1. Background
Health literacy (HL) is the degree to which individuals can obtain, process, and understand basic health information and services (1). It affects an individual’s capacities to interact with healthcare providers, engage in self-care, make informed health decisions, access health information, and understand health messages in the public domain (2). Inadequate HL competencies lead to unhealthy choices, high-risk behavior, poorer health, less self-management, and more hospitalization. Individuals with inadequate HL competencies are believed to waste human and financial resources in the health system (3). The concept of HL has also been discussed in public health. In addition to the articles reporting the correlation of HL with decreased treatment adherence, poor knowledge of health, poor adherence to self-care, and poor treatment outcomes, numerous studies have shown that HL is associated with health-promoting behaviors (4) such as participation in screening programs or using preventive services (5, 6). HL enables people to cope with chronic conditions and have active aging (7).
Health literacy is influenced by several factors. Evidence, for example, has shown that rurality alone does not describe rural-urban HL variations and that the social determinants play important roles in this regard (8). Media literacy is an important factor responsible for the HL, and an increase in media literacy may also increase the HL level (9). Furthermore, some studies have demonstrated that race and income (10), social support, food insecurity, and housing across diverse contexts (11) may significantly affect the HL.
External factors, including interpersonal relationships and socio-cultural conditions, have been reported to influence the HL considerably (12). Socioeconomic status (SES), especially educational attainment, contributes to HL levels which, in turn, contribute to the quality of life, health status, health behaviors, and use of healthcare services (13).
Several studies have examined the differences in the HL levels across different settings. European HL survey has indicated that at least 1 out of 10 participants (12.4%) suffers from inadequate HL and that the differences among member states are considerable (e.g., only 1.8% of the participants suffered inadequate HL in the Netherlands, whereas 26.9% of the participants suffered it in Bulgaria; almost 48% out of the total sample suffered inadequate HL) (14). The HL levels have been the focus of several studies in Islamic Republic of Iran. A nationwide population-based survey in 2015 showed that 18% of Iranian participants enjoyed adequate HL, while 45.7% suffered inadequate HL, and 36.3% had moderate HL (15). No study had investigated the HL in Qom province since 2015.
2. Objectives
The present study was conducted to examine the HL and the factors associated with it in Qom province in 2020, as well as to compare its results with those from the National Survey on HL.
3. Methods
This cross-sectional survey was conducted in November and December 2020 to examine adult people in Qom City, located in the center of Iran. Due to the limitations imposed to deal with the coronavirus pandemic, the “Porsline” platform was employed for recruiting the required participants. “Porsline” is an online platform that helps researchers create online questionnaires and share them with individuals interested in participating in online research studies around the country. An online questionnaire was distributed using social media (Telegram, WhatsApp, and Eita) and small message service (SMS) in order to obtain the most heterogeneous sample possible. HL was stratified into three levels adequate, moderate, and inadequate based on the National Survey on HL (15).
The following formula was used at 95% confidence intervals (z = 1.98), margin of error (d) of 0.05, and a prevalence (p) of 54.3%. In this formula, the HL prevalence (adequate and moderate levels) was determined based on a relevant study on health literacy conducted in Iran (15). Therefore, the sample size was calculated to be 477. Since the study was conducted online, the sample size was initially increased to 500 and then decreased to 488 participants in order to reduce the error of randomization. Finally, the questionnaire was completed by 488 participants, and the response rate was 44.3%.
As already mentioned, the questionnaire was sent to the participants using different methods. First, the link was sent to the residents of eight districts of the city through SMS sending systems, capable of sending SMS based on districts, in order to ensure the uniformity of sampling in the whole city. The social media accounts of the people from these regions, all available in the health service centers of these regions, were also used when sharing the link of the questionnaire with them.
Participants were 18 - 64 years old, residents of Qom, and able to use social media and web-based platforms. The questionnaire, which was a self-administered one, took 10 - 15 minutes to fill.
