1. Background
The coronavirus disease 2019 (COVID-19) spread around the world since 2019. This pandemic left the governments and health staff on the front line to treat and protect people (1-3). However, the medical staff’s mental health was exposed to the side effects of negative aspects of the pandemic such as confronting the patients’ problems, shortage of medicine, the repeated variations of the virus, changing the protocols, and being one the most vulnerable cases to catch the COVID-19 (2). Additionally, inadequate protection against infection, work overload, frustration, discrimination, isolation, contact with patients with negative emotions, lack of contact with the family, and fatigue caused mental health issues in this specific population (4-6). Wang et al. (6) reported that the medical staff experiences serious mental health issues. Stress, anxiety, depression, insomnia, denial, anger, and fear frequently have been reported by the studies. These mental health problems not only influence the attention, perception, and decision-making abilities of the staff. It seems essential to protect the mental health of healthcare workers and provide them with social support in order to manage the pandemic and guarantee the workers’ long-term health (6).
Although the medical staff are generally more informed about the methods of infection control, they seem to be stressed due to the higher risk of infection during prolonged contact with the patients (7). In this regard, Park et al. (8) evaluated the mental health of 187 nurses working in public medical centers during the outbreak of MERS; their results indicated mental health problems and stigma among nurses.
Moreover, Maunder et al. (9) investigated the psychological and occupational consequences of SARS epidemic among healthcare workers in 2003. The results of their study were published by nine hospitals treating SARS patients in Toronto, Canada, and four hospitals in Hamilton, Canada, without SARS treatment. Their results showed high levels of burnout, psychological stress, and PTSD. In another study by Su et al. (10), healthcare workers who worked in SARS units experienced higher levels of depression (38.5%) and insomnia (37%) compared to those who did not work in SARS units. Their study also reported strong negative emotions and inadequate coordination between the staff after the epidemic. Besides, this study emphasized that positive coping strategies and strong social and family support could protect the medical staff against acute stress.
Social support is a flexible resource for healthcare professionals to overcome the challenges associated with long-term exposure to the hospital environment. Moreover, social support can reinforce interpersonal relationships and help the staff play a more active role in patient care. Overall, the prevalence of infectious diseases has various significant psychosocial consequences for healthcare workers, depending on the type of their work and risk awareness (11). Generally, social support for healthcare workers involved with COVID-19 patients can have a significant impact on reducing anxiety and stress. In a study by Xiao et al. (12) on Chinese healthcare workers treating patients with COVID-19 in January and February 2020, the level of social support for healthcare workers was significantly associated with self-efficacy and sleep quality. Moreover, anxiety and stress were significantly reduced.
Following the global spread of COVID-19, no country has been immune to this highly contagious disease. Therefore, urgent attention is needed to understand the potential psychological and social consequences of the rapid spread of this infectious disease.
2. Objectives
Due to the spread of COVID-19 in Iran, the present study aimed to examine the correlation between medical staff mental health and perceived social support during the COVID-19 pandemic, Sistan and Baluchestan Province, 2020, Iran. Based on the purpose of the present study, the current research hypothesizes that there is a significant relationship between perceived social support and mental health.
3. Methods
3.1. Participants
This descriptive, correlational study was performed on all health, medical, and administrative personnel of hospitals involved in the treatment of COVID-19 patients in Zahedan, Khash, Mirjave, Saravan, and Iranshahr in Sistan and Baluchestan Province, Iran. The criteria for entering the study include informed consent, allocating 20 - 30 minutes, not being under the treatment of a psychiatrist or clinical psychologist, and not currently diagnosed with a substance use disorder. Among the exclusion criteria of the present study, lack of interest in completing the questionnaire, incompleteness of the obtained information, and having a diagnosis of psychiatric disorders during the last 1 to 6 months. Samples were selected from the target population according to the characteristics under study. Based on the Purposive sampling method, and according to Morgan’s sample size estimation table and Cochran’s number formula, a total of 320 healthcare workers were selected as the study population.
