1. Background
Parkinson’s disease is one of the most common progressive neurological diseases that cause a range of motor and non-motor symptoms and affects the patient’s quality of life (1). The prevalence of this disease is from 5 to more than 35 people per 100,000 people (2) and increases with age: 5 to 10-fold from the sixth to the ninth decades of life (3). With the tendency of communities to age, the prevalence of this disease also increases (4).
This progressive neurodegenerative disease does not have a definite treatment; therefore, progressive symptoms severely lower the quality of life and become a source of anxiety and distress for caregivers (5). To the best of our knowledge, determining the quality of life is suitable for checking the progress of the disease (6) plus managing chronic conditions (7).
Quality of life is the clients’ understanding and evaluation of themselves and the impact of their illness on their lives and its consequences. The concept of quality of life is a combination of the well-being of physical, mental, and social conditions in the framework of a specific disease (8). People with Parkinson’s disease and their caregivers seek assistance and support from the healthcare system to develop the necessary strategies and skills to adapt to life in the presence of a chronic illness (9).
Supporting clients through self-management is considered one of the most importantly supportive and educational activities by nurses, especially Rehabilitation Nurses, as they have the necessary medical knowledge and close contact with people suffering from chronic neurologic diseases so that they are aware of how the disease affects Quality of Life. Nurses must educate patients on self-management skills through regular symptom monitoring and careful assessment, promote self-efficacy, and improve treatment adherence (10).
Based on prior knowledge, self-management involves a set of measures to control symptoms, and comorbidities and prevent disease progression (11). It is crystal clear that with the effect of Parkinson’s disease on motor function, most patients have functional problems that prevent them from participating in counseling and ongoing treatment sessions (12). According to previous research, it was found that self-management education can be effective in patients with Parkinson’s disease, and on the other hand, the rising coverage of smartphones with practical applications is a promising strategy for PD self-management (13). Therefore, the usability of new technologies in chronic care has been recently recognized to help nurses in self-management education (14).
Despite numerous studies and trials conducted before, it cannot be concluded that there is a specific intervention that is completely effective for a disease (15); yet, it is recommended to develop the Application network and support patients through self-management (16). Considering the multiple needs of clients, nurses in close and constant contact with patients should try to formulate and implement self-care and self-management programs, help patients achieve maximum independence, and, thus, improve their quality of life (17).
As far as we know, Persian language self-management educational content based on a mobile application for Parkinson’s disease patients has not been designed in the field of rehabilitation nursing in Iran. On the other hand, problems related to in-person visits to clinics during the COVID-19 pandemic were considered: To decrease the risk of transmitting the virus, patients were less willing to take periodic visits (18), yet were more likely to receive online counseling sessions or mobile applications (18). Hence, in this study, we hypothesized that self-management education based on the mobile application affects the quality of life of people with Parkinson’s disease.
2. Objectives
In the present study, we evaluated the effect of self- management education based on the mobile application on the quality of life of Parkinson’s disease in patients referring to neurology clinics of selected medical education centers of Iran University of Medical sciences in 2021.
3. Methods
3.1. Participants
This quasi-experimental study was performed on 77 patients with Parkinson’s disease who entered the intervention group from August to November 2021, with a convenience sampling method in the neurology clinic of selected educational and medical centers of Iran University of Medical Sciences (Firoozgar and Hazrat-e-Rasoul hospitals). Based on a previous study that assessed the quality of life of Parkinson’s disease patients (19), to determine the required sample size assuming the effect of the intervention before, compared to one and three months later, the sample size was estimated to be at least 70 people, which was estimated to be 77 people by calculating ten percent sample loss during the study.
3.2. Eligibility Criteria for Participants
Inclusion criteria were: Previous confirmation of the disease in medical documents by a neurologist; being in mild and moderate stages of the disease (stages 1, 2, 3, 4) (20); ability to read and write Persian and use a mobile phone with Android operating system (13); if the patient was not able to read and write, or use the mobile application, we got help from a caregiver who had a mobile phone with Android operating system and the ability to use mobile application; we asked caregivers to provide educational content to patients: Either by having the patient use the caregiver’s phone to read the content or if the patient had limitations in using a smartphone (such as low literacy or vision problems), we asked caregivers to read the contents for them. Clients were excluded from the study if the client passed away or was hospitalized for other reasons during the intervention.
3.3. Instrumentation
Characteristics of the instruments used in this study are as follows:
- Demographic checklist, including information on age, sex, marital status, level of education, employment status, duration of diagnosis and use of drugs, and having insurance. These data were collected only to report the demographic information of the research subjects.
