1. Introduction
Urinary incontinence (UI) was recently defined as any involuntary loss of urine that causes a social or hygienic problem (1). It affects quality of life (QoL) even more than hypertension or diabetes (2). Nowadays, almost 4 million females and 1.7 million males have UI in Spain (2). This fact poses UI as an important problem for public health.
Urinary Incontinence is often treated inadequately (3). In one study, only 60% of patients seeking care for UI (leakage at least once a week) recalled receiving any treatment for incontinence (4). Additionally, nearly 50% of those, who did receive treatment, reported moderate-to-great frustration with ongoing incontinence (4).
Urinary incontinence may be defined according to patient’s symptoms as: 1) stress UI (SUI) as the complaint of involuntary leakage on effort or exertion, or on sneezing or coughing; 2) urgency UI (UUI) as the involuntary leakage accompanied or immediately preceded by urgency; 3) mixed UI (MUI) as the involuntary leakage associated with urgency and also with effort, exertion, sneezing, and coughing (1). Stress UI can be subdivided in grades, according to O’Brink scale, to mild, moderate or severe SUI (5). Types of UI are essential because treatment should be aimed towards the main concern (urgency, loss or both) and treatment algorithms are created on this basis (1).
Urinary Incontinence is multifactorial (5). The risk factors for female UI are pregnancy, delivery, menopause, gynaecological, abdominal, and urological surgery (6), while for male UI, these are radical prostatectomy, abdominal and urological surgery (6). On an overall view, UI is not evitable (because of the several associated risk factors), yet, UI is treatable or at least manageable (1).
Treatment of UI may be conservative and surgical. Conservatives modalities include bladder training (based on voiding dairy), lifestyle recommendations, pelvic floor muscle training (PFMT), manometric or electromyography (EMG), biofeedback (BFB), and pharmacotherapy (1, 5, 6). Surgical treatment includes slings, bulking agents, colposuspension, bladder augmentation, and sacral neuromodulation (1, 5, 6). An intermediate alternative is peripheral percutaneous neuromodulation (5).
To evaluate the effectiveness of UI treatment, validated instruments are highly recommended (frequency volume chart or bladder diary), in order to state the symptoms severity (1). To assess the patient’s perspective of symptoms on UI and their impact on QoL, high quality questionnaires are recommended (1). There are different questionnaires/specific scales to assess QoL in UI (2). Among them are the incontinence quality-of-life measure (I-QOL) and the international consultation on incontinence questionnaire short form (ICIQ-SF), both of which are available in Spanish and have been validated and frequently used (2). The King’s health questionnaire (KHQ) is another scale (7). The ICIQ-SF is a brief questionnaire, which allows detection of both UI, and its severity, type, and impact on QoL. It is scored from 0 to 21; the higher the score, greater the severity (Table 1) (5, 6). A score of 21 corresponds to total incontinence, while a score of 0 reflects complete continence (5, 6). The I-QOL specifically measures the QoL in UI. It is a scale of 22 items, each of them is assigned a value of 1 (very) to 5 (anything). It has a maximum value of 110 points, where higher scores mean better the QoL. For a better interpretation, it is transformed to a scale from 0 to 100. The I-QOL is divided to 3 subscales: limitation of activity or behavior (LB) with 8 items, psychosocial Impact (PI) with 9 items, and social embarrassment (SE) with 5 items (Table 2) (5, 6).
| Description | |
|---|---|
| 1) How often do you leak urine? (circle only one answer) | |
| Never | 0 |
| Once a week | 1 |
| 2 - 3 times/week | 2 |
| Once a day | 3 |
| Several times a day | 4 |
| All the time | 5 |
| 2) How much urine do you think you leak? That is, how much urine do you usually leak (whether you wear protection or not)? (circle only one answer) | |
| None | 0 |
| A small amount | 2 |
| A moderate amount | 4 |
| A large amount | 6 |
| 3) Overall, how much does leaking urine interfere with your everyday life? | |
| 1 - 2 - 3 -4 - 5 - 6 - 7 - 8 - 9 - 10 | |
| Not at all | Great deal |
| 4) When do you leak urine? Please tick all that applies to you. | |
| Never | |
| Before you can get to the toilet | |
| When you cough or sneeze | |
| When you are asleep | |
| When you are physically active/exercising | |
| When you have finished urinating and are dressed | |
| For no obvious reason | |
| All the time |
Abbreviations: ICIQ-SF, international consultation on incontinence questionnaire–short form. aICIQ-SF score: sum scores of 1 + 2 + 3 questions.
aAny score more than zero is considered as diagnostic for urinary incontinence.
bThe questions on the 4th Item (when do you leak urine?) helps to identify the type of urinary incontinence, whether stress urinary incontinence, urgency urinary incontinence, or a combination of both (mixed urinary incontinence).