In this formula, N is the population size. The p statistic is the percentage distribution of the trait in the society, that is, the proportion of people who have the studied trait. The q statistic is also the percentage of people who do not have the trait under study. If the amount of p and q is not known, we used their maximum value, i.e. 0.5.
3.2. Procedure
The main purpose of the present study was to investigate the mental health status of treatment staff and its relationship with perceived social support, and there was no intention to compare treatment and non-treatment staff. However, the sample of the treatment staff of the present study includes doctors, specialist doctors, assistants, residents, nurses, midwives, paramedics, and administrative staff with less involvement, including hospital employees, university headquarters, guards, revenue department employees, and discharge have been.
In the selected cities, hospitals were selected based on COVID-19 admission rates and the staff’s direct or indirect contact with the patients. This study was approved by the Vice-Chancellor for Research and the Ethics Committee of Zahedan University of Medical Sciences, Zahedan, Iran. The ethics code for the research was IR.ZAUMS.REC.1399.017.
Regarding the high prevalence of COVID-19 during the study and our inability to complete the questionnaires with a pencil because of COVID-19 health protocols, an online version of the questionnaire was employed. Also, due to the fact that at the time of research design and implementation of our study, I was located in Zahedan province of Sistan and Baluchistan, Iran at the height of the COVID-19 pandemic, it was not possible to conduct the research in person. We used the online way to collect information. We used the https://survey.porsline.ir/website, which is in line with the implementation of software and the online version of research and obtaining information in Iran. With the initial registration on the site, the initial link was provided to the researchers. Then, the names of the hospitals under observation were obtained from Zahedan University of Medical Sciences, Zahedan, Iran. Then we obtained the information groups of the treatment and administrative staff of the hospitals. Finally, we sent this link on WhatsApp, Telegram, Instagram, email, and SMS. In the end, we received the output obtained from the online Pors-online site in Excel and then entered the information into the software. Online questionnaire link and collect information through https://survey.porsline.ir/s/kjLDY9W.
At first, the demographic information of each subject was obtained, and then two main research questionnaires were implemented and their information was recorded. An assessment was also performed using the Perceived Social Support Questionnaire Version 12 (13) and the General Health Questionnaire-28 Items (GHQ-28) (14).
3.3. Tools
3.3.1. General Health Questionnaire-28 Items
General Health Questionnaire (GHQ) was developed by Goldberg and Hillier in 1979 (14). The questionnaire has 28 questions and we used its Persian version to examine mental health in the treatment staff. The scoring system used in this questionnaire is Likert. The subject reads the question and expresses his opinion as not at all (0), to the usual extent (1), less than the usual extent (2), and much less than the usual extent (3). A total score of 23 or higher for each subscale indicates lack of general health, and a score lower than 23 indicates general health (15) Taghavi (16) In the Iranian population, the reliability of the questionnaire was reported as high and its alpha value for all items was equal to 0.90 and also the reliability obtained using Cronbach’s alpha was reported as 0.90.
3.3.2. Multidimensional Scale of Perceived Social Support (MSPSS)
This tool includes 12 items that were developed by Zimet et al. (17) which measured each person’s perceived social support on a seven-point scale, ranging from “disagree” to “completely agree” for each of the three subscales. The minimum and maximum score of the individual on the whole scale is 12 and 84, respectively, and in each of the subscales, it is 4 and 28, respectively. The validity and reliability of this scale were reported to be high by Zimet et al. (17). Salimi et al. (15) also reported the validity of this scale using Cronbach’s alpha method for the three subscales of social support from family, friends, and significant other (0.86, 0.86, and 0.82, respectively).
3.4. Statistical Analysis
First, the frequency and percentage of the demographic variables of the present study, including gender, age, workplace, education level, type of profession, and city, were checked based on the frequency and percentage. Then we examined the mean and standard deviation (SD) of the research variables, namely mental health and its subscales and perceived social support. In the following, we used Pearson’s correlation coefficient to investigate the relationship between mental health and perceived social support, as well as regression analysis for prediction. Finally, the collected data were described and analyzed in SPSS version 22.