Data were collected using the validated Iranian Health Literacy Questionnaire (IHLQ) (16). This questionnaire has 53 items on nine domains, including health information access (5 items), health information use (6 items), reading skills (5 items), comprehension skills (8 items), interpretation/judgment skills (6 items), communication and decision-making skills (8 items), health knowledge (5 items), individual empowerment (6 items), and social empowerment (4 items). In the study by Haghdoost et al., Cronbach’s alpha was > 0.7 (0.71 - 0.96) (16).
In order to calculate the total score of HL, the score of each domain was determined, and each domain was assessed according to the number of its items. The average score of the HL was calculated by adding the scores of domains and dividing it by the number of items from each domain. Scores were then categorized into three groups of inadequate (< 10), moderate (10 - 14), and adequate (> 14). Independent variables in this study were age, sex, education level, residence, and occupation.
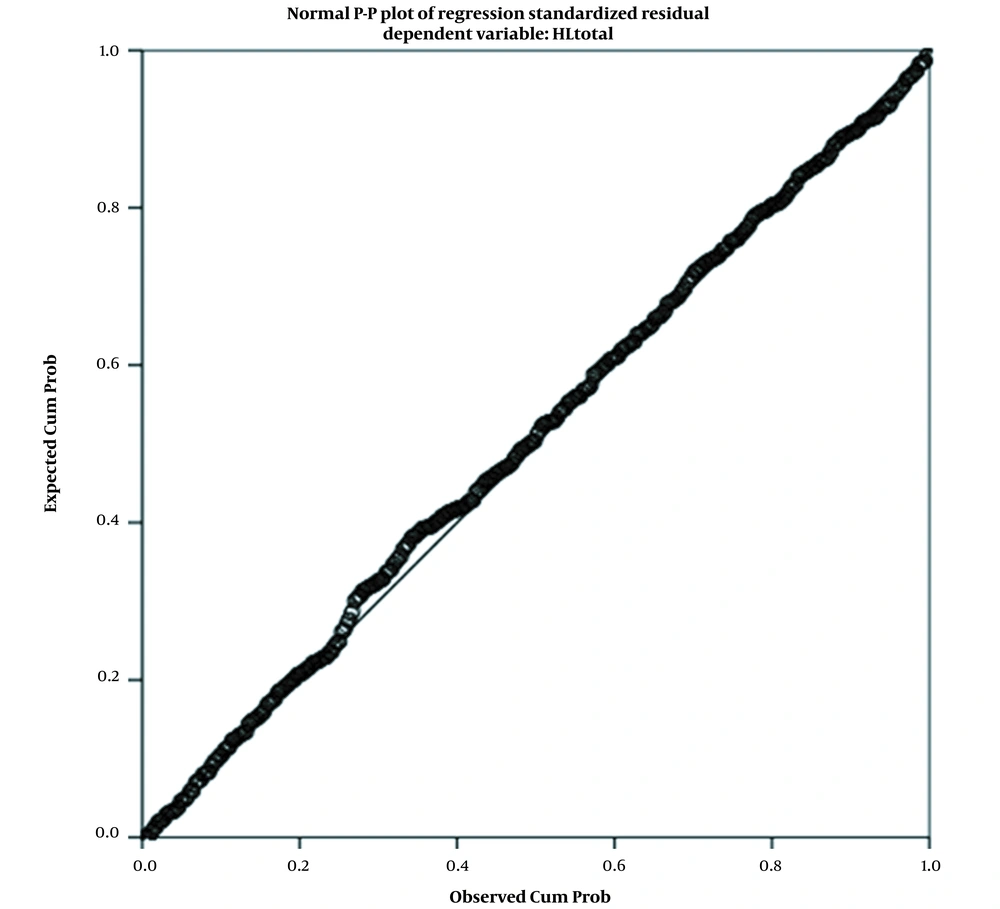
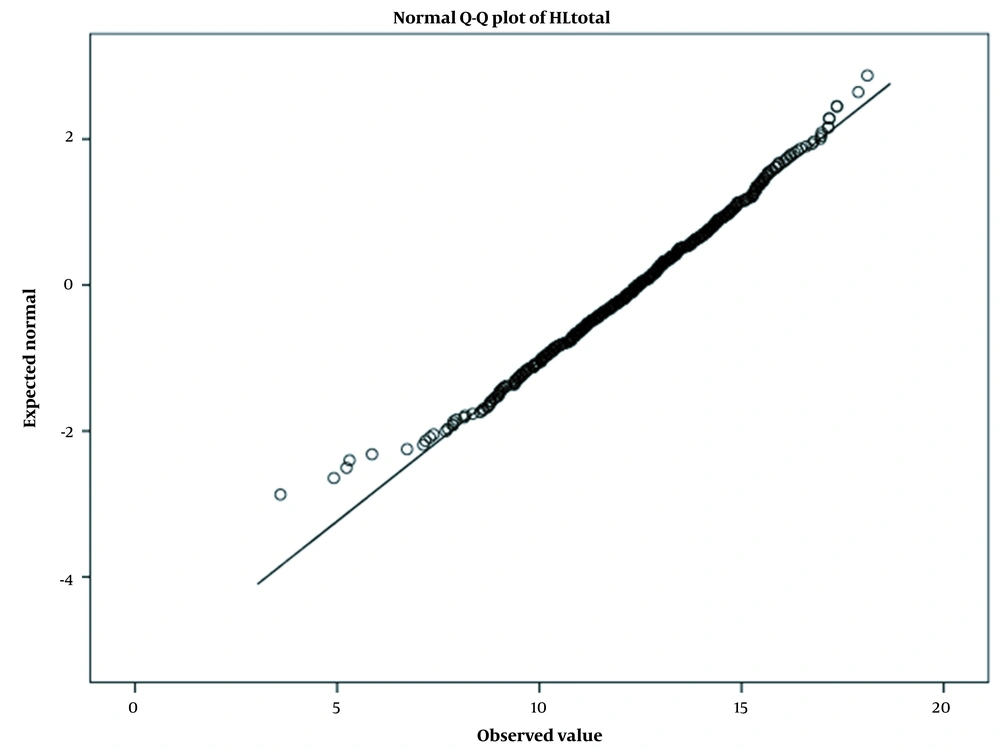
Before using the linear regression model, its assumptions (normality of residual and homogeneity of error variance) were first checked.
In order to examine the distribution normality of the model’s residuals, the normality of the residuals was evaluated using both the plot and the Kolmogorov-Smirnov statistical test, and it was found that the model’s residuals were normally distributed.