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. I worry about not being able to get to the toilet on time. | |||||
| 2. I worry about coughing or sneezing. | |||||
| 3. I have to be standing after sitting down. | |||||
| 4. I worry about where the toilets are in new places. | |||||
| 5. I feel depressed. | |||||
| 6. I don’t feel free to leave my home for long periods of time. | |||||
| 7. I feel frustrated because my incontinence prevents me from doing what I want. | |||||
| 8. I worry about others smelling urine on me. | |||||
| 9. My incontinence is always on my mind. | |||||
| 10. It is important for me to take frequents trips to the toilet. | |||||
| 11. Because of my incontinence, it is important to me to plan every detail in advance. | |||||
| 12. I worry about my incontinence is getting worse as I get older. | |||||
| 13. I have a hard time getting a good night sleep. | |||||
| 14. I worry about being embarrassed or humiliated because of my incontinence. | |||||
| 15. My incontinence makes me feel like I am not a healthy person. | |||||
| 16. My incontinence makes me feel helpless. | |||||
| 17. I get less enjoyment out of life because of my incontinence. | |||||
| 18. I worry about wetting myself. | |||||
| 19. I feel like I have no control over my bladder. | |||||
| 20. I have to watch what or how much I have to drink. | |||||
| 21 My incontinence limits my choice of clothing. | |||||
| 22. I worry about having sex. | |||||
| The following scoring system is used for all the elements: | |||||
| 1: Always; 2: Usually; 3: Sometimes; 4; Rarely; 5: Never | |||||
| Subscales structure: | |||||
| (LB), Items 1, 2, 3, 4, 10, 11, 13, and 20 | |||||
| (PI), Items 5, 6, 7, 9, 15, 16, 17, 21, and 22 | |||||
| (SE), Items 8, 12, 14, 18, and 19 |
Abbreviations: I-QOL, incontinence quality-of-life; LB, limiting behavior; PI, psychosocial impact; SE, social embarrassment.
aCalculation of subscale score = (obtained sum by corresponding items/sum of maximum value of analyzed items) × 100%.
bCalculation of total score of the scale = (obtained sum by total items/110) × 100%.
The guide from the fourth international consultation on incontinence recommendations of the international scientific committee agrees that the first line management of UI should include lifestyle interventions and PFMT with or without BFB (1). However, there is no agreement on the protocols used to treat UI; that is, there is still worldwide controversy regarding frequency, intervals of treatment, and type of muscle exercise (tonic or phasic) (7).
It is well known worldwide that manometric biofeedback improves fecal incontinence (2), yet, there are scarce studies (if any) that demonstrate its effectiveness on urinary incontinence. On the contrary, EMG-biofeedback is the most used technique to treat urinary incontinence (5-7).
The burden of the disease is explained by the highest prevalence in older societies like in Spain (10% to 50% of prevalence) and the economic impact it has on the society due to long treatment protocols and the use of diapers. Recently, Fernandez-Cuadros et al. demonstrated that a 20-session treatment protocol of tonic exercises applied at Salamanca’s University hospital was capable of improving male’s (6) and female’s (6) QoL in all types of UI, including UUI, for the first time. However, the high impact of the disease and limited health resources have led to an economic barrier, especially in times of crisis.
This study aimed at investigating if a 6-session protocol of tonic-phasic exercises using manometric-biofeedback is capable improving QoL and muscular strength, measured by ICIQ-SF/I-QoL questionnaire/scale and by manometric BFB evaluation, respectively.
