1. Background
Adequate nutrition is an essential determinant of health in the elderly. Normal deglutition, as the first phase of digestion, is one of the most complicated neuromuscular processes of the central nervous system that allows the easy and safe transfer of foods and liquids from the mouth to the stomach. This process occurs in four stages: preparatory, transport, pharyngeal, and esophageal stages (1). Swallowing disorder or dysphagia occurs when this normal process is disrupted, and the person cannot move food from the mouth to the stomach. Swallowing disorders can occur throughout a person's life, but they're more common in old age (2). The true prevalence of dysphagia in the elderly is very different and is often underestimated because of the aging associated with various neurological and metabolic diseases. But the prevalence of dysphagia in the elderly with no specific disease and as a natural result of aging is 37.6% among the elderly population (3-5).
Age-related changes in the swallowing mechanism, along with age-related diseases, put older individuals at a higher risk of developing dysphagia (6).
Complications of Dysphagia in the elderly as a result of undiagnosed and untreated include may cause Aspiration resulting in chest infection or pneumonia, malnutrition or insufficient nutrition, unexpected weight loss, dehydration, reduced muscle strength, and an increased risk of death in older people (7). Because eating is an important social activity, dysphagia has a negative impact on self-esteem, social role functioning, social isolation, depression, and quality of life (8).
Deglutition problems in the elderly who have no overt disease are mostly due to age-associated loss of muscle mass and strength (Sarcopenia) and frailty. Sarcopenia and frailty are the consequences of normal aging. As regards the muscles involved in swallowing, such as the tongue, pharyngeal muscles, and suprahyoid muscles, are skeletal muscles; the decrease in muscle mass affects the function and strength of these muscles (9-11). For example, the study by Metheny has indicated that the risk of Aspiration increases due to sarcopenia, which reduces tongue propulsion (12). Also, some studies have demonstrated that older people have a reduction in laryngeal elevation, rotation, and forward movements which can delay airway closure and poor cough in the elderly (13-15).
Therapeutic techniques provided by speech therapists include the use of compensatory strategies (change of diet, change of position) and rehabilitative exercises (muscle strengthening exercises or swallowing maneuvers) (1). Because the muscles used for swallowing can become weaker with age, in recent years, some studies have surveyed the effects of muscle strengthening exercises as the most common rehabilitative exercises for dysphagia therapy in the elderly (15-17). Robbins et al. studied the Effects of Lingual Exercise on swallowing in ten older adults, and the results indicated significantly increased isometric and swallowing pressures (18). In another study, Balou et al. (19) investigated the effect of effortful swallows, Mendelsohn maneuvers, tongue-hold swallows, supraglottic swallows, Shaker exercises, and effortful pitch glides on swallowing function in nine healthy older adults, and the results of their study indicated which significant improvements in swallowing physiology. In a randomized pilot study, Park et al. surveyed the effect of chin tuck against resistance (CTAR) exercise on patients with dysphagia following stroke. This study demonstrated that CTAR effectively improves pharyngeal swallowing function in patients with dysphagia after stroke (20). Despite the positive effects of these exercises on swallowing function, Wakabayashi and his colleagues investigated the effects of tongue resistance exercise and a head flexion exercise against manual resistance on dysphagia; the results of their study indicated resistance training of swallowing muscles did not improve dysphagia (21). Thus, there is a controversy about muscle training methods for dysphagia, the physiologic mechanisms of these exercises are debated, and there is little supporting data available. Also, most studies have been related to specific muscle groups, such as the suprahyoid in the Shaker exercise or tongue strengthening exercise in stroke patients. The swallowing process is a sequential process that begins from mouth to stomach.in this sequential process, more than 30 pairs of muscles are involved, which coordinately move food from the mouth to the stomach.
2. Objectives
In this study, our aim is to investigate the effect of strengthening exercises of these muscles on the clinical function of swallowing and the quality of life of the elderly.
3. Methods
3.1. Trial Design
This study was a pilot randomized clinical trial, registered in www.irct.ir, Reference Number: IRCT20130725014161N2, and approved by the ethics committee of Semnan University of Medical Sciences (reference code: IR.SEMUMS.REC.1397.139). All participants in this study were informed about dysphagia and its complications, and the role of swallowing rehabilitation in preventing these complications was explained.
