1. Background
Suicide is a deliberate and conscious act done by a person to kill himself not by accident or aimlessly, but to escape from a very painful problem or crisis (1). This phenomenon is considered a multifactorial behavior (2) and a major problem around the world (3). A wide range of personal, familial, economic, cultural, and social factors affect suicide (4). According to global statistics, the rate of suicide death is generally higher in men than in women. For instance, in countries with a high human development index, the rate of mortality following suicide attempts is 19.3 and 5.9 cases in men and women in every 100,000 individuals, respectively; this might be the reason for the smaller number of studies on suicidal behaviors in women (4).
The epidemiological patterns of suicide are not identical in different communities. For instance, in China, the rate of suicide attempts is higher in women than men (5). Besides, the results of some studies have shown that the rate of suicide mortality is higher in Iranian women than men (6). Generally, the scope of the impact of suicide attempts is too broad, as they can have destructive effects on families, friends, colleagues, and communities. Evidence suggests that each suicide attempt can severely affect 5 - 15 friends and relatives (5). It is believed that suicide is a progressive phenomenon, and suicidal thoughts, plans, and preparations occur before suicide (7).
The prevalence of addiction was estimated 4.3% in the population aged 15 - 64 in Iran in 2015, while this rate is reported 0.57 and 0.03 percent in China and Japan, respectively (8). Also, according to official reports, the average arrest rate of drug addicts in Iran has increased more than 7 times from 1992 (43.84 per hundred thousand people) to 2001 (312.02 per hundred thousand people) (9), which shows that in addition to the relatively high prevalence of drug use in Iran, the trend of its use is also increasing.
The effects of drug abuse on suicide attempts have been investigated in several studies. The results of these studies have shown that women with drug abuse are 6.5 - 9 times more likely to commit suicide than women who do not use drugs (10). However, the impact of drug addiction in other family members on women’s suicide attempts merits particular attention.
2. Objectives
With this background in mind, the present study aimed to examine the effect of addiction of family members and other related factors on women’s suicide attempts.
3. Methods
3.1. Study Population
This case-control study was conducted in Golestan Province, Iran. The case group consisted of 220 women, aged 15-65 years, who had a history of suicide attempts, whereas the control group consisted of 220 women without a history of suicide attempts. To recruit the case group, a list of all suicide attempts in 2020 was prepared based on the Health Information System (HIS) of Golestan Province. The case participants were selected through systematic random sampling. The control participants were also selected by systematic random sampling using the same information system after excluding individuals with a suicide attempt history. The inclusion criteria were willingness to participate in the study, minimum age of 15 years, and maximum age of 65 years. On the other hand, unwillingness to participate in the study, age below 15 years, and age above 65 years were the exclusion criteria.
3.2. Data Collection Method
After obtaining approval from the Institutional Ethics Committee of Shahid Beheshti University of Medical Sciences and informed consent from the participants (ethics code: IR.SBMU.PHNS.REC.1399.162), data collection was performed via interviews by trained psychologists using a researcher-made checklist to obtain information on three domains.
The first domain included nine demographic variables, including ethnicity (e.g., Fars or others), blood group (A, B, AB, and O), age, living area (urban or rural), education level (elementary school, high school, and university education), marital status (married, unmarried, widow, and divorced), occupation (office employee, worker, housewife, and others), housing status (house owner or tenant), and financial status (independent or dependent).
The second domain involved drug abuse-related variables, including three variables of tobacco product use (yes/no), alcohol use (yes/no), and drug addiction of family members, including the parents and spouse as the most influential people in the lives of Iranian women (yes/no). The third domain included two mental health-related variables, that is, a history of mental health disorders (yes/no) and experience of suicidal thoughts (never, sometimes, usually, and often). The criteria for drug abuse and history of mental disorders were the participants' positive responses to questions concerning “dependence on drugs” (i.e., cigarettes, alcohol, and drugs) and “history of any type of mental health disorders in the life time” during interviews.
3.3. Data Analysis Method
After collecting and cleaning the data, descriptive statistics, including mean (standard deviation [SD]) and median (interquartile range [IQR]), were measured for describing the data, and analytical tests, including chi-square test and independent t-test, were performed for data analysis. Imputation of missing data was also carried out using the expectation-maximization (EM) algorithm (no variable with more than 10% missingness). The EM algorithm is one of the novel methods based on repetition in missing data imputation. It assumes a variable with missing information as a dependent variable, and other variables are added to the model as independent variables. Subsequently, using data pertaining to independent variables, beta coefficients, which are required for estimating the missing data, were calculated.
