1. Background
Disability resulting from the developmental disorders in children is associated with a reduced performance. In addition to poor body function and structure, the environment is also an obstacle that limits participation in activities (1). Self-care includes basic activities of daily living (ADL) that humans engage in from the beginning of life (2). Eating and swallowing, bathing and showering, toileting, and toilet hygiene, dressing, functional mobility, personal hygiene, and grooming are among these activities (3).
Participating in self-care is one of the crucial aspects of a child's health, well-being, and development, and one of the main predictors of life satisfaction in future for a child and his/her caregivers (4). Failure to perform ADL was independently recognized by the World Health Organization (WHO) as one of the greatest health problems worldwide. Children's difficulties in ADL caused a high dependence on others, and a heavy burden of responsibility for the family, caregivers and health care providers (5).
A literature review shows that a large number of children with the cerebral palsy (CP) have problems to perform ADL in terms of the motor problems (6), children with intellectual disability (ID) are unable to perform ADL and are dependent on their caregivers (5), and children with autism spectrum disorder (ASD) face difficulties to do these activities independently due to sensory, cognitive, practical and perceptual defects (7). The greatest functional difference in children in terms of independence level of ADL is related to pre-school age, which is affected by the attitude of parents and their parenting style (8).
Pediatric Evaluation of Disability Inventory (PEDI), Children's Participation Questionnaire (CPQ), Functional Independence Measure for Children (WeeFIM), the Vineland Adaptive Behavior Scale (VABS) are among the tools which evaluate ADL in children. These tools were not developed based on Iranian culture, and they examine several areas, one of which is ADL. People's views on independence/dependence/interdependence in children's self-care activities are affected by cultural values (3). Family beliefs, values, and attitudes about child rearing, independence, and self-reliance affect children's ADL performance (9). Therefore, it is important to evaluate ADL in specific socio-cultural context of the clients. Activities of Daily Living in Iranian Children (ADLIC) scale specifically evaluates ADL in Iranian normal preschool children, which was developed by Soltaninejad et al. (10).
Performing ADL tasks is usually selected as one of the family's priorities in client-centered goal setting (11-13). Since that accurate assessment is required to develop a full therapy, it may be claimed that therapists can only make sound clinical reasoning and deliver the most effective intervention for ADL if they conduct an accurate assessment (6). ADLIC scale addresses these tasks in normal children, but rehabilitation professionals need to measure ADL in children with disabilities.
2. Objectives
This paper aims to show the psychometric properties of ADLIC scale to obtain a modified version for disabilities, to name it the Activities of Daily Living Inventory for Children with Disabilities (ADLIC-D). The study conducted in three phases: (1) face validity, (2) content validity, and (3) convergent, and discriminant validity, internal consistency, and test-retest reliability.
3. Methods
3.1. Study Design
In terms of its objectives, the current research is basic or fundamental; in terms of its data gathering strategy, it is descriptive and cross-sectional. This research was conducted in three phases, and a methodological mixed method was used.
3.2. Participants
The participants were selected by convenience sampling which were different for each phase of the study:
Phase 1: Participants were 20 mothers of the children with ASD, CP, or ID.
Phase 2: Participants were 10 occupational therapists.
Phase 3: Participants were 205 mothers of children with ASD, CP, or ID as well as normal children.
After explaining the purpose and process of the study, the participants signed a written consent form. Inclusion criteria for participants were as follows:
• Mothers, as main caregivers of subjects in phases 1 and 3, had to be literate and without psychiatric diagnosis.
• Children with disabilities in phases 1 and 3 were aged 3 - 6 years (3 to 6 years and 11 months old) and diagnosed with ASD, ID, or CP by a child psychiatrist or neurologist. Children with cerebral palsy should not have cognitive problems based on Sparkle form (14). Using the Gilliam Autism Rating Scale (GARS), the autism level of children with ASD had to be recorded in their medical records (15). Regarding the degree of their mental condition, the IQ of children with ID should be recorded in their medical records.
• Occupational therapists as experts in phase 2 should have at least 15 years of experience in the field of children's rehabilitation, teach at a university of medical sciences, and have published articles in this field in reputable journals.
• Normal children in phase 3 should be aged 3 - 6 years, have no history of disorder or long-term illness, and have no long-term medication use based on the kindergarten records and parents' reports.