2. Methods
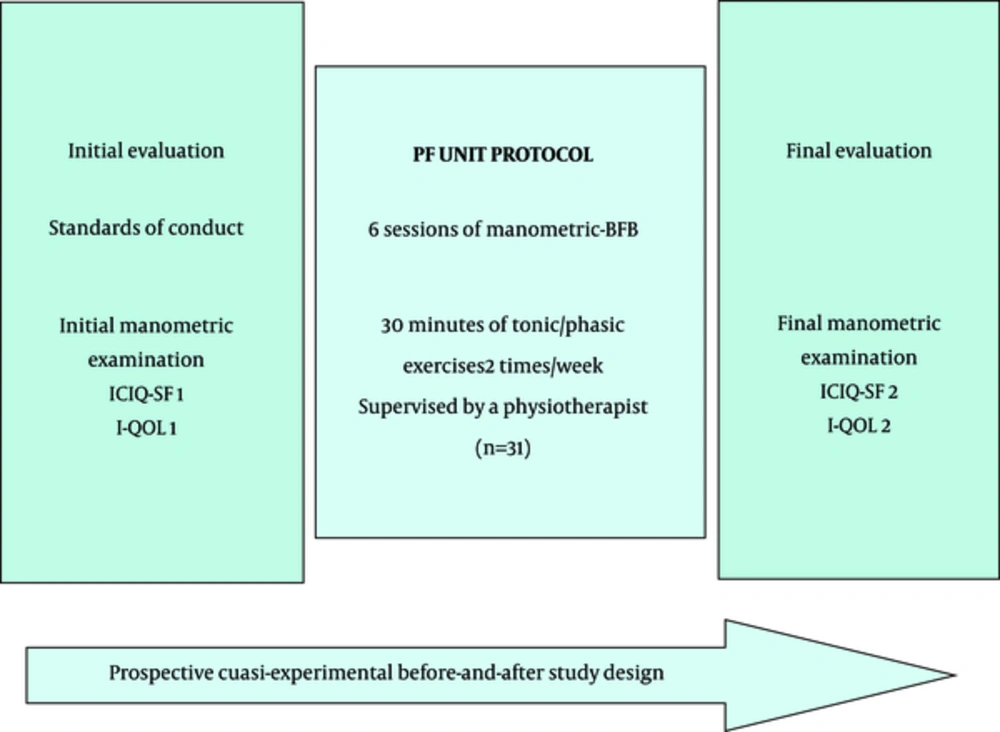
A prospective quasi-experimental before and after study was performed on a sample of 31 UI patients, who were referred to the rehabilitation department at Santa Cristina’s University hospital, Madrid, Spain. The study was conducted from January 2016 to December 2016 and it was accepted by the ethical committee of the hospital (Figure 1).
ICIQ-SF, international consultation on incontinence questionnaire-short form; I-QOL, incontinence quality-of-life; BFB, biofeedback. PF, pelvic floor. Protocol applied at the pelvic floor unit (PF) of the department of rehabilitation at Santa Cristina’s university hospital, Madrid, Spain. The study ran from January 2016 to December 2016.
The inclusion criteria were: 1) age of 18 years and older, 2) symptoms of urgency or leakage of urine or both, 3) referral to the rehabilitation department from Urology, gynaecology or familiar medicine departments, 4) provision of informed consent.
The exclusion criteria were: 1) lack of cooperation; 2) failure to understand the treatment protocol; 3) neglect and/or failure to fill the questionnaires/scales used; 4) failure to accomplish the manometric evaluation; 5) any severe neurological condition that caused inability to produce pelvic floor contractions (ictus, dementia, spinal cord injury, and others); 6) vaginal or urinary tract infection.
At the initial evaluation, affiliation data, medical history, predisposing factors (age, gender, pregnancy, delivery and menopause, gynaecological, urological or abdominal surgery) and type of UI were recorded. Patients were given lifestyle recommendations and questionnaires/scales to be filled at the beginning and the end of treatment (Table 3).
| Urinary Incontinence: Advices | |
|---|---|
| - | Avoid constipation (drink plenty of liquids, eat rich fiber meals, do exercise), avoid obesity, smoking and exhausting exercises. |
| - | Do not stop urinating. Go to urinate every 2 - 3 h. |
| - | Do not push to finish empting the bladder. |
| - | Do contract pelvic floor muscles while making efforts like coughing, loading, sneezing, and if you are in the imperious need of urinating. |
| - | Repeat the Biofeedback pelvic floor learned exercises, six times a day, at different moments, cycles of 10 repetitions (3 seconds of contraction, 7 seconds of relaxation) for tonic exercises, and 5 fast contractions and 10 seconds rest (for 10 times) for phasic exercises. |
The used equipment was MYOMED ® 932, which allows manometric-BFB with the use of a vaginal probe for female patients and a rectal probe for male patients. This electrical device emits auditory and visual signals, which can be seen on the screen, serving as a biofeedback for contraction of the pelvic floor muscles. This goal is sometimes difficult to be performed, especially in very old or very young patients.