Taking into account the P-value calculated by the K-S test, it was found that the residuals were normally distributed (Table 1).
| Kolmogorov-Smirnov (K-S) | ||
|---|---|---|
| Statistics | P-Value | |
| Residual | 0.039 | 0.07 |
Kolmogorov-Smirnov Test to Evaluate the Normality of Residuals’ Distribution
In addition to the statistical test, the P-P and Q-Q plots were also used to confirm the normality of the residuals (Figures 1 and 2).
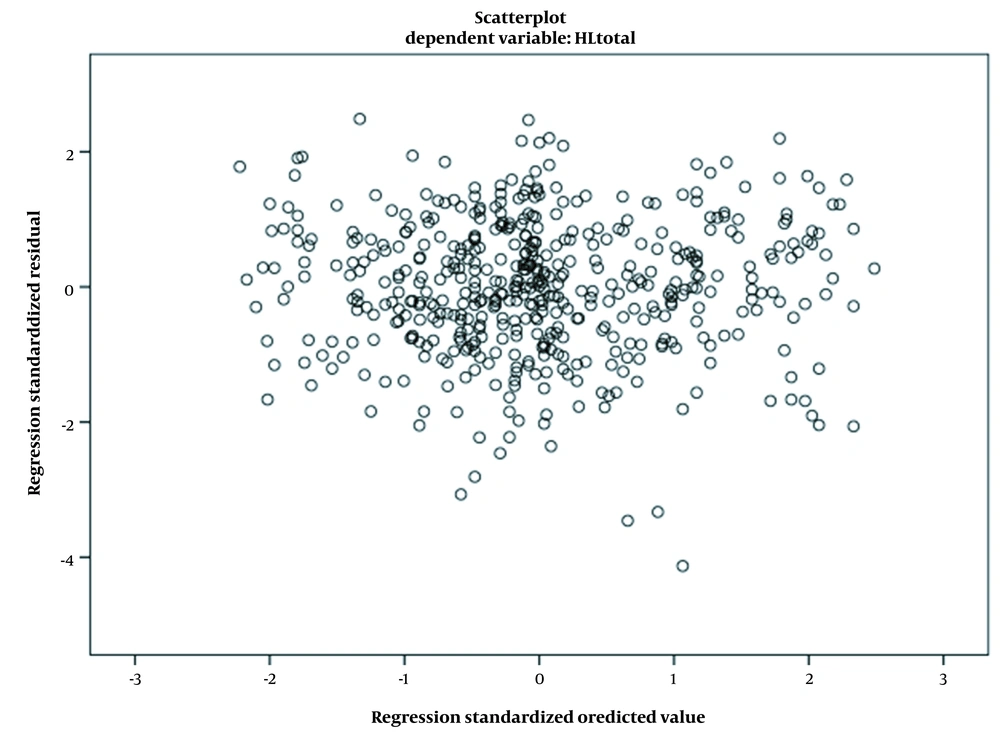
In order to examine the homogeneity of error variance, the Scatterplot of the residual was drawn, and it was found that the variance of the errors was stable (Figure 3).
Data analysis was performed using SPSS version 22, and the linear regression model was adopted to determine the factors involved in HL. P-values < 5% were considered statistically significant. The effect of independent variables on dependent variables was measured as bivariate and multivariable. Categorical variables were introduced to the multifactorial model variables using a series of indicators (e.g., education had four categories). One category of education was selected as the reference, and three binary variables were created, which took values of 0 and 1.
4. Results
The mean age of the participants was 38.72 ± 11.11 years; 34.6 of the participants (169) were males, 65.4 (319) were females, 62.9% of them (307) had university degrees, and 31.1% of them (152) had permanent jobs.
Our study results showed that inadequate, moderate, and adequate levels of HL among the participants were 14.3%, 60.5%, and 25.2%, respectively.