3.2. Participants
A total of 253 community-dwelling older adults (between June 2018 and February 2019) who attended a healthcare center to receive routine elderly medical care were interviewed to assess eligibility to participate in this clinical study. Demographic characteristics, including gender, age, and other health conditions, were obtained through structured interviews and based on personal health information files in the health care center.
Inclusion criteria include age range between 65 and 80 years old, no history of neurological or general disorders that could influence swallowing function, pneumonia or head and neck surgery and radiotherapy and tobacco usage, presence of signs and symptoms of oropharyngeal dysphagia, and at least being able to read and write.
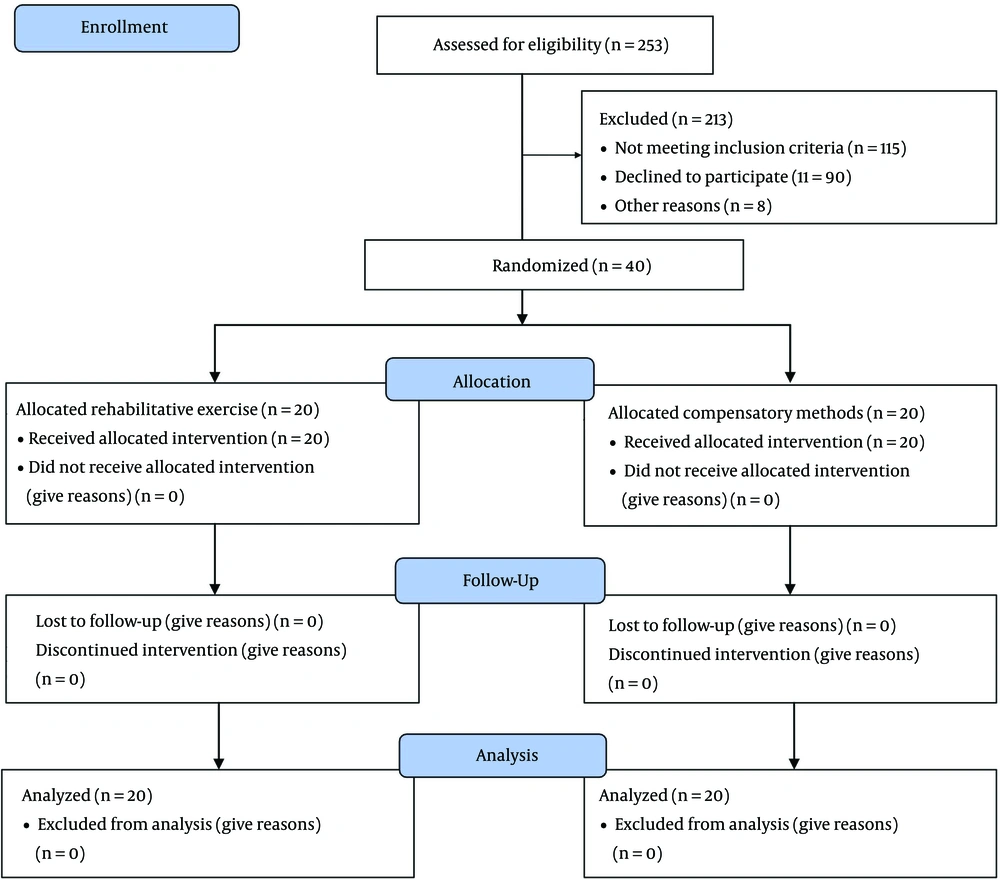
Participants would be excluded if any illness or problem with possible effects on swallowing function occurred during the study and the participants refused to cooperate. Out of 253 elderlies, 98 had oropharyngeal dysphagia, and only 40 were eligible for this study (Figure 1).
