1. Background
The birth of a preterm infant makes parents develop stress. According to the World Health Organization (WHO), a preterm infant is one born before 37 weeks from the first day of the last menstrual period (1). The WHO estimates that the global preterm birth rate was 10.6% in 2014 (2) and 4.8% in Iran (3). Prematurity is the leading cause of death and morbidity in infants worldwide. Preterm infants need hospitalization due to their problems, and sometimes they must be hospitalized in the neonatal intensive care unit (NICU) for a long time (4).
Hospitalization in the NICU is a bitter and stressful experience for parents (5). Stress from the equipment in the NICU, the presence of a vulnerable baby, and lack of knowledge about the baby’s condition can cause parental stress and feelings of helplessness (6). These parents often experience psychological reactions, such as hopelessness, confusion, separation, guilt, sadness, depression, hostility, irritability, fear, anxiety, grief, helplessness, failure, etc. (7).
Resilience is a positive psychological approach to coping with stressors throughout life. Resilience refers to how a person can improve their social functioning and overcome problems despite exposure to life pressures and risk factors (8). Resilience is characterized by strengths and abilities, optimism, flexibility, and altruism. Thus, interventions that aim to affect cognitive processes and improve these processes can play an important role in developing skills and abilities related to resilience components (9). Resilient family members have fewer symptoms of depression and acute stress. Highly resilient families are more satisfied with the care provided by the care team. Moreover, the implementation of interventions aimed at increasing resilience can improve the experiences of family members of patients admitted to the ICU (9). Implementing educational, supportive family interventions is effective in psychosocial adjustment and treatment acceptance in families. Accordingly, nurses, as professional health therapists, play a vital role in meeting educational needs, increasing empowerment, creating a sense of power in parents, and providing psychological, emotional, and social support for them (6).
In this regard, studies have shown that educational interventions reduce the anxiety, depression, and long-term stress of parents and increase their satisfaction, knowledge, and skills (10, 11). These studies have also shown that implementing educational programs empowered not only parents but also had positive psychological effects.
One way to provide education to parents is to use virtual learning. Virtual learning can facilitate instructions on health issues, raise public awareness, and provide easier access to the information needed by people at any time and place (4). Since there is a huge bulk of specialized materials on infant care, virtual learning can be used to improve care plans and skills (4). Nourani et al. showed that using a smart mobile application can satisfactorily improve the educational needs of mothers of premature infants (12). Kadivar et al. reported a positive impact of internet-based education and the satisfaction of mothers of preterm infants with this educational technique (6). Moreover, Garfield et al. found that a mobile phone training program increased the self-efficacy of parents of low-birth-weight children at the time of discharge (13).
2. Objectives
The presence and participation of parents in the care of preterm infants may improve parents’ resilience and care of infants. Also, the developmental status of preterm infants can be improved regarding the mothers’ participation in the neonatal care department. Based on previous studies, virtual learning might have a positive impact on the quality of care and satisfaction of mothers of preterm infants. Accordingly, this study aimed to determine the effect of virtual-learning supportive interventions on the resilience of mothers of premature infants admitted to NICUs in 2020.
3. Methods
3.1. Research Design
This quantitative quasi-experimental study was conducted on 2 groups with 2 pre- and post-intervention phases conducted from spring to the end of summer 2020 in the NICU of Afzalipour Hospital in Kerman, Iran. Afzalipour Hospital has 96 beds in the NICU and is equipped with all the facilities needed to care for premature infants. The hospital is the largest neonatal educational and medical center in southeastern Iran.