Generally, the EM algorithm is based on the presumption that the calculated coefficients and values are not the best coefficients and values and that the imputation process is repeated with new coefficients and values until convergence in beta coefficients and imputed values is achieved. The EM algorithm can be used for imputation of qualitative and quantitative variables under the condition that the estimated values for quantitative variables are used without any further processing. On the other hand, the estimated values of qualitative variables can be used after being rounded to the nearest possible value (11).
Due to the sparsity of data on some variables, Firth’s penalized logistic regression was employed for data analysis and modeling. This method is a penalized likelihood regression analysis, which decreases maximum likelihood bias in generalized linear models. It also resolves the separation problem in logistic regression (12). To measure the added diagnostic value, a comparison of the area under the curve (AUC) and net reclassification improvement (NRI) was performed. For this purpose, the AUC of the base model was computed, and the variable of “addiction in the family” was added to the model. Next, the AUC was recalculated, and difference in the AUCs of the base and extended models was considered as the added diagnostic value. Overall, a greater difference in the AUCs represents the higher diagnostic value of the new variable.
Moreover, NRI was measured to study the added value of the new predictor variable in the classification. Individuals were classified into high- and low-risk groups in terms of the incidence of phenomenon under study using the base model. Next, classification was repeated using the extended model. The difference in the correct classification of individuals based on the two models was expressed as the NRI, with accepted values of 0 - 2. Overall, a higher NRI value corresponds to the greater added diagnostic value of the new variable (13). Statistical analysis was performed using Stata version 14.
4. Results
The mean age of women with a history of suicide (case group) was 29.17 ± 10.79 years, and the mean age of women without a history of suicide (control group) was 34.49 ± 11.37 years (P < 0.001). In terms of the living area (urban or rural), 44.4% and 20.9% of the participants in the case and control groups lived in urban areas, whereas 55.6% and 79.1% of the participants in the case and control groups lived in rural areas, respectively (P < 0.001). Similar to the variables of age and living area, significant differences were found between the case and control groups regarding the variables of marital status, education level, occupational status, financial status, history of mental health disorders, alcohol or tobacco use, experience of suicidal thoughts, and drug addiction in the family based on the univariate analysis (Table 1).
| Variables | Case | Control | P-Value |
|---|---|---|---|
| Age, mean ± SD | 29.17 ± 10.79 | 34.49 ± 11.37 | 0.000 |
| living area (urban) | 99 (0.44.4) | 46 (20.9) | 0.000 |
| Ethnicity (Fars) | 175 (79.5) | 171 (77.7) | 0.642 |
| Blood group | 0.138 | ||
| A | 73 (33.2) | 66 (30) | |
| B | 82 (37.3) | 76 (34.5) | |
| AB | 43(19.5) | 39 (17.7) | |
| O | 22 (10) | 39 (17.7) | |
| Marital status | 0.000 | ||
| Married | 128 (47.4) | 116 (52.7) | |
| Never married | 90 (33.3) | 48 (21.8) | |
| Divorced | 41 (15.2) | 18 (8.2) | |
| Widowed | 11 (4.1) | 38 (17.3) | |
| Education level | 0.000 | ||
| Elementary | 41 (15.2) | 32 (14.5) | |
| High school | 161 (59.6) | 38 (17.3) | |
| University | 68 (25.2) | 150 (68.2) | |
| Occupation | 0.000 | ||
| Office employee | 15 (5.6) | 56 (25.5) | |
| Worker | 22 (8.1) | 4 (1.8) | |
| Housewife | 174 (64.4) | 123 (55.9) | |
| Others | 59 (21.9) | 37 (16.8) | |
| Financial status (independent) | 59 (21.9) | 88 (40) | 0.000 |
| Housing status (owner) | 158 (71.8) | 175 (79.5) | 0.059 |
| Mental health disorders (positive) | 19 (7) | 2 (0.9) | 0.005 |
| Using alcoholic drinks (positive) | 29 (10.7) | 1 (0.5) | 0.001 |
| Tobacco use (positive) | 68 (25.2) | 14 (6.4) | 0.000 |
| Experiencing suicidal thoughts | 0.000 | ||
| Never | 31 (11.5) | 175 (79.5) | |
| Sometimes | 60 (22.2) | 22 (10) | |
| Usually | 38 (14.1) | 11 (5) | |
| Often | 141 (52.2) | 12 (5.5) | |
| Addiction in family (positive) | 130 (48.1) | 40 (18.2) | 0.000 |
a Values are expressed as No. (%) unless otherwise indicated.