4. Results
4.1. Demographic Information
In the present study, there were 320 samples. Overall, in the gender variable, 139 participants were female, equivalent to 43.4%, and 181 were male equivalent to 56.6%. in the age variable, the majority of healthcare workers were in the age range of 30 - 39 years (142 (44.4%)). in the literacy/education level variable, In the literacy/education level variable, 133 participants in the research, equal to 41.6%, had a bachelor’s degree, also 58 participants, equal to 18.1%, had a high school diploma or lower, and the number of other 58 participants was equal to 18.1%. percent had a master’s degree and 35 other participants, equivalent to 10.9%, had an associate’s degree. In addition, the studied samples were selected from different cities under the supervision of Zahedan University of Medical Sciences in Sistan and Baluchistan province, Iran. The number of 116 people from Zahedan was equal to 36.2%, 99 participants were from the city of Iranshahr, which was equal to 30.9%, 71 participants were from the city of Khash, which was equal to 22.2%, 31 participants were from the city of Saravan, which was equal to 9.7%, and 3 participants were from the city of Mirjaveh, which was equal to 0.9%. Regarding the frequency of the participants’ workplace, 170 of the participants, equivalent to 53.1%, were working in the hospital, 40 of the participants equivalent to 12.5% worked in medical centers, 37 of the participants, equivalent to 11.6% worked in healthcare centers, 25 of the participants, equivalent to 7.8% worked in the network center, 24 of the participants, equivalent to 7.5% worked in emergency departments, and 24 of the participants, equivalent to 7.5% worked in the central headquarters.
4.2. Mental Health Information
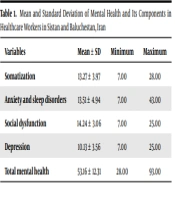
To confirm the research hypothesis, the mean and SD scores of variables were measured. Table 1 presents the participants’ mean and SD scores of mental health and its components.
| Variables | Mean ± SD | Minimum | Maximum |
|---|---|---|---|
| Somatization | 13.27 ± 3.97 | 7.00 | 28.00 |
| Anxiety and sleep disorders | 13.51 ± 4.94 | 7.00 | 43.00 |
| Social dysfunction | 14.24 ± 3.06 | 7.00 | 25.00 |
| Depression | 10.13 ± 3.56 | 7.00 | 25.00 |
| Total mental health | 53.16 ± 12.31 | 28.00 | 93.00 |
Mean and Standard Deviation of Mental Health and Its Components in Healthcare Workers in Sistan and Baluchestan, Iran
Table 1 presents the psychological disorders of healthcare workers participating in this study. The mean and SD of the total mental health score (53.16 ± 12.31) indicated the healthcare workers’ moderate mental health problems. The least prevalent mental health problem was depression (10.13 ± 3.56), while the most prevalent mental health problem was social dysfunction (14.24 ± 3.06). This finding suggests moderate mental health problems and social dysfunction in the medical staff during the COVID-19 pandemic.
4.3. Perceived Social Support Information
Table 2 presents the mean ± SD scores of social support and its components obtained by the healthcare workers.
| Variables | Mean ± SD | Minimum | Maximum |
|---|---|---|---|
| Perceived social support (family) | 21.92 ± 4.53 | 4.00 | 28.00 |
| Perceived social support (friends) | 19.23 ± 5.11 | 4.00 | 28.00 |
| Perceived social support (others) | 20.79 ± 5.16 | 4.00 | 28.00 |
| Total perceived social support | 69.95 ± 12.64 | 12.00 | 84.00 |
Mean and Standard Deviation of the Scores of Perceived Social Support and Its Components in Healthcare Workers in Sistan and Baluchestan, Iran
Table 2 indicates the perceived social support of healthcare workers during the COVID-19 pandemic. The mean scores of total perceived social support (69.95 ± 12.64) indicated the high level of perceived social support for healthcare workers. The highest perceived social support was related to perceived social support by families (21.92 ± 4.53). Overall, the results indicated the high level of social support for healthcare workers by their families, which play an important role during the COVID-19 pandemic. Pearson’s correlation coefficient test and regression analysis were also used to evaluate the research question regarding the mental health status of healthcare professionals involved in the treatment of COVID-19 patients in terms of perceived social support. Table 3 indicates the correlation matrix between the dimensions of perceived social support (predictive variables) and mental health and its dimensions (dependent variables).