3.2. Sampling
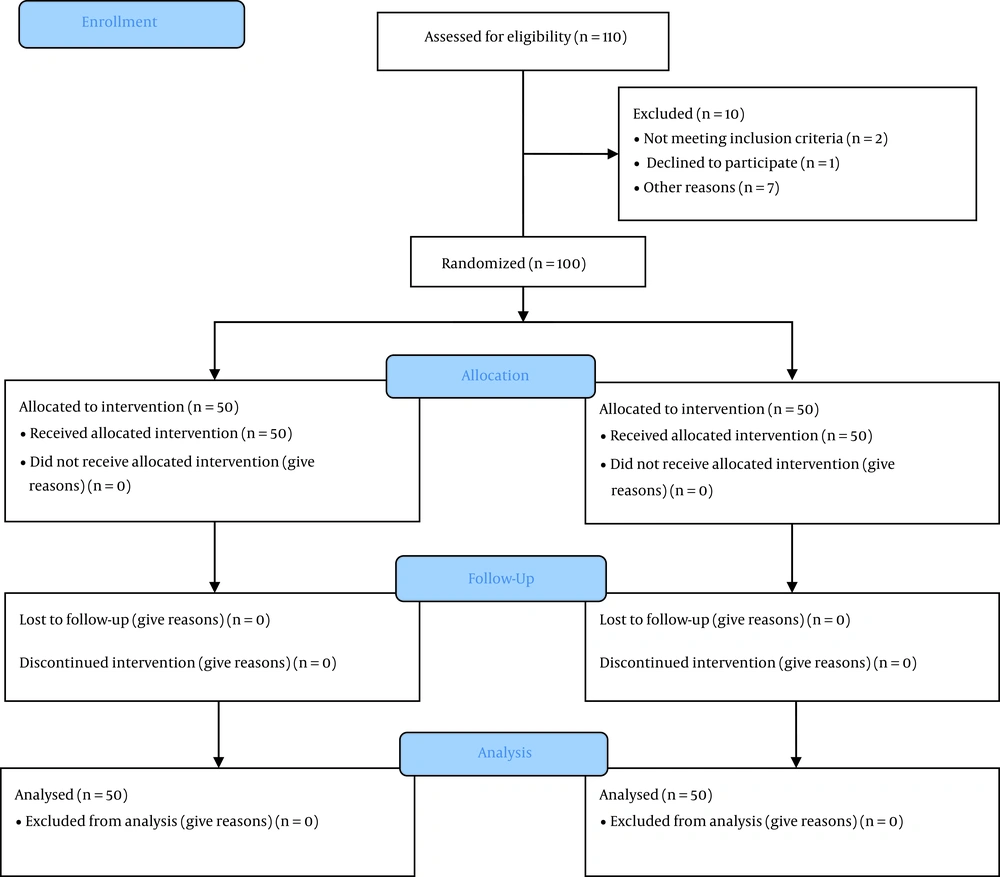
Following a similar study (14) and considering 80% power and 95% CI, the sample size was estimated as 28 persons using the Pokak formula using G*Power version 3.1.9.7. However, due to the likelihood of dropping out of the study, as well as to enhance the power of the study, 50 people were placed in each group (100 persons in total). The sampling procedure for the 2 groups lasted about 6 months. All participants completed the study. Inclusion criteria were infants aged 30 - 36 weeks, willingness to participate in the study, no history of another premature infant care, and having hemodynamic stability (heart rate: 120 - 160, respiratory rate: 40 - 60, O2 saturation 85% - 95% with infants having pink color), a minimum level of literacy for the mother, and the absence of any (self-reported) mood and emotional disorder in the mother that could prevent effective communication. The exclusion criteria were the death or change in the infant’s physiological condition (15).
The sampling procedure was done by one of the researchers (the first author) before starting the intervention. Firstly, a list of mothers of infants admitted to the NICU who met the inclusion criteria was prepared, and the mothers were allocated into 2 control and intervention groups using a random number table. Second, informed consent was obtained, and the objectives of the study were explained to the participants. Finally, 2 groups of the study completed the 2 instruments (the demographic information questionnaire and Connor-Davidson Resilience Scale (CD-RISC)) before the intervention.
3.3. Intervention
In the first face-to-face session, mothers in the intervention group who were familiar with the researcher attended a virtual learning program using an application called “Ghoncheha” (buds or preterm infants) that could be installed on the Android mobile operating system and received family-centered care training. The application was installed on the mothers’ mobile phones with the help of the researcher in the waiting room of the NICU. In this session, the mothers also learned how to install and use the application.