Based on the results, widows had the lowest risk of committing suicide, whereas married (odds ratio [OR] = 3.86, CI: 1.78 - 8.36), single (OR = 6.51, CI: 2.89 - 14.67), and divorced (OR = 7.27, CI: 2.87 - 18.43) women were more likely to attempt suicide, respectively. Moreover, the lowest risk of suicide was reported in women with academic education, while the highest risk was found in women with secondary education (junior or senior high school education) (OR = 10.09, CI: 6.25 - 16.30). The results revealed that the risk of committing suicide was 3.15 times higher in women with elementary education (below middle school) compared to women with university education (OR = 3.15, CI: 1.78 - 5.60).
Regarding the occupational status, the lowest risk of suicide attempt was observed in female employees. Housewives (OR = 5.35, CI: 2.74 - 10.44), women with other occupations (OR = 6.43, CI: 3.03 - 13.67), and workers (OR = 18.67, CI: 5.29 - 65.84) were more likely to commit suicide, respectively. Also, the risk of committing suicide was lower in women who were financially independent compared to financially-dependent women (OR = 2.33, CI: 1.53 - 3.53).
According to the present findings, alcohol consumption was significantly different between the case and control groups. In other words, the probability of alcohol consumption in the case group was more than 18 times higher than the control group (OR = 18.24, CI: 3.47 - 95.93). There was also a significant difference regarding smoking between the case and control groups, and the odds of smoking was more than five times higher in the case group (OR = 5.02, CI: 2.70 - 9.34).
In terms of mental health disorders, there was a significant difference between individuals with and without suicide attempts. The odds of having a history of mental health disorders was 6.59 times higher in the case group than the control group (OR = 6.59, CI: 1.71 - 25.41). The experience of suicidal thoughts was also significantly different between the case and control groups. Women with no experience of suicidal thoughts had the lowest risk of attempting suicide; in other words, as suicidal ideation increased, the risk of attempting suicide increased, as well (OR = 4.11, CI: 3.23 - 5.23).
Addiction in the family (i.e., father, mother, and husband) was significantly different between the case and control groups, and the odds of addiction in the family was more than four times higher in the case group than the control group (OR = 4.26, CI: 2.76 - 6.57). Based on the univariate analysis, the distribution of ethnicity (P = 0.642), blood group (P = 0.138), and housing status (P = 0.059) was not significantly different between the two groups. On the other hand, in the multivariate analysis, the variable of blood group remained in the model, and O blood type was found to be a protective factor for suicide attempts (OR = 0.11, CI: 0.038 - 0.34). Moreover, the results of multivariate analysis showed that variables of education level, living area, smoking, suicidal thoughts, and addiction in the family were the most important risk factors for suicide attempts in women (Table 2).