Incomplete information and parents' lack of consent to continue cooperating or using their information caused the exclusion of study. The sample was selected from Tehran (Iranian Down syndrome association and private rehabilitation clinics), and Yazd (Kindergartens and autism centers affiliated with the welfare organization) from August to December 2021.
3.3. Instruments
3.3.1. The Activities of Daily Living in Iranian Children Scale
The Activities of Daily Living in Iranian Children (ADLIC) scale is a parent-report inventory developed by Soltaninejad et al. for normal children aged 3 - 6 years (10). The bathing/washing/personal hygiene, clothing, eating/feeding, and functional mobility categories of this 73-item measure each include 19, 13, 18, 8, and 15 items. A 5-point Likert scale is used to assess the ADLIC scale (totally dependent, moderately dependent, relatively independent, adaptively independent, and totally independent). Overall score (range 0 - 365) is interpreted. A higher total score indicates greater independence to perform ADL (10). Internal consistency (Cronbach's alpha 0.96), ICC (0.95 - 0.98), and convergent validity between ADLIC, and Pediatric Evaluation of Disability Inventory (PEDI) (self-care = 0.88, mobility = 0.80) were reported as good (16).
3.3.2. Pediatric Evaluation of Disability Inventory
Pediatric Evaluation of Disability Inventory (PEDI) assesses ADL in children ages 6 months to 7 years. This tool includes three areas of self-care (73 items), mobility (59 items), and social function (65 items). It scores from three aspects, including functional skills (1 = capable, 0 = unable), caregiver assistance (5 = independent, 4 = supervision, 3 = minimum assistance, 2 = moderate assistance, 1 = maximum assistance, and 0 = total assistance), and the amount of modification (no modifications, child oriented modifications, rehabilitation equipment, and extensive modifications). Persian version of PEDI prepared by Moradi Abbasabadi et al. (17). The internal consistency was reported as 0.94, test-retest reliability for all items was 0.8-0.95, and content validity for all items was above 0.8 (18).
3.4. Procedure
3.4.1. Phase 1: Face Validity
After obtaining the code of ethics, the first author visited the sampling centers to study participants’ inclusion criteria via the demographic questionnaire. Face validity was examined using a qualitative method. Sixty mothers of the children with ASD, CP, and ID responded to each of the 73 items of the scale in the form of an in-depth open-ended interview in terms of compressibility, content clarity, and construct consistency. The study team evaluated and compiled the data they had collected from these interviews. In this phase, the ADLIC scale received 4 additional items, and a new test format was developed for use in the content validity phase. Hereafter, the scale will be referred to as ADLIC-D.
3.4.2. Phase 2: Content Validity
Content validity index (CVI) and content validity ratio (CVR) were calculated. At first, the test was sent to the experts via email. The experts determined the relevance and quality of each item in the CVI form, and the necessity of each item in CVR form. The experts' opinions were summarized and the necessity of each item calculated via Lawshe scale (19). The version resulting from content validity assessment was prepared in a meeting with the research team. The adjustments were then approved by all content validity experts in a subsequent virtual conference, and the administration and scoring rules for the ADLIC-D were also considered. Hence, scoring scale remained as 5-points; but for better understanding, changes were made in the description of each score. Besides, in this meeting, it was suggested to add a section called "examiner's guide" at the beginning of inventory. In this examiner's guide, general explanations for administration, and explanations for each item were designed. Then, based on the details of items to avoid mistakes by the parents to complete the inventory, the administration method was changed from parent-report to interview.
3.4.3. Phase 3: Convergent and Discriminant Validity, Internal Consistency, and Test-Retest Reliability
The groups with disabilities and normal group were recruited to study convergent and discriminant validity, internal consistency, and test-retest reliability. ADLIC-D and PEDI were completed in the form of interview with mothers. To assess test-retest reliability, the ADLIC-D was administered once again to 140 mothers two weeks later. The majority of the interviews were performed over the phone because of the Covid-19 epidemic.
3.5. Statistical Analysis
CVR and CVI formulas were used to check content validity. CVI score above 0.79 for the item suggests its appropriateness, between 0.79-0.70 means revision is needed, and below 0.70 means that item is unacceptable. To calculate CVR, based on Lawshe table, since the number of experts was 10, the necessity of each item was confirmed if the CVR score was higher than 0.62 (19).