The application contained 2 sections. The first section contained some information to increase the awareness and knowledge of the mothers of preterm infants, and the other section was designed to support them psychologically. The first section of the application consisted of 6 parts: (1) information about the NICU and its equipment; (2) information about premature infants (neonatal period, neonatal classification, preterm infant characteristics, causes of preterm infant birth, and premature infant problems); (3) premature infant nutrition (nutritional tips for premature infants, nutritional differences in premature infants, breast milk and premature infants, stages of preterm infant feeding, stimulation of premature infants to get the nipple, preterm infant breastfeeding conditions, nipple protection, and benefits of finger feeding); (4) developmental care (5 senses of the infant and the environment, preterm infant positioning, and premature infant sleep and wake states); (5) kangaroo care (definition and benefits of kangaroo care, mother and baby position during kangaroo care, and kangaroo care at home); and (6) post-discharge care (monitoring the growth and development of the preterm infant, feeding the preterm infant after discharge, nutritional supplements, vaccinations, danger signs in the preterm infant, various screening tests for the premature infant, infection, jaundice, gastroesophageal reflux disease, and neonatal colic (Table 1).
| Session | Description |
|---|---|
| 1 | Definition of NICU and its equipment, including incubators, warmers, monitors, and ventilators |
| 2 | Information about the newborn period, classification of newborns, preterm infants, characteristics of preterm infants, causes of preterm birth, problems of preterm infants, visits to the NICU, and hand hygiene |
| 3 | Information about the principles of feeding a preterm infant, the differences between a preterm infant in feeding, breast milk and a preterm infant, stages of feeding a preterm infant, stimulation to take the breast and how the baby takes the breast, the correct position of the infant, precautions while breastfeeding the infant, important points of nutrition in a preterm infant, breastfeeding positions of a preterm infant, the importance of breastfeeding position, nipple protector, tips and method of using nipple protector, tips for squeezing the breast and benefits of squeezing the breast, non-food sucking and finger feeding, and benefits of finger feeding |
| 4 | Information about developmental care, the 5 senses of the infant and the environment, the sense of sight and the effects of light in the preterm infant, the objects in the vision range of the preterm infant, the sense of hearing and the effects of noise in the preterm infant, the care of the hearing of the preterm infant, the care of taste, smell, and touch senses of a preterm infant, the positioning of a preterm infant, the complications and advantages of positioning an infant, the principles of moving a preterm infant, the method of lifting a preterm infant, the sleeping and waking position of a preterm infant, the benefits of sleep in an infant and the effects of sleep deprivation, infant sleep support, bathing a preterm infant in the NICU and how to bathe preterm infant, and change an infant’s diaper |
| 5 | Information about KMC and its benefits, the condition of the infant and mother in KMC, feeding the baby in KMC, covering the baby in KMC, KMC at home, benefits and tips of KMC at home |
| 6 | Information about following up the growth and development of a preterm infant, feeding a preterm infant after discharge, nutritional supplements, vaccinations, danger signs in a preterm infant, screening, hearing examination of a preterm infant, retinopathy of prematurity, hypothyroidism, phenylketonuria and fauvism, congenital dislocation hip, brain ultrasound, premature osteopenia, infection, jaundice, gastroesophageal reflux, and infantile colic |
| 7 | To provide psychological support to other parents of preterm infants, the photos and characteristics of grown-up preterm infants and the stories of mothers of preterm infants were presented. |
| 8 | Educational videos regarding the importance of breastfeeding for preterm infants, finger feeding, and cup feeding |
The Contents of the Training Program
This section is according to recent studies on neonatal intensive care nursing and related topics. The second section of the application contained some instructions on transferring experiences during the infants’ hospitalization. This section describes the experiences of mothers of premature infants and the strategies used by them to gain comfort during their child’s admission to the NICU. It also contained the data from the interviews with the mothers of infants who had previously improved and a review of the literature. The length of electronic instructions was about 120 minutes. This application was developed by the members of the research team using programming software, and the validity of the instructional content of the electronic file was confirmed by 2 experts holding a PhD in neonatal intensive care nursing and a neonatal fellowship degree from the Department of Newborn and Neonatal Care of the School of Dentistry (Figure 1).
The mothers were asked to read the instructions in the application during the day whenever they felt physically and mentally good. Also, the researcher created a WhatsApp group, and the mothers in the intervention group joined the group to receive education supplementary to the e-learning content. The instructional content of the application was uploaded to the group for mothers to review the instructions. The mothers could ask any possible questions from 7 AM to 7 PM, and a researcher, who was a final-year Master’s student of neonatal intensive care, answered their questions. The mothers could interact with each other and the researcher in the group. The researcher monitored their interactions to prevent exchanging incorrect instructions and false information with the group members. The mothers could also talk to each other about their psychological conditions, worries, and stress. The intervention in the intervention group lasted for 2 weeks. One month after the intervention, the participants completed the CD-RISC.