| Variables | Unadjusted | Basic Model | Extended Model | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Blood group | ||||||
| A | 1 | - | 1 | - | 1 | - |
| B | 0.975 | 0.62 - 1.54 | 0.73 | 0.34 - 1.52 | 0.62 | 0.28 - 1.34 |
| AB | 0.997 | 0.57 - 1.72 | 0.56 | 0.22 - 1.42 | 0.05 | 0.19 - 1.30 |
| O | 0.51* | 0.28 - 0.95 | 0.12* | 0.04 - 0.34 | 0.13* | 0.04 - 0.37 |
| Education level | ||||||
| College | 1 | - | 1 | - | 1 | - |
| High school | 9.94* | 6.17 - 16.01 | 3.06* | 1.55 - 6.06 | 3.31* | 1.64 - 6.70 |
| Elementary | 3.13* | 1.78 - 5.54 | 1.40 | 0.57 - 3.47 | 1.23 | 0.47 - 3.23 |
| Living area (urban) | 3.09* | 2.03 - 4.71 | 4.44* | 2.15 - 9.16 | 5.17* | 2.41 - 11.09 |
| Tobacco use (positive) | 5.02* | 2.70 - 9.34 | 8.99* | 3.56 - 22.71 | 7.94* | 3.05 - 20.66 |
| Suicidal thoughts experience | ||||||
| Never | 1 | 1 | 1 | |||
| Sometimes | 14.83* | 7.74 - 28.41 | 17.82* | 8.05 - 39.45 | 19.84* | 8.65 - 45.52 |
| Usually | 16.45* | 7.37 - 36.77 | 21.32* | 7.81 - 58.19 | 16.88* | 6.16 - 46.23 |
| Often | 66.34* | 32.44 - 135.67 | 128.22* | 47.75 - 344.31 | 107.52* | 38.51 - 300.17 |
| Addiction in family (positive) | 4.26* | 2.76 - 6.57 | - | - | 3.72* | 1.83 - 7.56 |
a Basic Model: Hosmer and Lemeshow Test = 0.217, Nagelkerke R Square = 0.621- Extended Model: Hosmer and Lemeshow Test = 0.463, Nagelkerke R Square = 0.732
b * P-value < 0.05
The variables of age, marital status, occupation, financial status, housing status, History of mental health disorders and Alcohol use had no significant relationship with women's suicide attempts and were excluded from the model. (P-value < 0.05)
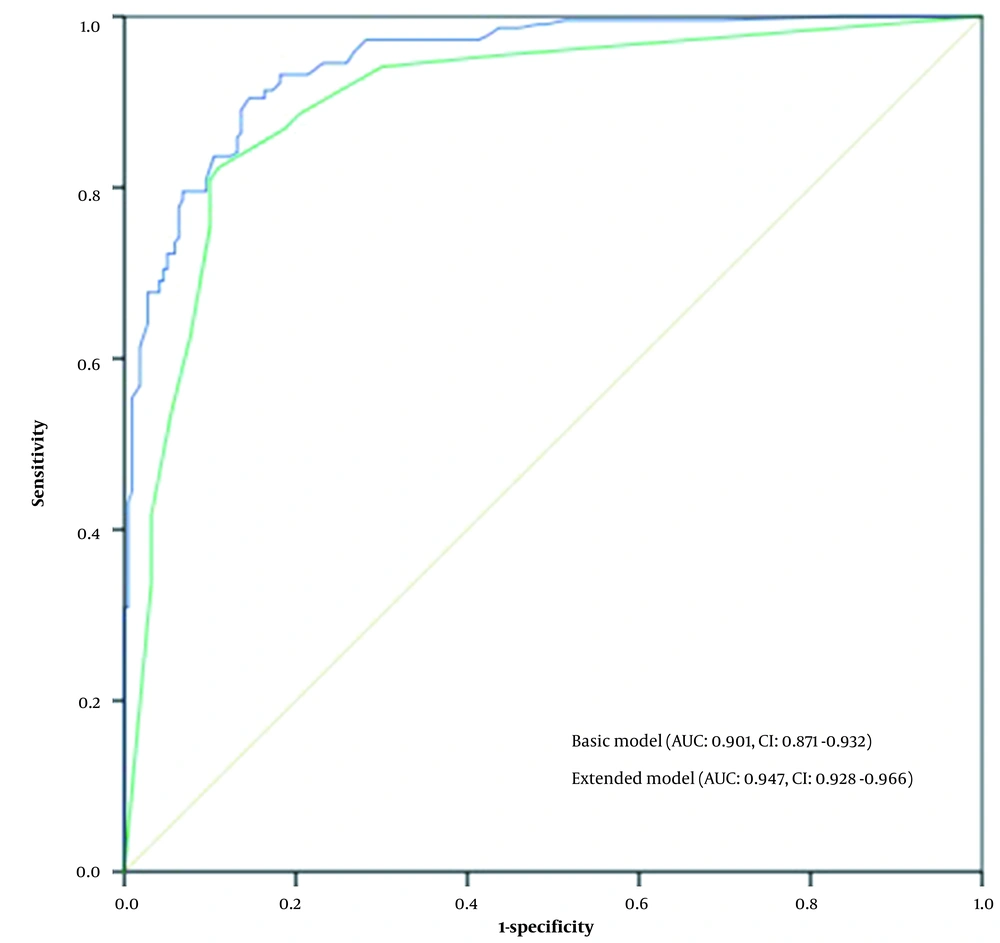
The added diagnostic value of the variable of “addiction in the family” was evaluated by comparing the AUC and also calculating the NRI. As shown in Figure 1, by adding this variable to the basic model, which included the living area, marital status, education level, smoking, and suicidal thoughts, the AUC of the extended model increased by 4.6% (P = 0.0005). By adding the variable of “addiction in the family” to the basic model, the ability of the extended model to correctly classify individuals into high- and low-risk suicide groups significantly improved by 0.61 (NRI = 0.61, P < 0001).