- The criteria for the clinical stage of the disease: The Hoehn and Yahr scale, which divides the disease into five stages, was presented simply so the subjects could choose the option near to the Patient's condition;
- The Parkinson's Disease Quality of Life Questionnaire (PDQ-39), the gold standard tool for examining the quality of life in people with Parkinson’s disease is the one designed by Jenkinson et al. in 1997 in the UK, known as Parkinson’s Disease Quality of life Questionnaire, which includes 39 questions in 8 aspects: Mobility, Activities of daily living, emotional well-being, stigma, social support, cognition, relationships, bodily discomfort. As this questionnaire is on the Likert scale, the first option indicates the best conditions with a score of zero, and the fifth option indicates the worst conditions with a score of four. In the end, the total score is one hundred points, which indicates the worst state of health, and a score of zero means no problem. The calculation of the score of each dimension is also expressed as a percentage: The total raw score of that part, divided by the maximum score in that dimension, multiplied by 100 (19).
In a study by Dehghan et al. on assessing the validity and reliability of the Persian version of this tool, Co-efficiency (Cronbach’s alpha) varied from 0.64 to 0.92 and was obtained above 0.70. Convergent validity has varied from 0.38 to 0.83, and in general, the Persian version of this tool is appropriate and acceptable and can be used to examine the quality of life of people with this disease (21).
In this study, the consent form was completed by the client or a caregiver who was able to read and write. Questionnaires were sent via an online link to clients through social networks.
3.4. Intervention
The content related to self-management education provided by the Mobile Application was extracted from reliable, up-to-date, evidence-based medical, nursing, and rehabilitation references by the author (rehabilitation nurse). The accuracy, precision, and validity of this information were approved by three faculty members of the School of Nursing and Midwifery at the Iran University of Medical Sciences.