Accessibility of the participants to health care providers, the internet, and mass media as resources of health information were 53.1%, 90.2%, and 79.5%, respectively.
As for the HL domains, the communication/decision-making skills of the participants had the highest percentage (56.8%) inadequate level, health knowledge of them had the highest percentage (51.0%) at a moderate level, and individual empowerment of them had the highest percentage (52.9%) in inadequate level (Table 2).
| Domain | Adequate | Moderate | Inadequate |
|---|---|---|---|
| Health information access | 151 (30.9) | 121(24.8) | 216 (44.3) |
| Health information use (previous month) | 115 (23.6) | 229 (46.9) | 144 (29.5) |
| Reading skills | 223 (45.7) | 194 (39.8) | 71 (14.5) |
| Comprehension skills | 238 (48.8) | 170 (34.8) | 80 (16.4) |
| Interpretation/judgment skills | 234 (48.0) | 160 (32.8) | 94 (19.3) |
| Communication/decision-making skills | 277 (56.8) | 169 (34.6) | 42 (8.6) |
| Health knowledge | 78 (16.0) | 249 (51.0) | 161 (33.0) |
| Individual empowerment | 123 (25.2) | 107 (21.9) | 258 (52.9) |
| Social empowerment | 153 (31.4) | 143 (29.3) | 192 (39.3) |
Distribution of Health Literacy Domain Scores Among Adults in Qom a
The generalized linear regression model used for examining the relationship between HL and independent variables revealed that gender and level of education were significantly associated with HL at a 95% confidence interval. Age was only slightly associated with HL at the 90% confidence interval (Table 3).