The probes are covered by a preservative and lubricated with a medical gel solution before insertion in the vagina or rectum. The evaluation of the muscle contractions is made by manual evaluation. The grading system goes from 0 to 5 and it is correlated with the manometric values obtained by the BFB equipment (8) (Table 4).
| Manual Evaluation | Manometric Preassure, mmHg | Manometric Preassure, hPa |
|---|---|---|
| 0 | 0 | 0 |
| 1 - 2 | 1 - 30 | 1 - 39 |
| 3 - 4 | 31 - 40 | 40 - 52 |
| 4 - 5 | 50 - 60 | 65 - 78 |
| 5 | > 60 | > 78 |
The manometric biofeedback protocol consisted of a 30-minute session, duration of pelvic floor muscle contractions, divided by 15 minutes of tonic exercises (3 seconds/work and 6 seconds/rest contractions), and 15 minutes of phasic exercises (5 rapid contractions followed by 10 seconds of rest), 2 times a week for up to 6 sessions, using a vaginal or anal probe (as needed), connected to MYOMED ® 932 Biofeedback-equipment, and supervised by a physiotherapist.
The recorded signal observed on the screen served as a catalyst for motor learning. In the initial and final evaluation, a 2-minute continued manometric evaluation was performed (1 minute of tonic and 1 minute of phasic exercises) in order to obtain the maximum and mean manometric session contraction. These values served as an objective measure to demonstrate the strengthening of the muscles over time. However, the values obtained are still a matter of controversy (8). All 6 sessions were performed by manometric biofeedback, to reinforce the correct execution of the tonic and phasic exercises.
For the statistical analysis, the SPSS ® version 20.0 software was used. Means and standard deviation (SD) were used for the descriptive analysis of quantitative variables. Frequencies and percentages were used for the analysis of qualitative variables. For the evaluation of quantitative variables before and after the treatment, a paired t test was used. The significance was established at a 99% level (P < 0.01).
3. Results
A total of 31 out of 35 patients that had been referred to the Pelvic floor unit at the rehabilitation department, Santa Cristina’s University Hospital, were studied. Patients were referred by Family Medicine, Urology, and Gynaecology specialists. Mean age of the sample was 52 ± 12.1 years.
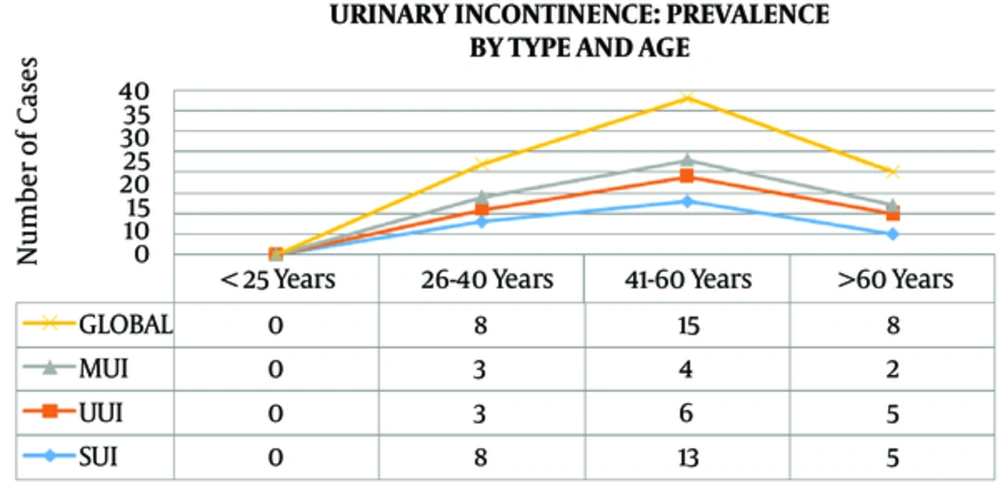
The UI increased with age, with the most frequent prevalence at 41 to 60 years old, decreasing slightly after this point. This phenomenon was observed globally, and in all subtypes of UI (Figure 2).
Urinary Incontinence is most frequent in females (2, 5-7). In this study, of the 31 patients, 30 were females (96.7%).
Except for 1 patient, who performed 9 sessions, most of patients executed 6 sessions of treatment (mean sessions were 6.16).