The normality of data examined using Kolmogorov-Smirnov statistic. To evaluate the internal consistency, Cronbach's alpha coefficient values of more than 0.9, 0.7 - 0.9, 0.6 - 0.7, and less than 0.5 indicated high, good, weak, and unacceptable, respectively (20). In order to look into the convergent validity, the Pearson correlation coefficient between the ADLIC-D and PEDI scores was assessed. Moreover, test-retest reliability and discriminant validity were assessed using this correlation coefficient. The values of 0 - 0.29, 0.30 - 0.49, 0.50 - 0.69, 0.70 - 0.89, and 0.9 - 1.00 were considered as little, low, moderate, high, and very high correlation coefficients, respectively (21).
IBM SPSS Statistics for Windows, Version 26.0 (IBM Crop., Armonk, NY, USA) was used for data statistical analysis.
4. Results
4.1. Phase 1: Face Validity
Three items were added to the original test (“putting on and taking off slippers when going to the toilet”, “closing the zip”, “holding a cup and placing the mouth to drink”), and one item was split into two separate items. "Eating textured and mixed foods" was separated into "eating solid and chunky foods" and "eating mixed foods".
4.2. Phase 2: Content Validity
Two items were added ("using toothpaste while brushing'' and "drinking from a straw"), and one item was split into two separate items ("going up and down stairs" to "going up stairs" and "coming down stairs"). At this phase, four items were removed according to the opinion of experts, as shown in Table 1.
| Item | Content Validity Ratio | Domain |
|---|---|---|
| 1. Adjusting the water temperature (hot and cold) | 0.6 | Bathing/washing/personal hygiene |
| 2. Tidying things up after showering | 0.4 | |
| 3. Washing toothbrush and putting it back | 0.6 | |
| 4. Rinsing hand and face | 0.4 |
As a result of the phases 1 and 2, the ADLIC-D structure consisted of 76 items in total, including 16, 14, 19, 11, 16 items in the areas of bathing/washing/personal hygiene, toileting, dressing, eating/feeding, and functional mobility, respectively. Major changes were made to the form and administration of the instrument, as well as the substance of the items, to accommodate for children with disabilities. These changes included defining each score, modifying the scoring system, and adding an explanation column to the score sheet.
4.3. Phase 3: Convergent and Discriminant Validity, Internal Consistency, and Test-Retest Reliability
In this phase, 205 mothers of children with and without disabilities participated. The children with disabilities included 45 children with CP based on Gross Motor Function Classification System (GMFCS) (15 level I and II, 15 level III, and 15 level IV and V), 45 children with ASD (15 at each level of I, II, and III), and 45 children with ID (15 from each mild, moderate, and severe level). Moreover, 70 mothers of normal children participated. The demographic information of children is presented in Table 2. Gender distribution was almost equal. The majority of the children (61%) had siblings. The distribution of data was normal.
| With Disability (N = 135) | Normal (N = 70) | Total (N = 205) | |
|---|---|---|---|
| Age, y (mean ± SD) | 5.22 ± 0.80 | 5.98 ± 0.41 | 5.48 ± 0.78 |
| Age range, y:mo (min - max) | 3:2 – 6:9 | 5:0 – 6:9 | 3:1 – 6:9 |
| Gender, No. (%) | |||
| Girl | 60 | 40 | 100 (48.8) |
| Boy | 75 | 30 | 105 (51.2) |
| Number of children in family, No. (%) | |||
| One | 53 | 27 | 80 (39) |
| Two | 67 | 37 | 104 (50.7) |
| Three | 12 | 5 | 17 (8.3) |
| Four | 3 | 1 | 4 (2) |
The test-retest reliability revealed that the intra-class correlation coefficient (ICC) is over 0.9, which is regarded as a very strong correlation, in a sample size of 140 persons (50 normal subjects, 30 ASD, 30 CP, and 30 ID subjects).
Cronbach's alpha was 0.977 in total, which was considered excellent. To examine the internal consistency at the level of items, that is, the correlation between each of the items with the other items, the correlation coefficients were strong in more than 80% of the items.
Convergent validity among ADLIC-D total score, and PEDI (functional skills scale and caregiver assistance scale) showed that there is a significant correlation (P ≤ 0.05). Since ADLIC-D has a direct relationship with PEDI in two scales of functional skills (r = 0.953), and caregiver assistance (r = 0.944), it can be interpreted that ADLIC-D has high convergent validity with PEDI.