In order to design the Mobile application, with the ability to install it on a smartphone under the Android operating system, we consulted with an experienced software engineer. After checking the compatibility of the content placement with the proposed graphics and matching the software standards with the existing content, the initial software was designed. Parkinson’s disease patients have vision difficulties, so the ability to enlarge texts and photos has also been added. The graphic consultant team also did the logo design. With the approval of the mobile application by five professors of the nursing faculty of Iran University of Medical Sciences, the application was made available to the people under research.
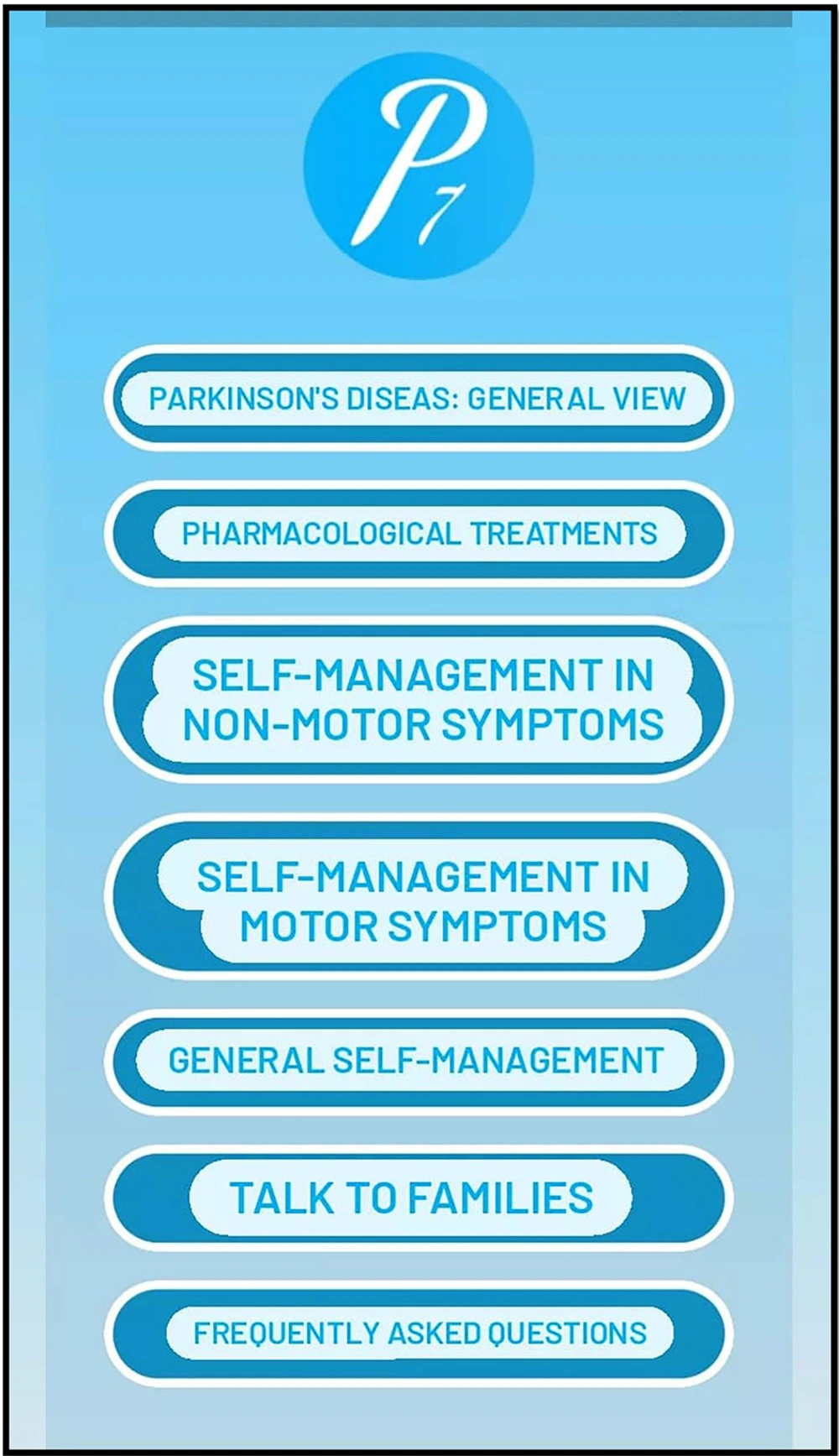
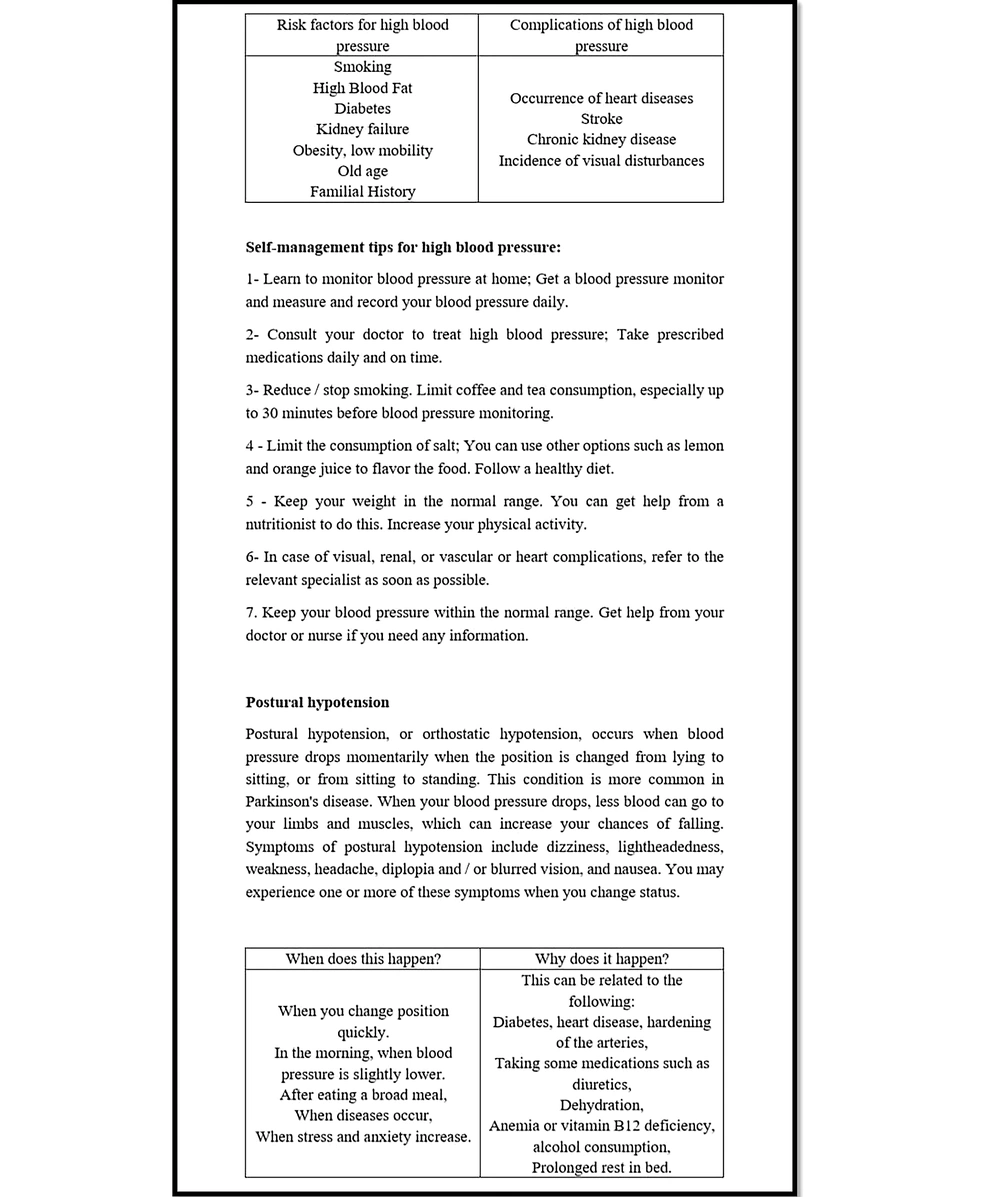
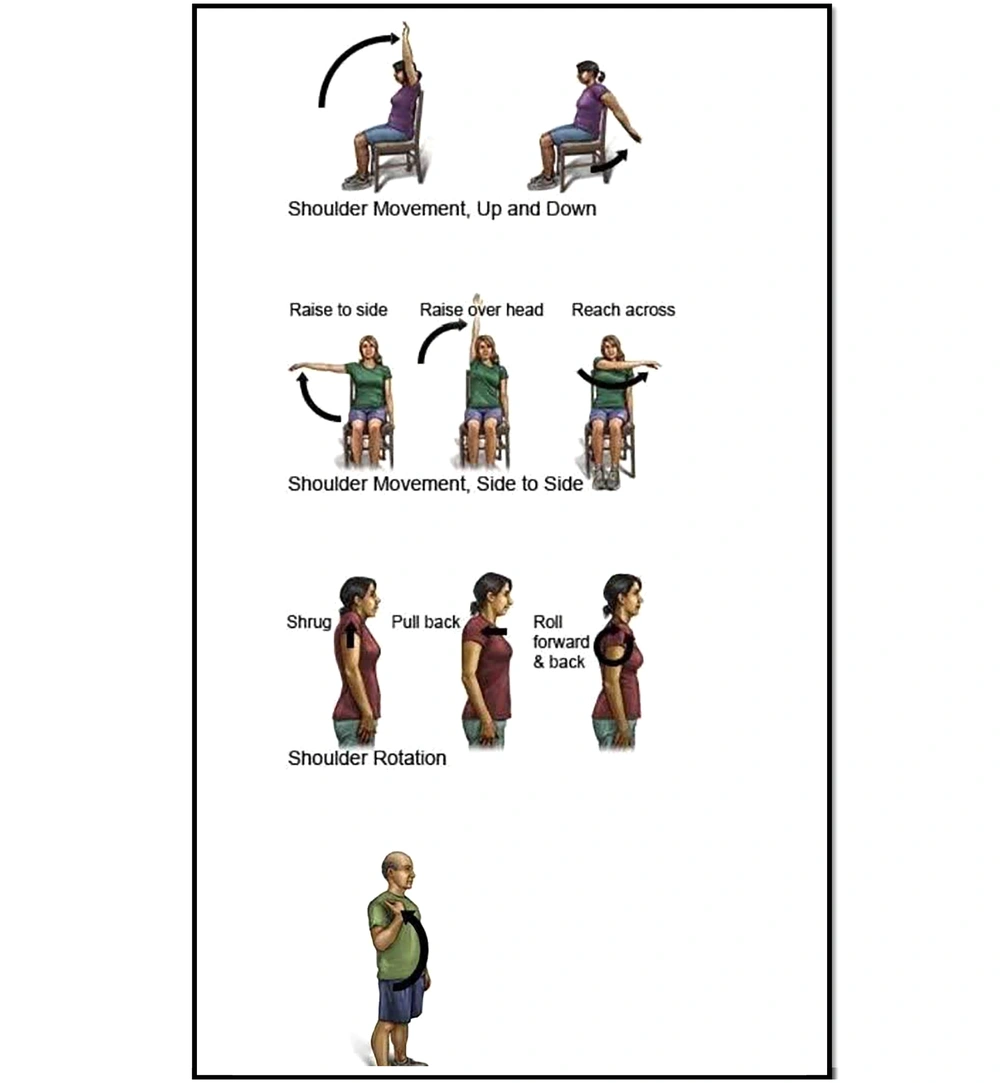
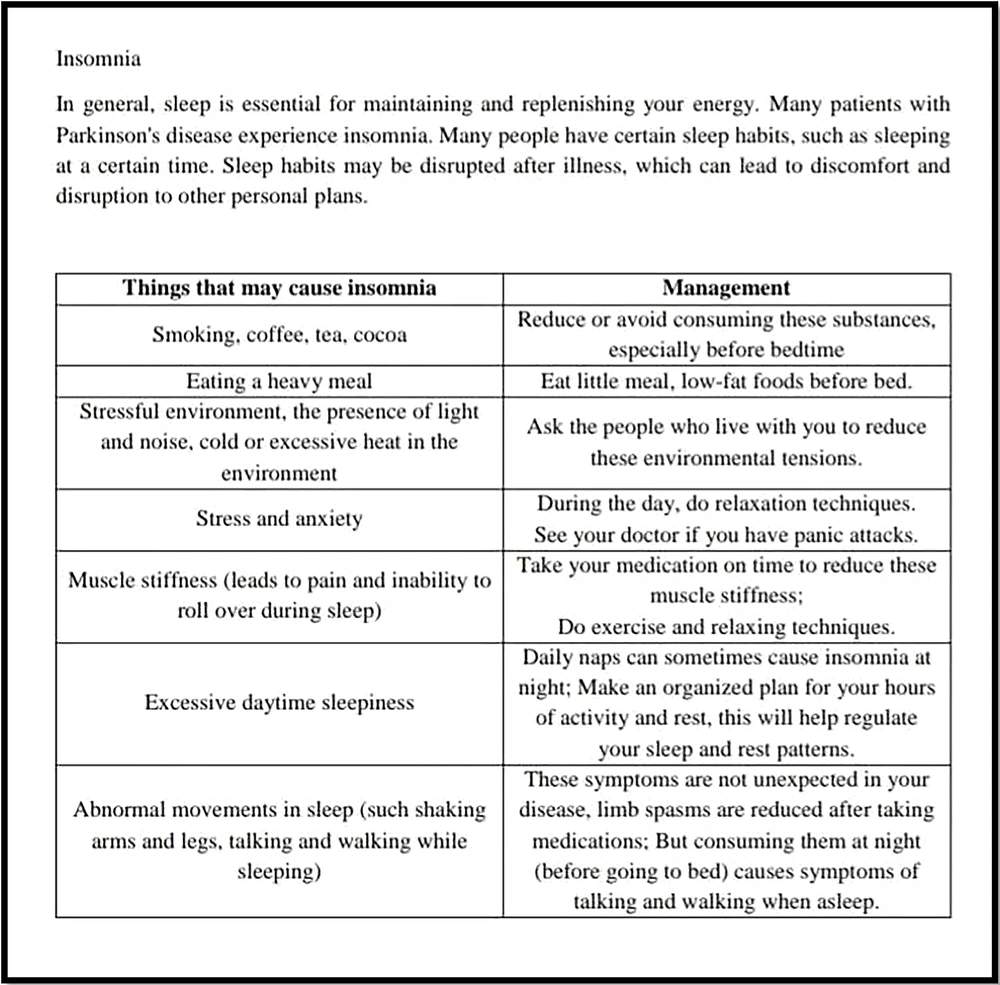
This mobile application could be installed on a smartphone running the Android operating system and could be used offline. The main features were: educational content, in Persian, related to (1) familiarity with the disease and symptoms, treatment methods, follow-up and adherence to treatment recommendations; (general overview of the disease); (2) pharmacological treatments (name of the drugs frequently used in this disease, indications, complication, and advice); (3) self-management in Motor symptoms (imbalance, gait disturbance and freezing, bradykinesia, tremor, masked face) including exercise (balance and corrective exercises for whole body), and safety advice; (4) self-management in non-motor symptoms (stress management, living with Parkinson’s disease, relaxation, cardiovascular problems, blood pressure, sleep and fatigue, mood, memory and cognition); (5) general self-management (gastrointestinal symptoms, nutrition management, urinary symptoms, pain, pressure ulcer, speech therapy and swallowing problems, advice about decoration change and taking notes everyday); (6) talk to families and/or caregivers (to prepare and improve conditions, supporting the family in using the application and accompanying the patient in self-management; how to decrease the burden generally); (7) frequently asked questions, and contacting the caring nurse (researcher). This mobile application called "ParkinSeven," was divided into seven sections and presented seven recommendations in each part, providing self-management content to the client at once.