| Variables | Bivariate Linear Regression | Multiple Linear Regression | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | t | 95% CI for β | P-Value | β | SE | t | 95% CI for β | P-Value | |
| Age | -0.01 | 0.009 | -1.58 | -0.03, 0.004 | 0.11 | -0.02 | 0.01 | -1.84 | -0.04, 0.001 | 0.06 |
| Gender | ||||||||||
| Female | 0 | 0 | ||||||||
| Male | -0.23 | 0.21 | -1.05 | -0.20, 0.65 | 0.29 | -0.53 | 0.24 | -2.18 | -0.99, -0.06 | 0.03 |
| Education | ||||||||||
| Illiterate | 0 | 0 | ||||||||
| Elementary and secondary | 4.16 | 1.28 | 3.24 | 1.63, 6.68 | 0.001 | 4.08 | 1.30 | 3.09 | 1.52, 6.63 | 0.002 |
| High school | 4.50 | 1.26 | 3.57 | 2.02, 6.98 | < 0.001 | 4.22 | 1.28 | 3.26 | 1.71, 6.72 | 0.001 |
| College/university | 5.70 | 1.25 | 4.55 | 3.24, 8.17 | < 0.001 | 5.16 | 1.27 | 4.00 | 2.66, 7.66 | < 0.001 |
| Job | ||||||||||
| Student (school) | 0 | 0 | ||||||||
| Student (college) | 1.17 | 0.64 | 1.81 | -0.09, 2.42 | 0.07 | 0.47 | 0.68 | 0.68 | -0.86, 1.79 | 0.49 |
| Housewife | 0.43 | 0.59 | 0.72 | -0.72, 1.57 | 0.47 | 0.23 | 0.67 | 0.33 | -1.10, 1.56 | 0.73 |
| Retired | 1.08 | 0.70 | 1.54 | -0.28, 2.43 | 0.12 | 1.15 | 0.86 | 1.33 | -0.53, 2.83 | 0.18 |
| Unemployed | 0.43 | 0.70 | 0.61 | -0.94, 1.80 | 0.54 | 0.71 | 0.74 | 0.95 | -0.75, 2.17 | 0.34 |
| Permanent employee | 1.53 | 0.59 | 2.60 | 0.38, 2.68 | 0.01 | 1.12 | 0.69 | 1.60 | -0.24, 2.49 | 0.10 |
| Temporary employee | 0.93 | 0.63 | 1.48 | 0.29, 2.16 | 0.14 | 0.54 | 0.69 | 0.76 | -0.83, 1.90 | 0.44 |
| Model summary | ||||||||||
| F | 6.65 | |||||||||
| R | 0.78 | |||||||||
| R2 | 0.61 | |||||||||
| Adjusted R2 | 0.60 | |||||||||
Association Between Health Literacy and Independent Variables
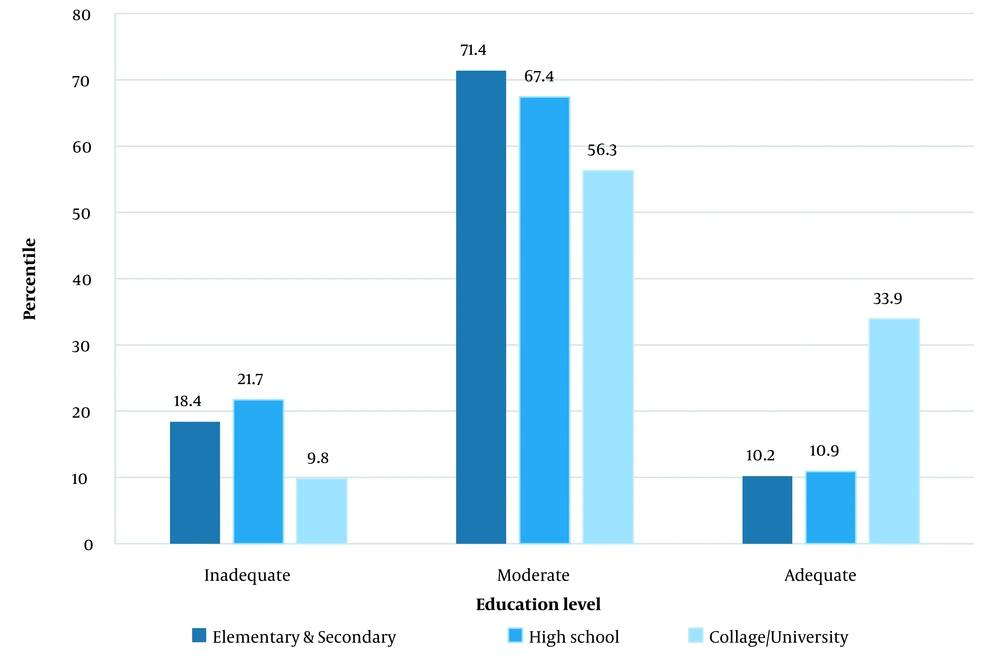
Using the Spearman coefficient of correlation in ordinal by the ordinal method indicated that there was a significant relationship between HL and education level, so the HL level increased as the education level increased (coefficient = 0.31) (P < 0.001) (Figure 4).