A comparison of the area under ROC curve of basic model with variables blood group, education level, living area, tobacco use, and suicidal thoughts experience and Extended model with variable blood group, education level, living area, tobacco use, suicidal thoughts experience, and addiction in family.
5. Discussion
This study was carried out to investigate the effect of drug addiction in the family on the suicide attempts of women while considering the role of other risk factors and demographic characteristics. The results revealed that addiction of the parents or husband is an effective factor in female suicide attempts, independent of other risk factors and demographic characteristics. The adjusted OR for the variable "addiction in the family" was 3.72, which clearly confirms the importance and effectiveness of this variable in women's suicide attempts.
According to our literature review, no study has evaluated the effect of family addiction on the general female population. However, in some demographic subgroups, several studies reported consistent results with the present study. In this regard, Dragisic et al. studied a drug addict population and reported that drug addiction was significantly more common in the families of addicts who attempted suicide compared to the families of addicts with no suicide attempts (10). Additionally, Ahmadi et al. found that self-immolation in married individuals had a significant relationship with drug addiction in the spouse, and in unmarried individuals, it had a significant relationship with the parents’ drug addiction (14). On the other hand, Rahmani et al. reported that drug addiction of the spouse did not increase the risk of self-immolation in the partner (15).
Several studies have examined the impact of alcohol abuse in the family on the suicide attempts of women. Pengpid and Peltzer reported that women with a family history of alcohol dependence/abuse were more likely to develop suicidal behaviors (e.g., suicidal thoughts, suicidal ideation, and suicide attempts) (16). Mroczkowska-Juchkiewicz (cited in Zygo et al.) also reported that the youth suicide attempt was rooted in familial problems and parental drug addiction (17). Additionally, Park et al. found that the odds of drug addiction in mothers, grandfathers, brothers, and sisters of females who committed suicide was significantly higher than the controls (18).
Addiction in the family can increase women's risk of suicide in several ways. Some studies have indicated that addiction in the family increases the risk of domestic violence (19). The results of some studies also indicated the role of domestic violence in increasing the risk of suicide in women (20). Therefore, it can be concluded that family drug addiction has effect on increasing the risk of suicide in women by increasing the risk of domestic violence. Another variable that has been shown to affect suicide in women is family breakdown (21). Some studies have reported that addiction in the family can cause family breakdown. It can be concluded that drug addiction in the family can also affect suicide attempts in women through family issues caused by drug abuse (22-24). Besides, addiction of family members may lead to lower living standards, increased life dissatisfaction, and increased social frustration, which can ultimately increase the risk of suicide in women.
As shown in Table 2, in agreement with the results of previous research (7, 10, 14, 17, 21, 25-28), the present findings showed that the variables of blood group, education level, living area, history of mental health disorders, smoking, and experience of suicidal thoughts had significant relationships with suicide attempts in women. The regression model predicting suicide attempts had a good predictive value in the population (Figure 1).
To evaluate the significance of a variable, it is important to determine whether its addition to the predictive model can improve the model performance (29). Considering the added value of “addiction in the family” in the model, this variable was regarded as an influential factor in the suicide attempts of women based on the comparison of AUCs and also calculation of NRI, as it could increase the power of the predictive model for suicide attempts in women. Therefore, addiction in the family can be introduced as a potential factor in suicide prediction models.
The limitation of this study was the sparsity of data on some variables. However, attempts were made to reduce the impact of this factor on the results as much as possible by using appropriate statistical methods.
5.1. Conclusions
Drug addiction in first-degree relatives (i.e., father, mother, and spouse) is an effective factor in increasing the risk of suicide in women, regardless of other influential factors. Therefore, suicide prevention programs need to be established for screening and detecting this problem in women. Overall, suicide in women can be considered an irreversible complication of drug addiction in drug prevention programs because it's predictable and preventable.