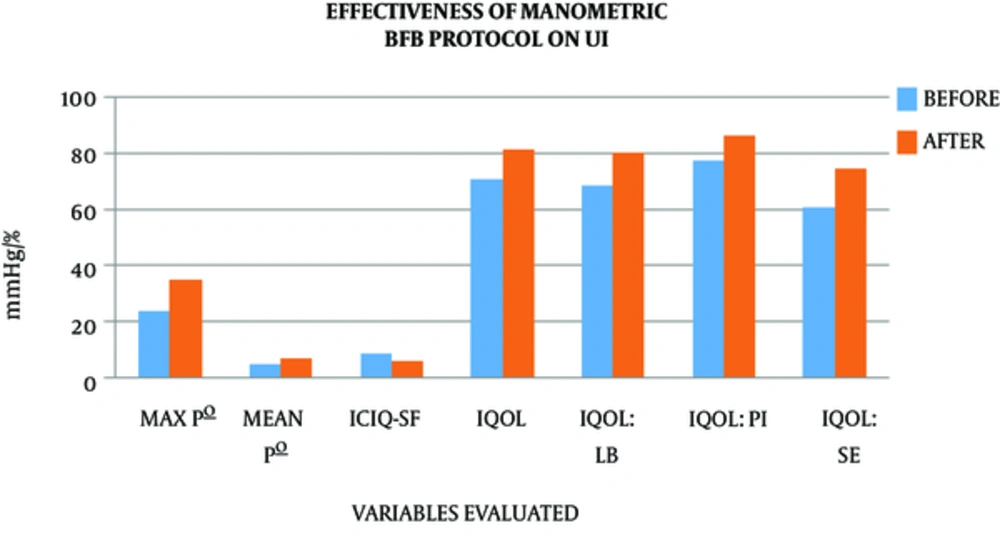
The maximal and mean strength of contraction of pelvic floor muscles evaluated during 2 minutes at the initial evaluation was 24 ± 17.72 and 4.9 ± 4.1 mmHg, respectively. After the 6-session manometric-BFB protocol, the maximal and mean manometric values increased to 35 ± 20.85 and 7.45 ± 4.92 mmHg, respectively, all with statistical significance (P < 0.001).
The symptom severity of UI, evaluated by ICIQ-SF, was 9.13 ± 5.18. After the treatment protocol, the symptoms ameliorated, decreasing significantly the values of ICIQ-SF to 6.13 ± 4.75 (P = 0.003). With respect to the QoL, measured by I-QoL, the global values increased significantly from 70.33 ± 22.12 to 81.25 ± 16.72 (P = 0.0017). When the I-QoL sub-scales were compared, all of them showed significant improvement. The I-QoL LB-subscale (Limiting Behaviour) raised from 68.38 ± 23.33 to 80 ± 16.56 (P = 0.0015); I-QoL PI-subscale (psychosocial impact) increased from 77.43 ± 24.51 to 80 ± 17.47 (P = 0.0152); and I-QoL SE-subscale (Social Embarrassment) incremented from 60.72 ± 22.37 to 74.37 ± 20.86 (P = 0.0007) (Table 5 and Figure 3).
| Variable | Before (mean ± SD) | After (mean ± SD) | P Value |
|---|---|---|---|
| MAX P°, mmHg | 24 ± 17.72 | 35 ± 20.854 | 0 |
| MEAN P°, mmHg | 4.9 ± 4.1 | 7.45 ± 4.92 | 0.0002 |
| ICIQ-SF (0 - 21) | 9.13 ± 5.18 | 6.13 ±4.75 | 0.0003 |
| IQOL (0 - 100) | 70.33 ± 22.12 | 81.25 ± 16.72 | 0.0017 |
| IQOL: LB (0 - 100) | 68.38 ± 23.33 | 80 ± 16.56 | 0.0015 |
| IQOL: PI (0 - 100) | 77.43 ± 24.51 | 86.23 ± 17.47 | 0.0152 |
| IQOL: SE (0 - 100) | 60.72 ± 22.37 | 74.36 ± 20.86 | 0.0007 |
Abbreviations: ICIQ-SF, international consultation on Incontinence questionnaire-short form; I-QoL, incontinence quality of life scale; LB, limiting behaviour; PI, psychosocial impact; SE, social embarrassment; MAXP°, maximal pressure; MEAN P°, mean pressure.