| Predictive Variables | Somatization | Anxiety and Sleep Disorders | Social Dysfunction | Depression | Total Mental Health |
|---|---|---|---|---|---|
| Support by family | |||||
| R | -0.231 a | -0.240 a | -0.181 a | -0.336 a | -0.313 a |
| P-value | 0001.0 | 0001.0 | 001.0 | 0001.0 | 0001.0 |
| Support by friends | |||||
| R | -0.230 a | -0.236 a | -0.208 a | -0.312 a | -0.311 a |
| P-value | 0001.0 | 0001.0 | 0001.0 | 0.0001 | 0.0001 |
| Support by others | |||||
| R | 0001.0 | -0.125 b | -0.207 a | -0.256 a | -0.234 a |
| P-value | -0.181 b | 025.0 | 0.0001 | 0.0001 | 0.0001 |
| Total social support | |||||
| R | -0.250 a | -0.233 a | 0.234 a | -0.351 a | -0.334 a |
| P-value | 0001.0 | 0001.0 | 0001.0 | 0001.0 | 0001.0 |
The Correlation Matrix for Perceived Social Support and Mental Health and Its Dimensions in Healthcare Workers
4.4. Correlation Matrix Information
Based on the results presented in Table 3, there was a significant negative relationship between the healthcare workers’ perceived social support and mental health (R = -0.334, P ≤ 0.0001). Therefore, the increased perceived social support of healthcare workers reduced their mental health problems. Family support, as a perceived component of social support, was negatively and significantly associated with depressive disorder (R = -0.336, P ≤ 0.0001). Perceived social support had the most significant association with depression (R = -0.351, P ≤ 0.0001). Moreover, a simultaneous regression analysis was performed to predict the impact of perceived social support and its components on the mental health of healthcare workers. Table 4 presents a summary of the model and regression analysis.
| Model | Multiple Correlation Coefficient | Coefficient of Determination | Standard Error of the Mean | Df | F | Significance Level |
|---|---|---|---|---|---|---|
| 1 | 0.343 | 0.118 | 11.625 | 319 | 14.06 | <0.0001 |
A Summary of the Model and Regression Analysis
4.5. Regression Analysis Information
According to the results presented in Table 4, the multiple correlation coefficient was 0.343 and the coefficient of determination was 0.118. In other words, 0.118% of mental health variance could be predicted by perceived social support and its components. This model was also significant for predicting mental health (F = 14.06, P < 0.0001).
According to the results presented in Table 5, the beta coefficient obtained in the fixed model was equal to 41.47 and the obtained t-score was equal to 21.44, which was also significant (P > 0.0001).
| Model | Predictive Variables | Beta Coefficient | Beta | T | Significance Level |
|---|---|---|---|---|---|
| 1 | Constant Value | 71.47 | - | 21.44 | 0.0001 |
| Family | -0.457 | -0.168 | -0.089 | 0.037 | |
| Others | -0.093 | -0.039 | -0.567 | 0.571 | |
| Friends | -0.434 | -0.180 | -2.525 | 0.012 |
Regression Coefficients of Mental Health Based on Perceived Social Support
5. Discussion
This study was conducted comprehensively in Sistan and Baluchestan province, Iran, and was unique in its kind, and it was also a research project approved by Zahedan University of Medical Sciences. According to the present study, the medical staff of S Sistan and Baluchestan province, Iran, experienced many tensions and mental health problems during the COVID-19 pandemic when this province had many problems. The main mental health problem of the treatment staff was impairment in social functions and anxiety and sleep problems. The depression of the treatment staff had the lowest rate. The intensity of mental health problems in the medical staff of Sistan and Baluchestan province, Iran, was average. Also, considering the epidemic of COVID-19, the medical staff of Sistan and Baluchestan province, Iran, received the most perceived social support from their families. We also found that with the increase of perceived social support in the treatment staff during the COVID-19 pandemic, the amount of mental health problems also decreases. And this relationship was significant.