To ensure that participants in the 2 groups did not communicate and did not exchange information, the members in the 2 groups were selected from separate work shifts. All participants were unaware of how each group member was assigned. For example, if the participants in the intervention group were sampled on Saturday morning, the members of the control group were selected in other shifts on Saturday. In addition, the application was installed on the phones of the participants in the intervention group in a separate room where the members of the control group were not present, and the researcher asked them not to install it on other people’s phones (16).
3.4. The Control Group
The control group received routine care and training in an unorganized manner by NICU nurses. One month after the intervention, the participants completed the CD-RISC. To comply with ethical considerations, the mobile application was given to the members of the control group at the end of the study, and they could also ask questions about the application for 2 weeks in a WhatsApp group.
3.5. Instruments
Demographic data were collected using a demographic questionnaire assessing the maternal age, age of marriage, education, place of residence, mother’s job, neonatal sex and age, birth weight, type of nutrition, type of delivery, and satisfaction with the neonatal sex. Moreover, CD-RISC was used to measure the participants’ level of resilience before and after the intervention. The scale was developed by Connor and Davidson in 2003 based on a review of the literature from 1979 to 1991. The scale contains 25 items scored on a 5-point Likert scale ranging from not true at all (0) to true nearly all the time (4). The minimum and maximum resilience scores for a respondent are 0 and 100, respectively. The results of exploratory factor analysis confirmed the existence of 5 factors: Personal competence, high standards, and tenacity; trust in one’s instincts, tolerance of negative affect, and strengthening effects of stress; positive acceptance of change and secure relationships; control; and spiritual influences. Higher scores on this scale indicate that a person will be able to cope more effectively with adverse or complex events in their life (8). The validity of this scale was confirmed by estimating its content validity and convergent and divergent validity in different (normal and at-risk) groups (17). The validity of this tool was confirmed in Iran by Mohammadi, with a Cronbach α of 0.89 for the total scale (18). In the study by Jamali et al., the Cronbach α coefficient was 0.87 for the reliability of the scale (8). Besharat confirmed the validity and reliability of the scale (19). Ranjbar Hagh et al. assessed the reliability of the scale using the Cronbach α coefficient; the corresponding value was reported to be 0.84, confirming the acceptable reliability of the scale (20).
3.6. Data Analysis
The collected data were analyzed using SPSS version 22 (SPSS Inc, Chicago, Ill, USA). Descriptive statistics (frequency, percentage, mean, and SD) were used to describe the demographic characteristics of the participants. Moreover, chi-square and Fisher exact tests were used to compare the intervention and control groups in terms of demographic variables. Based on the Kolmogorov-Smirnov test, an independent samples t-test was used to compare the scores of resilience and resilience dimensions between the 2 groups before and after the intervention. Moreover, a paired samples t test was used to compare the resilience scores in each group before and after the intervention. The significance level was set at P < 0.05.
3.7. Ethical Considerations
This study was approved by the Ethics Committee of Kerman University of Medical Sciences (code: IR.KMU.REC.1399.192). The researcher also obtained an introduction letter from the Office of Postgraduate Studies of the Faculty of Nursing and presented it to the officials of the NICU. The participants entered the study with full knowledge and with their written consent. The participants were reassured that their identities and information would be kept confidential.
4. Results
The majority of participants in both groups were 25 to 35 years old and had been married for 18 to 35 years. Fifty percent of mothers in the intervention group had an undergraduate or postgraduate degree, and 42% in the control group had an associate degree or high school diploma. There were no significant differences between the 2 groups in terms of demographic characteristics (Tables 2 and 3).