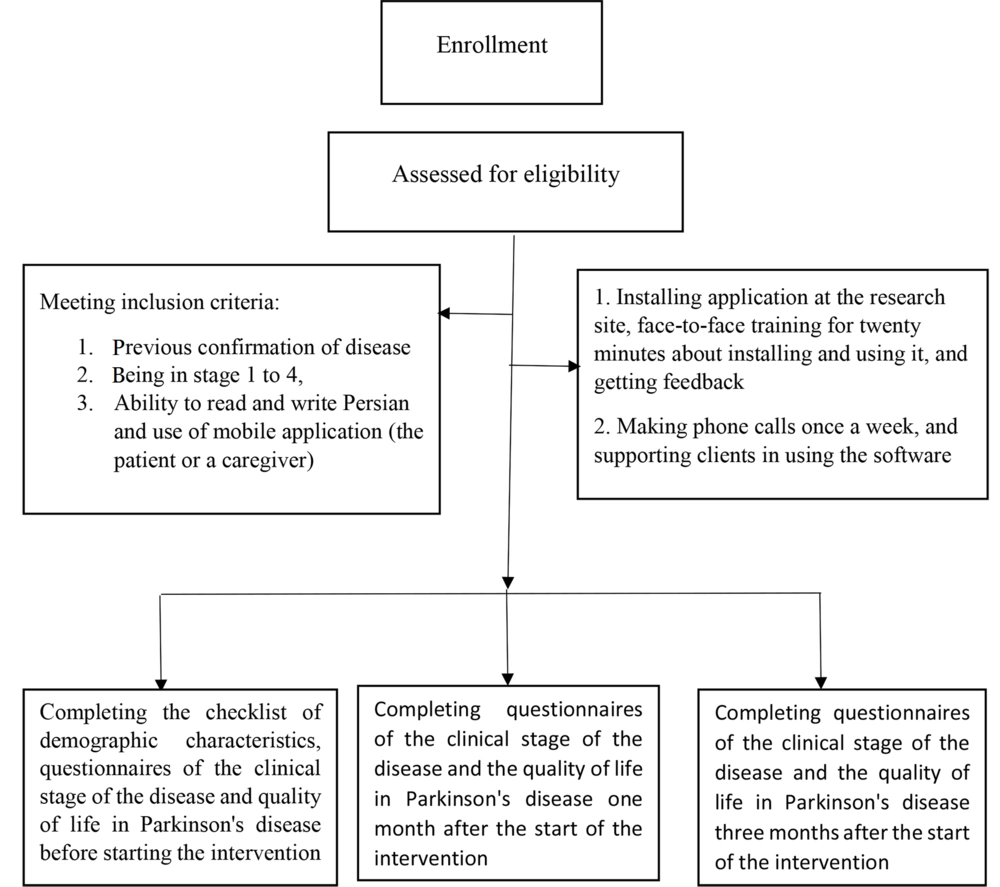
The researcher installed the application and taught us in person for about 20 minutes. They were asked to run the application for certainty. The demographic checklist, clinical stage criteria, and quality of life questionnaire in Parkinson’s disease (PDQ-39) were sent via online links to patients or a caregiver before, one month, and three months after the start of the intervention (12 weeks intervention). The author would support the subjects with a weekly phone call and answering online in order to use the application and check the subjects for keeping up with the intervention.
3.5. Statistical Analysis
Analysis of variance with repeated measures was used to compare before, one, and three months later, using SPSS version 20. The significance level for all analyses was 0.05.
4. Results
This study involved 77 patients aged 61.16 ± 12.58 (minimum 18 and maximum 84 years) of which 66.2% were men (Figure 1). Table 1 shows the frequency distribution of demographic characteristics. We did not anticipate any effect of demographic information on patients’ quality of life and did not find any similar study in the studies field in Iran. The obtained data can be used in future studies, and the relationship between factors and their impacts can be investigated in future research.
| Characteristics | No. (%) |
|---|---|
| Gender | |
| Female | 26 (33.8) |
| Male | 51 (66.2) |
| Sum | 77 (100) |
| Age | |
| ≤ 49 | 14 (18.2) |
| 50 - 59 | 17 (22.1) |
| 60 - 69 | 23 (29.9) |
| ≥ 70 | 23 (29.9) |
| Sum | 77 (100) |
| Employment status | |
| Employed | 19 (24.7) |
| Retired | 33 (42.9) |
| Pensioner | 11 (14.3) |
| Effete | 13 (16.9) |
| Covered by NGOs | 1 (1.3) |
| Sum | 77 (100) |
| Insurance status | |
| Insured | 68 (88.3) |
| Not insured | 9 (11.7) |
| Sum | 77 (100) |
| Educational status | |
| Lower than diploma | 34 (44.2) |
| Diploma | 28 (36.4) |
| Bachelor | 13 (16.9) |
| A higher degree | 2 (2.6) |
| Sum | 77 (100) |
| Marital status | |
| Married | 57 (74.0) |
| Widow/widower | 15 (19.5) |
| Divorced | 4 (5.2) |
| Single | 1 (1.3) |
| Sum | 77 (100) |
| Housing | |
| I live alone | 12 (15.6) |
| I live with my spouse | 13 (16.9) |
| I live with my spouse and child/children | 44 (57.1) |
| I live with my child/children | 8 (10.4) |
| Sum | 77 (100) |
Table 2 shows characteristics related to the disease in people with Parkinson’s under research. In Table 3, scores of quality of life and its dimensions can be seen before, one, and three months after the intervention. The findings of this table show a decrease (i.e., improvement) in overall scores and sub-dimensions of quality of life.