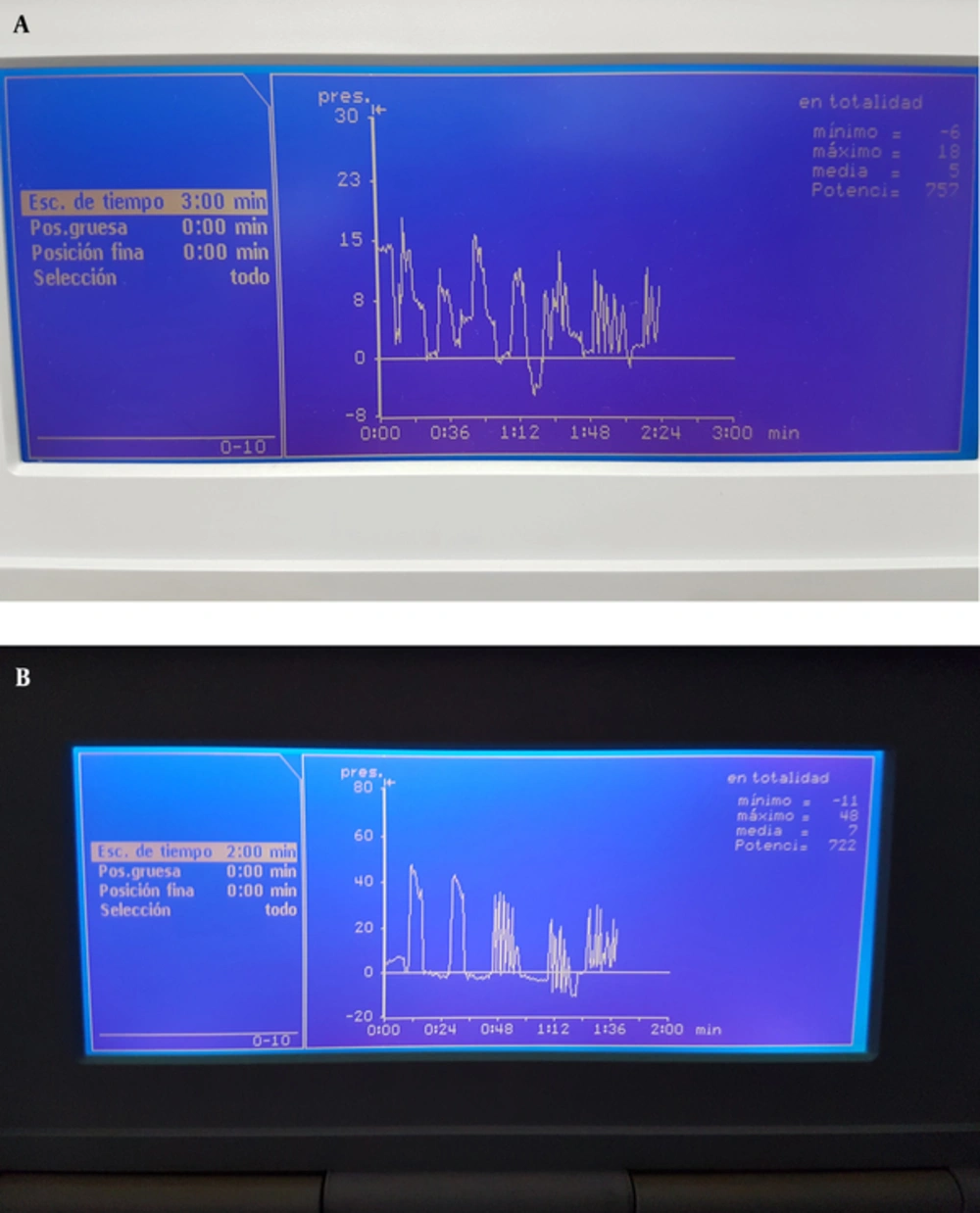
When the shape of lines from tonic and phasic exercises were evaluated on the screen of the BFB-equipment MYOMED ® 932, an increase of the maximum and mean parameters was observed, while a change in the shape of lines were also confirmed, before and after treatment (Figure 4).
4. Discussion
Urinary Incontinence is a clinical problem that most people deny because of shame and because they consider it is a problem of aging (6). It has great economical, social, and psychological impact (10), thus effective measures should be taken to solve it.
Biofeedback is a technique by which a physiological process that is usually unconscious is presented to the patient and to the therapist through a visual or audio signal or a combination of both. This signal is subsequently used to teach and correct the physiological process, achieving a therapeutic effect (8, 11). Biofeedback is considered as an operant conditioning therapy (12). It is thus an instrumental technique of PFMT with permanent feedback and in a close chain. This operant conditioning therapy is known as Skinner’s type and it is some what different from the classic Pavlov’s conditioning therapy, in which a stimulus is substituted by another (13). In USA, BFB is supported by extensive evidence and therefore is accepted as a paid treatment for 3 pathologies, migraine and tensional headache (14), urinary (6), and faecal incontinence (15), as the Harvard Pilgrim Health Care Institute states for its medical policies on biofeedback.