| Groups | Intervention (n = 50) | Control (n = 50) | Test Results |
|---|---|---|---|
| Demographic Variables | |||
| Mother’s age | 24.65 ± 4.667 | 23.89 ± 4.23 | t = 0.043 b; P = 0.892 |
| Marriage age | t = 0.56; P = 0.78 b | ||
| < 18 | |||
| 18 - 35 | 22.32 ± 2.34 | 23.13± 3.45 | |
| > 35 | |||
| Qualitative Variables | |||
| Level of education | χ2c = 0.89; P = 0.19 | ||
| High school | 4 (8) | 10 (20) | |
| Diploma and post-diploma | 21 (42) | 21 (42) | |
| Bachelor’s degree and higher | 25 (50) | 19 (38) | |
| Address | χ2d = 0.66; P = 0.29 | ||
| City | 44 (88) | 46 (92) | |
| Village | 6 (12) | 4 (8) | |
| Mother’s job | χ2c = 0.98; P = 0.10 | ||
| Employed in government offices | 5 (10) | 4 (8) | |
| Employed in the private sector | 2 (4) | 2 (4) | |
| Housewife | 43 (86) | 44 (88) | |
| Type of delivery | χ2d = 0.29; P = 0.93 | ||
| Normal vaginal delivery | 11 (22) | 13 (26) | |
| Cesarean section | 39 (78) | 37 (74) | |
| Satisfaction of the baby | χ2c = 0.54; P = 0.99 | ||
| Satisfied | 49 (89) | 50 (100) | |
| Unsatisfied | 0 | 0 | |
| No idea | 1 (2) | 0 | |
Frequency Distribution and Percentage of Demographic Variables of Mothers of Hospitalized Preterm Infants (n = 100) a
| Demographic Variables | Intervention (n = 50) | Control (n = 50) | Test Results |
|---|---|---|---|
| Gender of the baby | χ2b = 0.040; P = 0.841 | ||
| Boy | 25 (50) | 24 (48) | |
| Girl | 25 (50) | 26 (52) | |
| Baby age | χ2c = 0.756; P = 0.385 | ||
| Under a week | 17 (34) | 14 (28) | |
| 1 - 2 weeks | 22 (44) | 21 (42) | |
| 2 weeks to 1 month | 8 (16) | 12 (24) | |
| Over a month | 3 (6) | 3 (6) | |
| Birth weight of the baby | χ2c = 0.002; P = 0.964 | ||
| Under 1500 g | 15 (30) | 14 (28) | |
| 1500 - 2500 g | 31 (62) | 33 (66) | |
| Above 2500 g | 4 (8) | 3 (6) | |
| Type of nutrition | χ2c = 57.98; P = 0.950 | ||
| Breast milk | 33 (66) | 36 (72) | |
| Formula | 6 (12) | 6 (12) | |
| Breast milk and formula | 11 (22) | 8 (16) |
Frequency Distribution and Percentage of Demographic Variables of Preterm Hospitalized Neonates (n = 100) a
The mean resilience scores in the intervention group were 57.62 ± 13.95 and 76.96 ± 08.07 before and after the intervention, indicating a significant difference in their resilience before and after the intervention as confirmed by the paired samples t-test (P = 0.000). There were also significant differences between the mean scores of resilience dimensions before and after the intervention in the intervention group, as shown by the paired samples t-test (P = 0.000). In addition, the mean resilience scores in the control group were 60.40 ± 14.41 and 62.70 ± 11.09 before and after the intervention, showing no significant difference in their resilience before and after the intervention (P = 0.08). There were significant differences in the resilience dimensions, including positive acceptance of change, secure relationships, and control for the participants in the control group before and after the intervention (P = 0.000). However, there were no significant differences in the mean scores of personal competence tenacity, trust in personal instincts (P = 0.581), tolerance of negative affect (P = 0.785), and spiritual influence (P = 0.90) in the control group before and after the intervention, as shown by the paired samples t-test. The independent samples t-test also suggested no significant differences between the 2 groups in terms of resilience before the intervention (P = 0.32). However, there were significant differences between the 2 groups regarding resilience after the intervention (P = 0.000), as shown in Table 4.