| Characteristics | No. (%) |
|---|---|
| Presence of underlying disease | |
| I have an underlying disease | 32 (41.6) |
| I do not have an underlying disease | 45 (58.4) |
| Sum | 77 (100) |
| Duration of diagnosis (y) | |
| ≤ 4 | 24 (31.2) |
| 5 - 9 | 18 (23.4) |
| 10 - 14 | 21 (27.3) |
| ≥ 15 | 14 (18.2) |
| Sum | 77 (100) |
| Min | 0.03 (3 mo) |
| Max | 21 |
| Mean ± standard deviation | 8.3813 ± 5.6693 |
| Clinical stage | |
| 1 | 22 (28.6) |
| 2 | 18 (23.4) |
| 3 | 19 (24.7) |
| 4 | 18 (23.4) |
| Sum | 77 (100) |
| Aspects and Stage | Mean ± SD | F | P-Value |
|---|---|---|---|
| Mobility | 198.911 | ≤ 0.001 | |
| 1 | 52.37 ± 31.22 | ||
| 2 | 35.90 ± 26.51 | ||
| 3 | 27.07 ± 23.19 | ||
| The activity of daily living | 183.44 | ≤ 0.001 | |
| 1 | 46.64 ± 28.91 | ||
| 2 | 29.76 ± 25.00 | ||
| 3 | 20.56 ± 20.15 | ||
| Emotional well-being | 159.69 | ≤ 0.001 | |
| 1 | 65.96 ± 26.16 | ||
| 2 | 43.72 ± 22.54 | ||
| 3 | 31.11 ± 20.59 | ||
| Stigma | 125.70 | ≤ 0.001 | |
| 1 | 57.79 ± 30.46 | ||
| 2 | 40.66 ± 25.23 | ||
| 3 | 30.27 ± 21.53 | ||
| Cognition | 131.55 | ≤ 0.001 | |
| 1 | 49.51 ± 25.94 | ||
| 2 | 35.55 ± 12.79 | ||
| 3 | 26.05 ± 18.03 | ||
| Relationships | 153.370 | ≤ 0.001 | |
| 1 | 47.61 ± 28.57 | ||
| 2 | 30.62 ± 22.31 | ||
| 3 | 20.45 ± 17.49 | ||
| Social support | 160.94 | ≤ 0.001 | |
| 1 | 39.82 ± 25.64 | ||
| 2 | 20.07 ± 17.94 | ||
| 3 | 12.50 ± 16.08 | ||
| Bodily discomfort | 205.54 | ≤ 0.001 | |
| 1 | 57.89 ± 26.45 | ||
| 2 | 38.26 ± 21.30 | ||
| 3 | 26.86 ± 6.81 | ||
| Quality of life | 194.924 | ≤ 0.001 | |
| 1 | 48.2670 ± 20.83 | ||
| 2 | 34.24 ± 18.25 | ||
| 3 | 24.33 ± 15.51 |
a In this table, number 1 shows the data obtained from the first stage, and numbers 2 and 3 show the averages obtained before, one, and three months after the start of the intervention, respectively.
The difference between the three stages in scores of eight dimensions and quality of life, before, one, and three months after the intervention, is shown in Table 4. The findings of this table indicate that in the dimension of emotional well-being, there was an average difference of 34.84 ± 2.46. This finding means that the greatest change and improvement has happened in the dimension of emotional well-being.