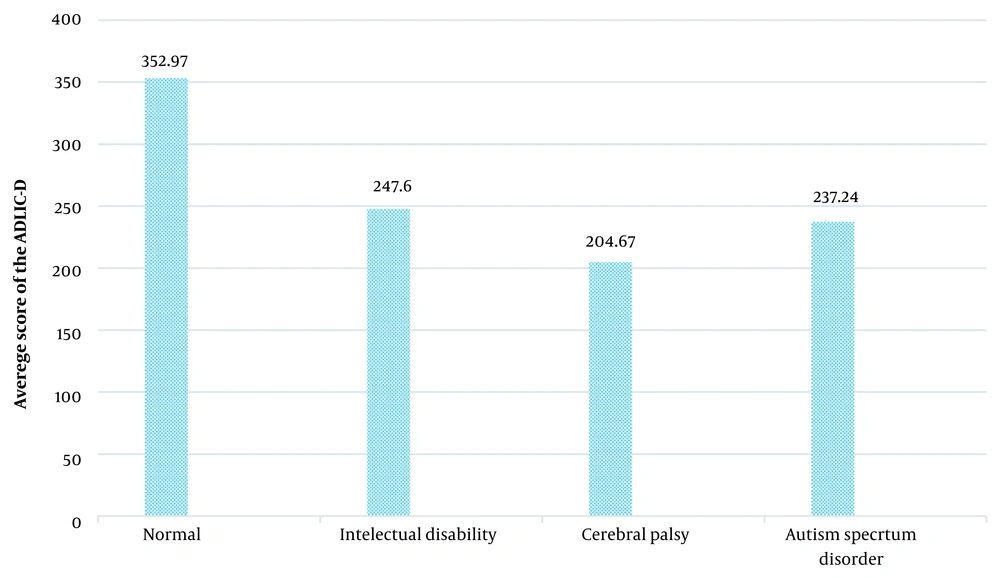
Examining discriminant validity of ADLIC-D showed that the different groups with disorder and the normal group do not have a significant correlation or have a weak correlation with each other. By comparing the mean ± standard deviation of the normal group (352.97 ± 6.216) and the groups with disorder as a whole (229.84 ± 65.6699), ADLIC-D is able to discriminate the normal group from the groups with disorder. That is, the mean of two groups shows a significant difference (P = 0.00).
To find that this instrument is able to discriminate among ASD, CP and ID groups, one-way ANOVA showed that the discriminant validity of ADLIC-D was optimal for differentiating self-care abilities in children with ASD, CP and ID. In order to find out which two groups have a significant difference, the Post Hoc test was done. It showed that ADLIC-D can have a significant difference between ID and CP, as well as CP and ASD (P ≤ 0.05) (P ≤ 0.05) while there was no significant difference between ID and ASD (P > 0.05) (Table 3). Besides, the comparison of the mean of groups with disorder showed that the normal group had the highest mean score, followed by ID, ASD, and CP groups, respectively (Figure 1).
| Group 1 | Group 2 | Mean Difference | Standard Error | P-Value |
|---|---|---|---|---|
| Normal | Intellectual disability | 105.371a | 9.866 | 0.000 |
| Cerebral palsy | 148.305a | 9.866 | 0.000 | |
| Autism | 115.727a | 9.866 | 0.000 | |
| Intellectual disability | Normal | -105.371a | 9.866 | 0.000 |
| Cerebral palsy | 42.933a | 10.885 | 0.000 | |
| Autism | 10.356 | 10.885 | 0.343 | |
| Cerebral palsy | Normal | -148.305a | 9.866 | 0.000 |
| Intellectual disability | -42.933a | 10.885 | 0.000 | |
| Autism | -32.578a | 10.885 | 0.003 | |
| Autism spectrum disorder | Normal | -115.727a | 9.866 | 0.000 |
| Intellectual disability | -10.356 | 10.885 | 0.343 | |
| Cerebral palsy | 32.578a | 10.885 | 0.003 |
a The mean difference is significant at the 0.05 level
5. Discussion
This research was set out to study the validity and reliability of ADLIC-D to prepare an appropriate instrument to evaluate self-care skills in the children with disabilities. As mentioned in the results section, changes were made in the items in the face and content validity phases; in other words, to adapt the tool for children with disabilities, it was necessary to remove some items and add others. Throughout the content validity procedure, several adjustments (item additions/deletions) to their scale were also done in a related research by Schulze et al. Nine questions were added to the functional skills section of the PEDI throughout the translation and face validity processes, and it was psychometrically assessed in both typically developing children and children with CP and ASD (22). These findings confirm that a valid instrument for normal children needs some modifications to be validated for children with disabilities. In the children with disabilities whose performance components are impaired, performing an activity becomes more complex than normal health conditions. In this case, adapting a tool for use in the children with disabilities requires a more detailed analysis of ADL functional skills.