| Variables | Before the Intervention | After the Intervention | Within Groups |
|---|---|---|---|
| Notion of personal competence, high standards, and tenacity | |||
| Intervention group | 5.62 ± 18.00 | 3.58 ± 23.58 | t = -8.483; P = 0.000 b |
| Control group | 5.99 ± 18.78 | 4.41 ± 18.48 | t = 0.556; P = 0.581 b |
| Between the 2 groups | t = -0.671; P = 0.50 b | t = 6.34; P = 0.000 b | |
| Trust in one’s instincts, tolerance of negative affect, and strengthening effects of stress | |||
| Intervention group | 4.60 ± 13.94 | 3.07 ± 19.02 | P = 0.000 b; t = -9.589 |
| Control | 4.33 ± 15.62 | 3.88 ± 15.48 | P = 0.785 b; t = -0.274 |
| Between the 2 groups | P = 0.0 b; t = - 1.879 | P = 0.000 b; t = 5.055 | |
| Positive acceptance of change and secure relationships | |||
| Intervention group | 3.50 ± 12.60 | 1.59 ± 17.32 | P = 0.000 b; t = -13.042 |
| Control | 3.53 ± 12.88 | 2.89 ± 14.38 | P = 0.034 b; t = -2.175 |
| Between the 2 groups | P = 0.69 b; t = 0.398 | P = 0.000 b; t = 6.282 | |
| Control | |||
| Intervention group | 2.07 ± 7.04 | 1.25 ± 10.16 | P = 0.000 b; t =10.068 |
| Control | 2.04 ± 7.14 | 1.47 ± 8.22 | P = 0.000 b; t = -4.056 |
| Between the 2 groups | P = 0.80 b; t = 0.243 | P = 0.000 b; t = 7.093 | |
| Spiritual influences | |||
| Intervention group | 1.15 ± 6.04 | 0.89 ± 6.88 | P = 0.000 b; t = -5.838 |
| Control | 1.37 ± 5.98 | 1.29 ± 6.14 | P = 0.290; t = 1.071 |
| Between the 2 groups | P = 0.81 b; t = 0.236 | P = 0.001 b; t = 3.326 | |
| Resilience | |||
| Intervention group | 13.95 ± 57.62 | 8.07 ± 76.96 | P = 0.000 b; t = 11.770 |
| Control | 14.41 ± 60.40 | 11.09 ± 62.70 | P = 0.08 b; t = 1.740 |
| Between the 2 groups | P = 0.32 b; t = -0.980 | P = 0.000 b; t = 7.352 |
Comparison of the Mean and SD Resilience Score of Mothers Between and Within the 2 Groups
5. Discussion
This study examined the effect of a virtual educational and supportive intervention on the resilience of mothers with preterm infants admitted to NICUs in 2020. The results showed a statistically significant difference between the mean resilience scores in the intervention group before and after the intervention. While the mothers in the control group did not receive any special intervention, and their tolerance scores did not change. A comparison of the resilience scores after the intervention showed a statistically significant difference between the intervention and control groups. Thus, the virtual educational and supportive intervention improved the resilience of mothers of premature infants.
In line with our results, Arani Assarpour et al. reported that psychological empowerment training could increase the resilience of mothers of premature infants admitted to the NICU (17). In their study, the supportive program included only psychological interventions, but in our study, the educational and psychological needs of mothers were also considered in the intervention program.
Further, Naderi et al. also showed that supportive interventions for the resilience and quality of life of family caregivers with advanced heart failure increased the resilience of caregivers (21). In their study, family caregivers confronted many problems in the care of heart failure patients for a long time, and in our study, most of the mothers suffered acute mental problems due to the unexpected birth of their children.
Perhaps the passage of time can improve the resilience of caregivers, which was not the aim of the present study. In our study, the intervention program was conducted for 2 weeks, indicating that more studies should be conducted for longer periods.
One of the effective factors in raising the level of resilience is spiritual/religious beliefs. Rahmati et al. found that religious and spiritual interventions can effectively improve the resilience of parents of patients admitted to the NICU (22). In the context of this study, all mothers were Muslims, and they all believed in the existence of supreme power. However, it seems that comparative studies in different societies with different beliefs can give valuable information in this regard.
Satici argued that hopefulness affects resilience (23). In line with these findings, it can be argued that supportive educational interventions can meet the educational needs of mothers, encourage them to engage in caring for the infant, and create a sense of power in them. In addition, using mobile applications (such as WhatsApp messenger) can provide a good platform for communication and exchange of experiences among mothers of premature infants and promote the social support of mothers. Thus, implementing virtual support interventions can improve maternal resilience. However, the studies reviewed above were different from the current study in terms of teaching methods. The interventions in the reviewed studies were conducted in person, while the supportive intervention in the present study was through distance education.
In line with the results of the present study, Nourani et al. showed that using smart mobile apps can satisfactorily meet the educational needs of premature infants admitted to teaching hospitals in Tehran (12). This study focused only on meeting the educational needs of mothers. However, the present study addressed the mental and educational needs of mothers of premature infants. Nourani et al. also assessed mothers’ satisfaction (12). Maternal satisfaction can improve the mental state and thus improve the quality of maternal care for the infant.