The results of the present study are consistent with those reported by Fang et al. (18), Li et al. (19), Shahid et al. (20), Wang et al. (6), and Asnakew et al. (21). The global spread of COVID-19 and its high mortality rates have posed serious challenges to different countries around the world. One of the most serious unrecognized and unaddressed challenges is the psychological problems of healthcare workers due to direct or indirect exposure to COVID-19 patients during the pandemic; these problems have caused major stress in healthcare professionals. In a review of six studies assessing several aspects of COVID-19 related mental health, psychological variables, such as inadequate social support, low self-efficacy, increased anxiety, depressive symptoms, and insomnia, were reported (22).
Since the first report of COVID-19, medical and paramedical staff have been dealing with major stressors, affecting their social, psychological, and personal lives. Fear of infection or family exposure, lack of concentration due to overwork, physical and verbal violence by the caregivers of COVID-19 patients, and fear of insecurity can result in mental health problems in the medical staff (20).
The results of this study showed that perceived social support had the most significant association with depression. The findings of this study are consistent with the previous studies. In 2021, Asnakew et al. (21) investigated the adverse effects of the COVID-19 pandemic on the mental health of 419 healthcare workers in Northwestern Ethiopia. Their results showed a high prevalence of depression (58.2%), anxiety (64.7%), and stress (63.7%). They also found that poor social support was significantly associated with high levels of anxiety and that participants with poor social support experienced far more stress during the COVID-19 pandemic. In another study conducted in Libya by Elhadi et al. (23) on 745 healthcare workers from 15 hospitals, 56.3% and 46.7% of the participants showed symptoms of depression and anxiety, respectively; it should be noted that these results were obtained when Libyan healthcare workers were also involved in a civil war with minimal social support.
Healthcare professionals have faced major challenges during the COVID-19 pandemic. The prevalence of mental health problems is increasing due to the death of healthcare workers’ colleagues, threats to their lives, fear of infection, lack of effective social support systems, and high workload (24).
Another important result of the current study was that family support, as a perceived component of social support, was negatively and significantly associated with depressive disorder. These results are consistent with those depicted in previous studies. For example, Liu et al. (25) found that in the context of the COVID-19 pandemic and its negative impact on mental health, social support from family and friends can protect against depression and PTSD symptoms. In other words, social support plays a moderating role in the association of the COVID-19 pandemic with mental health problems.
To reduce these mental disorders, it is important to meet the financial and physical needs of healthcare workers, provide them with healthy diets, reduce their working hours and consider rotating shifts, meet the care needs of their children, monitor their physical and mental health status, and identify the staff with burnout or psychological distress (26).
Overall, social support for healthcare workers can help achieve good patient prognoses during an epidemic and can be used to establish effective psychological interventions for the treatment of COVID-19 patients (18). One of the limitations of the present study was that it was a descriptive, correlational study and the studied variables were collected as a self-report. Also, due to the focus of this study on COVID-19 healthcare workers, there is a possibility for bias in the results because there is potential for these risk factors to occur in other healthcare settings that directly and indirectly deal with COVID-19 patients.
5.1. Limitations
The questionnaires were designed as self-reports and online, and there are limitations to the online test for this study. The issue of what state the respondents were in at the time of answering may have overshadowed our information, compared to When the questionnaire is filled in the presence of the researcher.
5.2. Conclusions
Mental health problems and insufficient support from the medical staff during the time of exposure to COVID-19 have had a significant negative impact on the quality of work life and its relationships. Overall, the medical staff experienced moderate mental health problems, with social dysfunction causing the greatest psychological disorders during the COVID-19 outbreak in Sistan and Baluchestan Province, Iran. More attention should be paid to the mental health and perceived social support of these workers, and their mental status should be regularly assessed. Therefore, perceived social support can significantly predict the mental health of healthcare workers, as it reduces the psychological problems of the medical staff.
The present study indicated that social support, especially from family and friends, can reduce mental health problems in medical staff.