| Aspects | Comparison Between Aspects | Average Comparison in Aspects | |
|---|---|---|---|
| Mobility | 1 | 2 | 16.46 ± 1.32 |
| 1 | 3 | 25.29 ± 1.64 | |
| 2 | 3 | 8.83 ± 0.71 | |
| The activity of daily living | 1 | 2 | 16.88 ± 1.27 |
| 1 | 3 | 26.08 ± 1.75 | |
| 2 | 3 | 9.19 ± 1.00 | |
| Emotional well-being | 1 | 2 | 22.24 ± 2.07 |
| 1 | 3 | 34.84 ± 2.46 | |
| 2 | 3 | 12.60 ± 1.14 | |
| Stigma | 1 | 2 | 17.12 ± 1.69 |
| 1 | 3 | 27.51 ± 2.22 | |
| 2 | 3 | 10.39 ± 1.17 | |
| Cognition | 1 | 2 | 13.96 ± 1.21 |
| 1 | 3 | 23.45 ± 1.75 | |
| 2 | 3 | 9.49 ± 1.34 | |
| Relationships | 1 | 2 | 16.99 ± 1.52 |
| 1 | 3 | 27.16 ± 1.99 | |
| 2 | 3 | 10.17 ± 1.02 | |
| Social support | 1 | 2 | 19.75 ± 1.50 |
| 1 | 3 | 27.32 ± 2.03 | |
| 2 | 3 | 7.57 ± 1.00 | |
| Bodily discomfort | 1 | 2 | 19.62 ± 1.55 |
| 1 | 3 | 31.03 ± 1.85 | |
| 2 | 3 | 11.40 ± 1.15 | |
| Quality of life | 1 | 2 | 13.99 ± 0.82 |
| 1 | 3 | 23.93 ± 1.20 | |
| 2 | 3 | 9.94 ± 0.68 | |
a In this table, number 1 shows the data obtained from the pre-intervention phase, and numbers 2 and 3 show the averages obtained in one and three months after the start of the intervention, respectively. In each row, the average comparison of the first and second, first and third, and second and third steps can be seen.
5. Discussion
Parkinson’s disease is a neurodegenerative disorder with gradual onset and progression that eventually leads to disability (22). The goal of Parkinson’s treatment is to achieve maximum functional independence, safety, well-being, and, thus, health-related quality of life (23). Self-management interventions are designed for people with chronic diseases to help them respond to different aspects of illness (9).
A variety of interventions have been designed to support self-management by persons with Parkinson’s disease (24), yet this paper is the very first study conducted to investigate the effectiveness of self-management education by a rehabilitation nurse based on the mobile application on the quality of life of people with Parkinson’s disease. Although many studies have evaluated the effect of a mobile intervention for self-management in Parkinson’s disease (25), to the best of our knowledge, there has not been an organized academic study addressing the role of Rehabilitation Nurses in improving quality of life with a certain self-management intervention in Iran.
The results of this study showed that the post-intervention mean score of quality of life was significantly improved. In other words, this study proved the effectiveness of self-management education based on mobile applications has a positive effect on the quality of life of people with Parkinson’s disease, and this finding is consistent with the study of Chen et al. (26). Also, our findings emphasize that intervention through electronic health is effective on improving movement disorders in patients with Parkinson’s disease. This result is in line with a review study by the same researcher (27).
Lee et al. assessed the use of mobile apps for self-care in people with Parkinson’s disease in a review study and recommended the development of mobile apps focused on self-care that can enhance symptom management and health promotion practices, plus evaluate the effects of mobile apps on symptom improvement and quality of life in People with Parkinson’s disease (28). These findings are in line with the present study. Demos for running the application are available in Figures 2 - 5.
Nowadays, Health Care Providers, Policymakers, and clients wish to adopt low-cost comprehensive strategies that improve quality of life (9, 29). The self-management intervention implemented in this study was found to significantly improve the quality of life and its dimensions in patients. Observing positive effects in clinical care can be a valuable approach to assessing the consequences of educational interventions for clients and healthcare workers (30). Finally, with the growing use of smartphones with useful applications, promising self-management strategies are emerging in chronic neurological diseases such as Parkinson’s disease (13).
5.1. Limitations
Naturally, this study was not without its limitations. First of all, the effect of changing the drug dosage on clinical symptoms; the individuals’ symptoms may improve relatively due to the dose of the drug or simple changes in the medication plan, which is suggested to be monitored in future studies. Adequate cognitive status, plus age limitation, was not part of the inclusion criteria, which can be intervening variables. It is suggested that future studies control the range of age in participants and assess cognitive status with specialized tools before starting the study.
Also, the small number of samples and absence of the control group may affect the generalizability of the results of this study; future studies with more samples, longer follow-up duration designing a mobile application that all operating systems can run, and comparison with the control group is recommended. Researchers can E-mail the corresponding author to receive the educational content.
5.2. Conclusions
The present study showed that self-management education based on mobile applications positively affects the quality of life of people with Parkinson’s disease. Overall, our study re-emphasized the importance of self-management education for patients’ quality of life. Accordingly, it will be profitable to utilize the results of this beneficial research in educational and medical centers by clinicians, nursing staff, managers, and rehabilitation personnel to improve the quality of life of Parkinson’s disease patients.