Most studies worldwide have stated that EMG-BFB is an effective technique for the treatment of UI (5-7, 16, 17). In the case of manometric-BFB and UI, studies are scarce. Most of manometric-BFB studies have been done on the treatment of faecal incontinence. There subsides the importance of this study.
Manometric-BFB is not recommended for patients with vaginal athresia (colpoathresia), in virgin females and in children (13); in such cases EMG-BFB is the recommended technique, and therefore is currently the most used BFB technique.
Urinary Incontinence is related to aging and is more common in females (18), as it was observed in the current study. The most common age was between 41 and 60 years, as already stated by Geanini-Yaguez (5) and Fernandez-Cuadros (6). The most common UI type in this study was SUI, followed by UUI and MUI, as stated by Espuna-Pons (19).
The high prevalence and the economic and social impact on public health allows us to study if as many as 6 sessions of manometric biofeedback protocol are effective enough to improve QoL and manometric values of patients with UI. In times of crisis, it is essential to develop effective and low cost treatments.
To date, there has been controversy on treatment protocols related to frequency, intervals of treatment, and type of muscle exercises (tonic or phasic) used for UI (6, 7). For example, Hay-Smith suggested that the regimen should consist on 3 sets of 8 to 12 tonic contractions sustained for 8 to 10 seconds each, and performed 3 times a day; these must be continued for 15 to 20 weeks (20). Munoz -Bono reported that the treatment protocol for faecal incontinence might vary from 1 to 15 sessions, which is due to the difference in learning and comprehension between patients, as stated by Rao (21, 22). Gilliland goes even further and states that BFB effectiveness seems to be related to the number of sessions (23). Several authors reported that duration, number, and frequency of sessions are variable. Rao supports 3 to 6 sessions, 60 to 90 minutes in duration, while Suarez-Crespo suggests 4 to 6 sessions of 45 to 60 minutes duration (24). Fernandez-Cuadros et al. demonstrated that 30 minutes of tonic exercises, 2 times a week for up to 20 sessions is effective for diminishing losses and improving QoL in male and female patients with urinary and faecal incontinence (6, 25).
With respect to BFB protocols, as already stated by different authors worldwide, there is great variation and controversy on treatment protocols; some investigators state that duration should last 30 to 60 minutes (26). Grosse supports that at the beginning of BFB, the duration per session should not exceed 10 to 15 minutes, including the resting time, because of fatigue and concentration factors (14). Guerra-Mora stated that frequency of sessions should be 1 or 2 per week. As the exact number of sessions to get the maximal contraction on pelvic floor muscles is not known, Guerra-Mora observed that after 3 sessions of EMG-BFB, there is no greater improvement on pelvic floor contraction, yet, the maximal force was maintained up to 6 sessions (26). That is the reason why only 6 sessions of manometric-BFB protocol in the current study demonstrated effectiveness in improving manometric values and QoL.
When it comes to deciding the type of BFB, Suarez-Crespo stated that the ideal method depends on the availability, the expertise, and the experience of the caregivers (24). In the hospital of the current study, there was years of experience using manometric-BFB, so this technique was applied for the patients with UI. Moreover, Suarez-Crespo suggested that EMG-BFB and manometric-BFB are similar regarding efficiency (24). However, the effectiveness of different BFB techniques is still under debate. Glia stated that manometric-BFB is superior to EMG-BFB, while Heymenn claimed that there is no significant difference between them (27). What is clear is that BFB shows good efficacy in short term, measured by QoL scales and by psychological state (28). However, in the long term, follow-up studies indicate a fading effect over time (28). Even though, a high percentage of patients (up to 50%) continue to report satisfaction even after 12 to 44 months since treatment (29).
Biofeedback improves UI, yet, the mechanisms are still unclear (27). The reason why BFB (an instrumental technique of PFMT) is effective on UI might be because: 1) PFMT activates the perineum-detrusor inhibitory reflex (R3 of Mahony) (13) acting on UUI episodes (5, 11); 2) PFMT maintains the correct position and mobility of the urethra, which is fundamental especially for female incontinence (7); 3) PFMT compresses the urethra against the pubic symphisis increasing intra urethral pressure, thus giving resistance to voluntary voiding of urine (7), acting on SUI; 4) PFMT protects passive containment elements (ligaments and fibrous elements) and nerve structures from exposure to stretch (13, 30).