Similar to the findings of the current study, Jafarzadeh et al. highlighted the positive effect of distance nursing on increasing attachment and reducing stress in mothers with premature infants (24). Also, Jalali et al. showed that virtual education were so effective in developmental care in nurses of neonatal intensive care units (4).
According to the results of the current study, some studies indicated that distance nursing support promoted maternal attachment and reduced maternal stress. For example, Kadivar et al. reported the positive effect of internet-based education on the satisfaction of mothers with premature infants (6). The training intervention in their study was provided based on the internet, while in our study, the training program was implemented through a mobile application. Also, Garfield et al. examined the support for parents of premature infants transferred from the NICU to home with a mobile app at the US Children’s Hospital and showed that parental self-efficacy increased at discharge (13). They aimed to assess the effect of the intervention on parents’ readiness for discharge, while we addressed mothers’ resilience.
Tang et al. also developed a mobile app called Estrellita to support caregivers of premature infants, including parents and nurses, at a southern California hospital (25). The results showed that parents’ stress levels were reduced, and their self-esteem improved (25). Ra and Lim developed and evaluated a video education program focusing on mother-infant interaction for mothers of preterm infants admitted to the NICU (26). The program contained educational scenarios and videos. The results showed that the content designed for mother-infant interaction was effective in reducing stress and increasing mothers’ self-confidence (26).
Implementing virtual supportive interventions, like other virtual training, makes it easier for mothers of preterm infants to access the information they need at any time and place, thereby increasing their awareness and improving their functions and caring skills. Thus, implementing virtual supportive interventions can positively affect mothers’ resilience. Implementing support programs with a focus on various educational, empowerment, and psychological aspects of parents of premature infants is an inevitable necessity. In fact, with the admission of the infant to the NICU, the parents enter an unfamiliar and complicated situation, and, instead of having a healthy infant, they have a premature baby who has to undergo intensive care and aggressive procedures and be surrounded by technology to meet their needs. These conditions do not allow the parents to help the infant; thus, they feel so stressed by the lack of control over the situation and separation from the infant. These tensions and stresses reduce mothers’ resilience and put their mental health at risk (27, 28). Moreover, the anxiety and stress of infant admission can cause parents not to receive and process educational information properly (6).
Since resilience is not a stable trait, people can have higher or lower levels of resilience because people’s resources change over time. Resilience is a non-inherent and learnable trait that can be enhanced by education and experience (29). One of the effective measures to improve the mental condition of mothers is to educate and support them to create positive outcomes and improve mothers’ resilience. Accordingly, the virtual supportive intervention enabled mothers to receive care information about their infants as soon as possible. The program also helped the mothers meet their emotional needs, reduce their anxiety and stress, and improve their resilience.
5.1. Conclusions
Resilience and all its dimensions improved more in the intervention group than in the control group. The virtual supportive intervention provided psychological support to parents and improved their awareness. Thus, this intervention led parents to effectively deal with the stressful conditions of the infant’s hospitalization and thus promoted parental resilience. Accordingly, supportive educational interventions can be provided using mobile applications for parents of hospitalized infants. These interventions can provide psychological support to parents, meet their needs for information about the premature infant’s conditions, and help them to engage in caring for the infant.
5.2. Limitations
This study had some limitations that need to be addressed. A self-report questionnaire was administered to measure the effectiveness of a virtual educational and supportive intervention in the resilience of mothers of preterm infants. The assessment of the resilience of mothers of preterm infants might be affected by the participants’ bias inherent in the self-report questionnaire. In other words, since mothers of preterm infants might tend to overrate their levels of psychological situation, the data might not reflect the actual level of mothers of preterm infants’ resilience. Thus, to determine the actual level of resilience among these mothers, future research might include objective rather than self-reported measures of resilience, as well as mixed methods of competency evaluation. Further, data analysis was performed 1 month after the intervention; accordingly, more studies are needed with longer follow-ups (3 - 6) to obtain more accurate findings, determine the long-term influence of these interventions, and evaluate their impact on the mothers. Another limitation of the research is that the subjects were selected from only 1 medical center; thus, the results could not be generalized to the general population.