3.3. Randomization
Randomization and allocation concealment was undertaken using a block randomization technique. Two groups were defined: (1) rehabilitative exercises (n = 20); and (2) compensatory methods (n = 20). The elderly persons who visited on even days were allocated to group 1, and the elderly persons who visited on odd days were allocated to group 2. This study was single-blind because all participants included in this study were unaware of their allocation into intervention groups, but the speech therapists who treated the participants were aware of the group. Also, a therapist who was unaware of the allocation process administered the pre- and post-evaluations.
3.4. Intervention
3.4.1. The Experimental Group
In each treatment session, rehabilitation exercises for all three muscle groups were performed for 30 minutes by a speech therapist. The therapist performed the exercises five times per week for four consecutive weeks. The total number of therapeutic sessions was 20.
3.4.1.1. Tongue-Strengthening Exercises
The tongue muscles are divided into two groups, each comprising four muscles. They are classified as intrinsic muscles (superior longitudinal, inferior longitudinal transverse, and vertical muscles) and extrinsic muscles (palatoglossus muscles). The participants were asked to stick out their tongues as far as possible, hold them for five seconds, relax, and repeat the exercise five times. The other exercise applied to this group of muscles was pushing his/her tongue against the back of a spoon or a tongue depressor, holding for five seconds, relaxing, and repeating five times. Elevate the tongue inside the mouth, press the hard palate, hold for 5 seconds, and relax and repeat five times.
3.4.1.2. Perioral Muscles Strengthening Exercises
These muscles include risorius, zygomaticus major; orbicularis oris; levator labii superioris; depressor labii inferiors, mentalis; levator anguli oris; depressor anguli oris, buccinators; masseter, temporalis muscles. Elderly persons were asked to follow the therapist's command; for example, elderly persons were asked to smile, and therapists applied rehabilitation to the corners of the mouth medially and slightly downward (caudally); this exercise was used for risorius and zygomaticus major muscles.
3.4.1.3. Chin Tuck Against Rehabilitative (CTAR)
The aim of this exercise is to strengthen the infrahyoid (those that insert inferiorly include the sternohyoid, omohyoid, and sternothyroid muscles) and suprahyoid (those inserted superiorly on the hyoid bone include the geniohyoid, mylohyoid, hyoglossus, stylohyoid, and digastric muscles). In order to do this exercise, the participant is asked to sit on a chair and place a ball under her/his chin, then tuck the chin to compress an inflatable rubber ball (diameter: 30.00 cm) as far as possible. This action was repeated 30 times, regarded as a set of actions. Each patient must perform three sets of actions in the morning, afternoon, and evening.
Two speech therapists (S.S and A.T) did all these exercises with two years of swallowing rehabilitation experience.
3.4.2. The Control Group
The Control group received compensatory methods and precautions for safe swallowing, including a change of head positioning and a slowed rate of feeding by the speech therapist. After the initial evaluation and receiving recommendations and exercises related to safe swallowing, this group visited the clinic twice for secondary and final evaluation, and their swallowing function was evaluated.
3.5. Instruments
3.5.1. Mann Assessment of Swallowing Ability (MASA)
The mann assessment of swallowing ability (MASA) is an instrument designed for bedside evaluations of patients referred for swallowing function assessment. The MASA consists of 24 items. The total scores obtained from this test are 200, and its cut-off point is 177; its sensitivity (71%) and specificity (72%) were identified. A score above 178 is interpreted as normal swallowing, 168 - 177 as mild dysphagia, 139–167 as moderate dysphagia, and less than 138 as severe dysphagia (22, 23).
3.5.2. Persian Version of the Dysphagia Handicap Index (DHI)
This is a 25-item self-report tool that was used to evaluate the effect of swallowing disorders on patients' quality of life. This tool has nine questions in the functional subscale, nine in the physical subscale, and seven in the emotional subscale. There are three choices for each item, never (zero), sometimes (two), and always (four), respectively, making the range of the total DHI score 0 - 100. The Iranian version of this questionnaire has good validity, and the test-retest reliability for the total and three subscales ranges between 0.95 and 0.98 (24).