Several studies have demonstrated the effectiveness of EMG-BFB on UI basically on SUI and UUI (Robles and Sari) (9, 17). Recent studies have demonstrated EMG-BFB utility even on UUI in male and female patients (Geanini-Yagüez and Fernandez-Cuadros) (2, 5, 6). Unfortunately, there are only a few studies on the effectiveness of manometric-BFB on UI and its subtypes. There subsides the originality and the importance of the study. There is no doubt that manometric BFB is effective on faecal incontinence, as almost 60 studies support it (25). The present study demonstrated that manometric BFB improves manometric values and UI, measured by I-Qol (as already stated by Sari and Garcia-Bascones) (9, 31) and ICIQ-SF (as Lorenzo-Gomez and Glazer and Lane previously reported) (7, 32).
The objective to use validated instruments on UI, such as ICIQ-SF and I-QoL, is to provide evidence for the severity of symptoms before treatment and to evaluate the impact of BFB protocol after treatment (1). This improvement is clearly observed in our study, and with statistical significance.
Whether manometric-BFB produces improvement on manometric values in the contraction of pelvic floor muscles is still a matter of controversy, and the mechanisms involved are still poorly understood (9). Guerra-Mora stated that improvement of EMG-BFB values showed no clear correlation, neither with symptoms nor with QoL (26). Seiman observed that in the BFB treatment, the size of improvement in anorectal pressure gradient or in anal electromyography activity does not seem to be relevant to treatment outcome (33). Fernandez-Cuadros observed that although the shape of exercises on EMG-BFB protocol got better, the intensity of contraction did not increase significantly after treatment (2.97 mV vs. 2.67 mV); in fact, it already diminished, although not significantly (P = 0.28) (2). According to Grosse, the reason for this observation is that adipose tissue, cutaneous resistance, vaginal impedance and electrodes positioning are very variable, and the obtained measures have no value between sessions. It would be reliable only if the measures are made on the same session and with the electrodes kept on the same position during the evaluation (13). Even so, Marrinaci claimed that the improvement on strength of muscle contraction is correlated with BFB measures (13).
Apart from all the controversy on BFB measures, in this study, the manometric-BFB protocol improved the QoL measured by ICIQ-SF and I-QoL scales/questionnaires, and significantly increased maximal and mean manometric values of pelvic floor muscles (P < 0.001).
The execution of manometric-BFB protocol by the supervision of a physiotherapist and the use of visual and/or auditory signals allowed patients a correct execution of the tonic/phasic exercises protocol. The partnership between patient-physiotherapist: a) increases patient satisfaction and improves compliance and adherence to treatment, b) lets a rapid recognition of pelvic floor muscle exercises (13), and c) enhances learning and comprehension of exercises, since the number of sessions are dependent on patients motivation and cognitive level (21, 22).
The 6-session manometric-biofeedback protocol implemented at Santa Cristina’s Hospital improved QoL and reduced UI, as compared with other protocols, which are substantially larger, as the one introduced by Fernandez-Cuadros et al. (20-session protocol) (5, 6). This finding has direct impact on the health care system, because of the shortness and effectiveness of the protocol, and it could therefore be recommended to other public and private institutions, due to its cost/effectiveness properties.
The UI produces an economic impact derived from direct and indirect costs. The direct cost of UI includes diagnosis (specialist consultation and exams), rehabilitation, pharmacologic and surgical treatment, diapers, washing/cleansing products, and transportation expenses to medical facilities. The indirect cost includes labour absenteeism, productivity impairment, quality of life impairment, and caregiver’s salaries. In the USA, the direct cost per patient (diagnosis and treatment) was 600 dollars. In patients older than 65 years of age, the cost can go up to 3,565 dollars per patient. In Spain, a physiotherapist session is valued 53 euros per day (8). The reduced protocol will have an impact on the health system (less number of sessions and less use of medical resources) and in the economy of patients (less use of diapers).
One important limitation of this study was the absence of control group due to the small sample size (n = 31). Since PFMT and BFB have proven effects on the improvement of UI, it is not ethical to deny such an intervention for patients with UI. A quasi-experimental before-after study, also known as a non-randomized control trial, was used to solve such an ethical problem. Besides, it was an experimental study with recognised medicine-evidence based level (2B, according to the Canadian task force) (34).
4.1. Conclusions
Manometric BFB protocol is capable of decreasing UI and improving QoL and manometric values, measured by ICIQ-SF/I-QoL scale/questionnaire and by manometric BFB evaluation. This reduced protocol could be applied to other public and private institutions and it could have an economic impact on the health system and on patients’ economy.