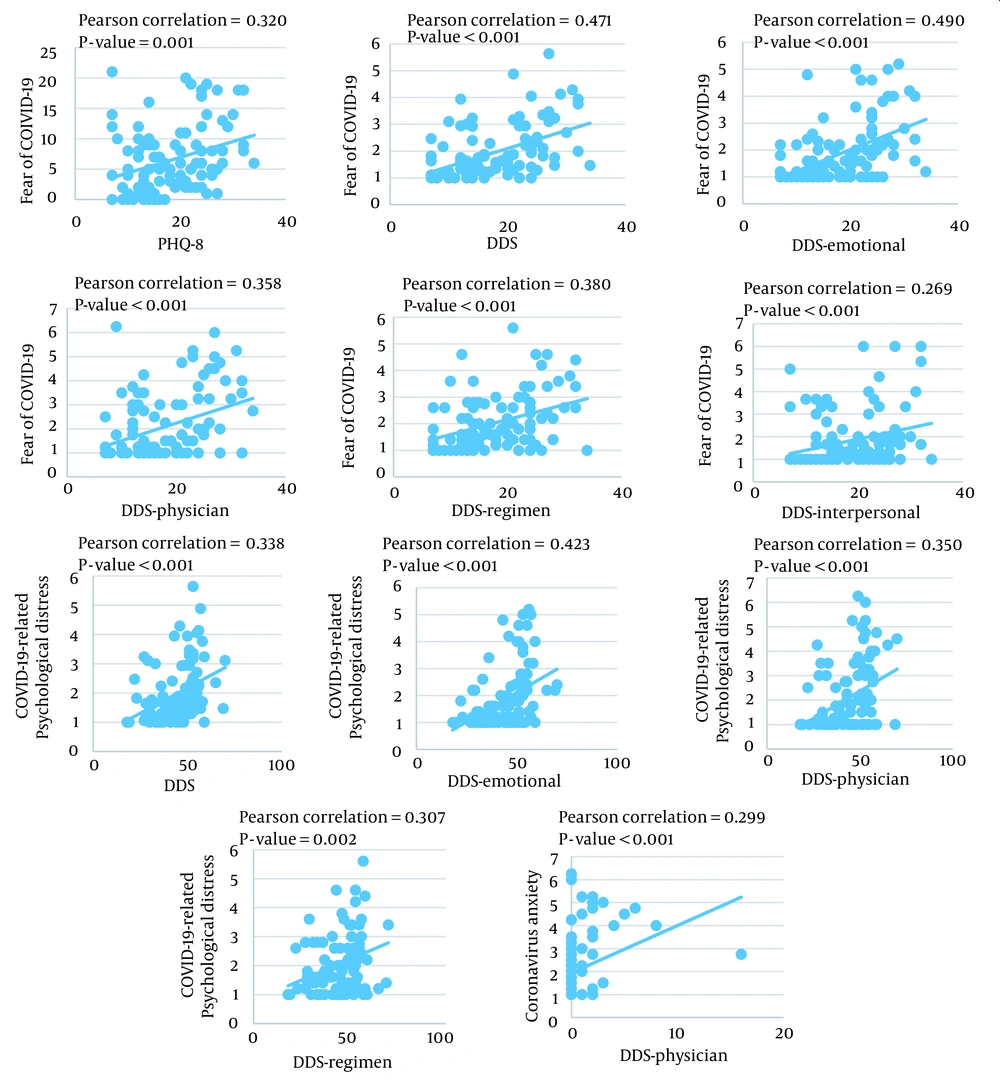
Depressive symptoms, total DDS score, and its subscales were weakly to moderately related to the total DSMQ score and its subscales (Table 2). COVID-19-related fear, anxiety, and distress were significantly correlated (r = 0.317 to 0.712, P < 0.001) but were not associated with DSM. Fear of COVID-19 correlated with depressive symptoms, total DDS score, and DDS subscales. Besides, COVID-19-related psychological distress was associated with the total DDS score and emotional, physician-related, and regimen-related distress. Coronavirus anxiety was significantly correlated with physician-related distress (Figure 2).
4.3. Multivariate Linear Regression Analysis to Predict Self-management
Table 3 presents the modeling of factors associated with self-management behaviors in people with type-2 diabetes (Adjusted R2 = 96%, P< 0.001). After adjusting for confounding variables, there were significant relationships between the total DSMQ score and blood glucose management, regimen control, health care use, physical activity, regimen-related distress, interpersonal distress, COVID-19-related psychological distress, and the number of family members with chronic disease. There was no collinearity among these variables.