3.6. Statistical Method
Statistical analysis of data was done with SPSS software for windows (version 19.0, SPSS Inc., Chicago, IL, USA). Two-sample Kolmogorov-Smirnov test was used to evaluate the normal distribution, and the scores of the two groups on different tests were compared with the independent samples t-test and paired sample t-test. Chi-square and Mann-Whitney tests were applied to analyze ordinal variables. P-value ≤ 0.05 was considered to be statistically significant.
4. Results
Statistical analysis showed that the two groups did not have significant differences in age, gender, swallowing function, and quality of life, related to swallowing function before the intervention (P > 0.05) (Tables 1 and 2).
| Characteristics | Control Group (n = 20) | Experimental Group (n = 20) | P-Value |
|---|---|---|---|
| Age; mean ± SD | 74.5 ± 4.97 | 73.2 ± 4.97 | 0.695 |
| Gender; No. (%) | 0.429 | ||
| Male | 8 (40) | 11 (55) | |
| Female | 12 (60) | 9 (45) |
| Scores | Experimental Group (n = 20) | Control Group (n = 20) | P-Value |
|---|---|---|---|
| MASA | 161.35 ± 11.34 | 159.2 ± 7.34 | 0.451 |
| DHI | 44.4 ± 11.21 | 42.05 ± 10.02 | 0.459 |
Abbreviations: MASA, mann assessment of swallowing ability; DHI, dysphagia handicap index.
a Values are expressed as mean ± SD.
After the participants in both groups received the designed intervention, the experimental group who received rehabilitative exercises scored significantly higher than the others who did not. Table 3 displays details of outcome measures for swallowing function in both groups.
| Scores | Experimental Group (n = 20) | Control Group (n = 20) | P-Value |
|---|---|---|---|
| MASA | 175.80 ± 6.86 | 163.35 ± 8.001 | 0.001 |
| DHI | 14.80 ± 7.26 | 40.10 ± 7.98 | 0.001 |
Abbreviations: MASA, mann assessment of swallowing ability; DHI, dysphagia handicap index.
a Values are expressed as mean ± SD.
The other significant outcomes were a remarkable reduction in dysphagia severity and aspiration severity in terms of the MASA test (Tables 4 and 5). In the experimental group, after 20 sessions of intervention, 40% of the elders had mild dysphagia, and 60% had none of the dysphagia signs. The severity of Aspiration decreased significantly. While 60% of the experimental group reported "no aspiration" after the intervention, the control group struggled with this issue.
| Severity of Dysphagia | Experimental Group (n = 20) | Control Group (n = 20) | P-Value | ||
|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | ||
| No | - | 12 (60) | - | - | 0.001 |
| Mild | 4 (20) | 8 (40) | 3 (15) | 6 (30) | |
| Moderate | 8 (40) | - | 10 (50) | 8 (40) | |
| Severe | 8 (40) | - | 7 (35) | 6 (30) | |
a Values are expressed as No. (%).
| Severity of Aspiration | Experimental Group (n = 20) | Control Group (n = 20) | P-Value | ||
|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | ||
| No | - | 12 (60) | - | - | 0.001 |
| Mild | 6 (30) | 7 (35) | 4 (20) | 5 (25) | |
| Moderate | 8 (40) | 1 (5) | 9 (45) | 11 (55) | |
| Severe | 6 (30) | - | 7 (35) | 4 (20) | |
a Values are expressed as No. (%).