The findings showed that internal consistency of ADLIC-D was confirmed. The items evaluated a common construct and work well together. A high Cronbach's alpha suggests that the respondents had a similar understanding of the items and did not have divergent interpretations of them. It means that the interpretation and understanding of all interviewees with each type of disorder and level of disability of the children was the same (23). This type of reliability was confirmed in similar tools, such as the PEDI. In a study by Chen et al. aimed at cross-cultural comparisons of the PEDI, as a similar tool to ours, it had excellent internal consistency in American and Taiwanese children (24). Since internal consistency is part of reliability methods, this fit reflects the accuracy, reliability, and stability of the ADLIC-D, and indicates that all items evaluate a single construct.
To justify the low correlation of some items with the others in the item level analysis, it can be concluded that the subjects of present study had three types of disorders with defects in different performance components and skills. For example, the parents of children with CP were more likely to report difficulties on ADLIC-D activities with greater motor demands than the other two disorders. Therefore, in terms of the heterogeneity of disorders, this correlation was low. It seems that increasing the sample size and homogenizing the subjects may increase these correlation coefficients.
The results showed that ADLIC-D has good test-retest reliability, similar to other well-known assessment tools for ADL, such as WeeFIM (25) and PEDI (26). The high test-retest reliability of the ADLIC-D indicates that the measured construct was stable over two weeks. The high reliability indicates that confounding variables such as common life experiences in the past few days do not affect the ADLIC-D result. The ADLIC-D's test-retest reliability is a benefit for its use in clinical trials because it gives a researcher the assurance that changes between the pre- and post-test are solely the result of the intervention and not simply the passage of time. To evaluate the convergent construct validity, PEDI was chosen as the second instrument. PEDI is a validated and standardized scientific and clinical tool. Therefore, it is commonly used to examine convergent validity in the psychometric studies of ADL assessments (27). This study’s results showed that ADLIC-D has acceptable convergence with PEDI. In conclusion, ADLIC-D measures the same construct (self-care) that PEDI assesses, and it can be stated that ADLIC-D is a valid and valuable tool for ADL assessment.
The findings of divergent validity showed that ADLIC-D can be suitable for screening normal children and children with disorders. Moreover, ADLIC-D differentiates between children with ID and CP, as well as between children with CP and ASD in terms of self-care skills. The only two groups that the ADLIC-D could not differentiate between were ID and ASD. It seems that common cognitive deficits in ID, and ASD seem to make it difficult to distinguish between two groups.
Other findings of this study showed that the children with CP have the least ability in ADL skills. This finding can be resulting from the movement-disorder nature of this disorder. ADL tasks are mainly repetitive motor actions and are not as cognitively challenging as academic or social tasks. In support of this idea, a study by Smits et al.’s showed that there is a close relationship among these activities, and gross motor abilities in preschool children with CP (28). In comparison among other groups, the lower mean score in the children with ASD compared to the group with ID can be justified in terms of the more complex cognitive, and sensory problems of children with ASD (12).
In this study, the researchers attempted to choose a sample with various physical-motor, mental-cognitive, and communication-social problems so that the final tool might be used for a wide range of disorders with different levels of abilities in children. Thus, by preparing ADLIC-D, it is possible to evaluate self-care skills in Iranian children with disorders with specialized tools of Iranian culture.
The main limitation of this study was its implementation during Covid-19 pandemic due to the closure of kindergartens and rehabilitation centers, which created problems in sampling.
Considering this instrument should be conducted with the parents of children with disabilities in the form of an interview, it is suggested that the inter-rater reliability of ADLIC-D be investigated in future studies.
5.1. Conclusions
ADLIC-D showed acceptable reliability and validity for the parents of children aged 3 - 6 years with physical and intellectual disabilities. This tool can be a guide for rehabilitation interventions in clinical and research fields by carefully examining the functional skills necessary to perform ADL.