| Variables | Correlations | Unstandardized Coefficients | Standardized Coefficients | P-Value | Collinearity Statistics | ||
|---|---|---|---|---|---|---|---|
| r | P-Value | β | SE | β | VIF | ||
| Number of high-risk family members | -0.162 | 0.053 | -0.057 | 0.28 | -0.040 | 0.048 | 1.07 |
| DSMQ-blood glucose management | 0.823 | < 0.001 | 0.348 | 0.019 | 0.459 | < 0.001 | 1.59 |
| DSMQ-control of regimen | 0.764 | < 0.001 | 0.231 | 0.018 | 0.321 | < 0.001 | 1.70 |
| DSMQ-physical activity | 0.602 | < 0.001 | 0.162 | 0.016 | 0.232 | < 0.001 | 1.40 |
| DSMQ- health care use | 0.616 | < 0.001 | 0.189 | 0.020 | 0.213 | < 0.001 | 1.35 |
| COVID-19-related psychological distress | -0.013 | 0.448 | 0.008 | 0.003 | 0.056 | 0.009 | 1.18 |
| Diabetes distress (regimen distress) | -0.659 | < 0.001 | -0.208 | 0.049 | -0.132 | < 0.001 | 2.60 |
| Diabetes distress (interpersonal distress) | -0.354 | < 0.001 | 0.077 | 0.032 | 0.061 | 0.018 | 1.71 |
Abbreviations: DSMQ, Diabetes Self-management Questionnaire; SE, Standard Error; VIF, Variance Inflation Factor.
a Adjusted R2 = 96%; P < 0.001.
5. Discussion
Type-2 diabetes mellitus is a risk factor associated with COVID-19 (3). Self-management is the basis of diabetes care, and its adherence during the COVID-19 pandemic has great importance (6). This study investigated the factors related to diabetes self-management during the COVID-19 pandemic.
5.1. Personal Factors
Our results showed that people with more infections with COVID-19 or hospitalizations due to the disease had less participation in activities related to their dietary control. Different self-management activities form people's daily routines (24). Getting infected with COVID-19 imposes lifestyle changes on lives and alters one's routine activities (25, 26), which may be challenging for DSM. In contrast, this study revealed that people who received more doses of the COVID-19 vaccine were more likely to participate in physical activity and health care use. They also reported fewer hospitalizations among their family members and scored lower on diabetes distress and depression. Social distancing following the outbreak of COVID-19 causes barriers to optimal self-management as it limits one's participation in outdoor physical activities and access to adequate food, medicine, and glycemic control equipment. The condition also resulted in people having fewer visits with their family, health care providers, and peers, hence receiving less support from them (10, 12, 27). COVID-19 vaccination may reduce isolation and improve participation in social activities, including diabetes management. On the other hand, due to the negative relationships between psychological symptoms and DSM activities (28-30), COVID-19 vaccination may improve self-management by reducing diabetes distress and depressive symptoms.
5.2. Familial Factors
According to our results, COVID-19 infection or hospitalization in one's family member was associated with less involvement in various self-management activities, especially adhering to a healthy diet. Also, having fewer high-risk family members was of the factors predicting more desirable self-management. As people live in their family and social environment, the family and their routines are considered an influencing factor for DSM (31, 32). Having a family involved with COVID-19 may change the family routines and sources of family support and impose barriers to self-management. Also, as the findings of this study support, one's family hospitalization due to COVID-19 was associated with diabetes distress and depressive symptoms, compromising DSM (28-30). Consistent with our findings, previous research has confirmed the association between having high-risk family members and anxiety, stress, and depression in people with diabetes in the COVID-19 pandemic (33).
5.3. Psychological Factors
The present study showed that the increase in various aspects of diabetes distress and depressive symptoms were associated with poorer DSM behaviors. In line with our results, previous research also identified anxiety and stress as barriers to optimal management of diabetes during the COVID-19 pandemic (27). Participation in self-management activities, developing a healthy lifestyle, and receiving social support from family, health professionals, and peers can reduce diabetes distress and depressive symptoms (29, 30). The prevalence of COVID-19 has limited people's social support sources and affected their outdoor physical activity and their access to the materials and equipment required for DSM (10, 12, 27). These may negatively affect self-management and, consequently, the psychological health of people with diabetes. The present study also showed that in addition to diabetes distress and depressive symptoms, COVID-19-related psychological distress could predict DSM behaviors. Furthermore, the COVID-19-related fear, anxiety, and distress were associated with some aspects of diabetes distress and depressive symptoms. Previous studies have shown that diabetes distress and depressive symptoms have a stronger negative effect on DSM and thus glycemic control by reinforcing each other (34, 35). Our study suggests that different psychological factors in the COVID-19 pandemic may overlap and challenge the optimal self-management of people with diabetes. Future research could provide further investigation in this area.
5.4. Strengths and Limitations
This study was one of the pioneers in investigating the relationship between DSM and COVID-19-related personal, familial, and psychological factors. Despite weak correlations between the study variables, the findings can expand the body of existing evidence and help conduct future research on a larger sample of people with diabetes. The generalizability of the findings was also limited due to the selection of the study participants from one geographical area.
5.5. Conclusions
People with diabetes can improve their participation in diabetes self-management activities by taking care of themselves and their families against COVID-19 and controlling negative emotions. COVID-19 vaccination can reduce one's diabetes distress and depressive symptoms and lead to more desirable self-management behaviors.

.png)