5. Discussion
This pilot randomized controlled trial showed that rehabilitative exercises through strengthening muscles positively affected clinical swallowing dysfunction and quality of life-related swallowing among older people without the overt disease. The participants in the intervention group significantly increased their swallowing function and reduced clinical signs of Aspiration after four weeks of rehabilitative exercises compared with controls. These findings align with previous studies investigating the effect of swallowing rehabilitation aimed at improving the physiology of swallowing dysfunction by strengthening muscles in older people (21, 25). A study showed that oral neuromuscular training positively affected swallowing dysfunction and significantly reduced aspiration signs among older people in intermediate care (26). However, in this study, changes in swallowing-related quality of life did not differ between groups. However, in our study, in the experimental group, the swallowing-related quality of life was better than in the control group because the quality of life is completely individual and is based on an individual's perception of various aspects of their lives in the cultural context; thus one of the reasons for this difference is related to the difference in the cultural context (Swedish versus Iranian) in the two studies. Another study found that expiratory muscle strength training had a positive effect on bilateral buccinators, the orbicularis oris muscles, and suprahyoid muscles in elderly participants; despite our study, in this study, the main outcome measures were swallowing-related muscle strength and did not assess swallowing function (27). According to Robbins et al., lingual resistance exercise programs can improve swallowing function in older individuals. Whereas in our study, we used swallowing-related muscle-strengthening exercises for swallowing function (18). In another study, Poorjavad et al. investigated the effects of a period of head lift exercise (HLE) and neuromuscular electrical stimulation (NMES) on swallowing muscles activity in healthy elderly and showed that the HLE, against the NMES, may be effective in reducing some aging effects on the suprahyoid muscles activity (28). Furthermore, Yoon et al., in a study observed chin tuck against resistance (CTAR) was effective for suprahyoid muscles, which agreed with the finding of our study (29). Despite of positive effects of muscle strengthening exercises on swallowing function in older people in previous studies, Wakabayashi et al. found resistance training of swallowing muscles has not been positive effects on dysphagia in older people; one of the reasons proposed by the researchers of this study is that participants in this study had low adherence rate to the exercises (21).
Another finding of the present study was the positive effect of swallowing rehabilitation on the quality of life in older people. Prior studies have also shown that elderly people who experience swallowing difficulties have decreased quality of life (QOL), social isolation, and depression (30, 31). Besides, because eating is a social and pleasurable activity, any change in this activity due to dysphagia will also negatively affect the person's quality of life (QOL) (32). Thus, a comprehensive swallowing evaluation, including patient-based, clinical, and objective instruments, has been recommended for the assessment of the efficacy of the intervention (33); we used a self-report tool for the evaluation of the quality of related swallowing that assesses a person's experience of having a swallowing problem.in agreement with previous studies, participants in this study were unaware of their swallowing dysfunction or often believed that their condition was untreatable (8).
Swallowing difficulty is a health concern in an aging population. Changes in swallowing physiology are common in elderly people due to reductions in muscle mass and connective tissue elasticity resulting in loss of strength. Dysphagia has a variety of complications on health status, such as the increased risk of malnutrition, dehydration, and pneumonia and negative impacts on quality of life. In order to prevent and minimize these complications, management of swallowing difficulties with proper intervention must be done by a speech therapist. There is no appropriate single strategy for all elderly patients with dysphagia. There are two main intervention strategies for the management of dysphagia includes Compensatory and rehabilitative strategies. The goals of compensatory techniques are using simple adjustments to facilitate oral intake safely, and their impacts are immediate and temporary. However, swallow rehabilitation exercises are intended to improve the physiology of swallowing. These rehabilitation exercises comprise various exercises for improving swallowing physiology. Although there is controversy about the effectiveness of oral motor exercises, some recent studies have indicated the positive effects of strengthening swallow musculatures, such as lip and tongue resistance exercises. Unlike previous studies, which only examined the effectiveness of one group of muscles in swallowing function, in this study, we investigated the effectiveness of strengthening exercises for all types of muscles involved in swallowing (oral, tongue, suprahyoid, and infrahyoid muscles) on swallowing function and the quality of life of the elderly.
5.1. Limitation and Suggestion
The methodology of this study was one of its most important limitations. In this study, we used only clinical evaluation for the assessment of swallowing function before and after interventions, and we did not have access to instrumental assessments such as fiberoptic endoscopic evaluation of swallowing (FEES) or tools for assessment of the strength of muscles. Future studies may result in different findings if they use instrumental assessments of swallowing function and the strength of muscles. Also, it's suggested that future studies examine the maintenance effects of exercises at 3- and six months post-treatment.
5.2. Conclusion
According to the present study, dysphagia during elder age was present in most of the evaluated elders, highlighting the necessity of proper intervention. Accordingly, the rehabilitative exercises on all swallowing muscles were applied, and their effectiveness compared with the compensatory methods was confirmed. Our findings support the use of rehabilitative exercises for swallowing therapy in elders.