5. Discussion
This study assessed the HL levels of the individuals from Qom based on IHLQ in an online context. Nine main categories were explored to determine the different dimensions of HL. This study was conducted using the IHLQ. These questionnaire components were developed based on a health promotion approach and, to some extent, had the properties that made the questionnaire an appropriate instrument for evaluating the HL.
The relationships between HL levels and some participants’ characteristics were investigated. Overall, more than half of the participants enjoyed moderate HL levels. In this study, compared to the study by Haghdoost et al. (15), a considerable increase was recorded for adequate HL levels, while a decrease was documented for inadequate HL. This finding may have been attributed to some factors, such as the study sample size affected by the COVID-19 pandemic, the online recruitment method, and the vast public health education provided during the COVID-19 epidemic period. Due to the application of an online platform to recruit the participants, illiterate people were excluded from the study, which may also have affected the results.
The participants in this study faced HL challenges in the “individual empowerment” and “health information access” domains, and the “health knowledge” domain was moderate in HL levels. While “individual empowerment” consists of constructs such as the ability to read medical forms, transfer content to others, and take care of one’s health in different situations, an inadequate level of HL in this domain suggests that the participants are likely unable to use their information in practice and need to adopt a more effective method for learning. Considering the development of and the good access to social media and communication in today’s community, the inadequate level of HL in the “health information access” domain was considerable, which may have indicated that health was not an important priority for the people at the time of our study. This finding was consistent with that reported by Yari et al. (17).
According to our results, gender had a significant relationship with HL, so the female participants enjoyed higher HL levels, which was in line with the findings from several other studies, such as the studies by Kohan et al. (18) and Sorensen et al. (14). This may have been due to the fact that women use health information media more frequently, have greater rates of follow-up, pay more attention to health problems, and have more frequent contact with healthcare system workers. Furthermore, most women in this study were housewives who, in general, have easier access to different mass media. However, some studies have reported no relationship between inadequate HL and gender (19).
Our study results also revealed that HL had a significant relationship with higher levels of education, which was consistent with the results from previous studies (14, 20, 21). This predictable result highlighted the need for a plan aimed at increasing the quantity and quality of public education in order to improve HL in the community and, consequently, to reduce the risk of involvement in unhealthy behaviors.
This study indicated that individuals with permanent jobs enjoyed higher levels of HL, which was in agreement with the finding of Haghdoost et al. (15). This result may have been attributed to the fact that individuals with permanent jobs have easier access to health information in their workplace and to health care services. The need for higher education in order to obtain a permanent job and higher socioeconomic status may also have been associated with higher HL.
In our study, no significant relationship was found between age and HL. However, the significance of the age variable may have been set at a 95% confidence level so that HL levels showed a little decrease with older age and approximately HL decreases by 0.02 points per year, which was in line with the findings from studies by Yari et al. (17) and Sorensen et al. (14).
5.1. Conclusions
In sum, the majority of the participants enjoyed moderate and high HL levels. Due to the exclusion of illiterate individuals from this study, however, HL remained a challenge to adopting the health behaviors. Therefore, it was recommended that the policy-makers should improve HL by promoting education for the population, providing them with permanent job opportunities, improving individual empowerment, providing them with health information access, facilitating health information application, and helping them improve their interpretation/judgment skills. Furthermore, it was suggested that an effective training program should be developed and conducted for those with lower education levels and older people. To address the lower HL among male participants, it was found important to develop immediate plans aimed at increasing their HL level. Given our study limitations, such as the application of an online data-gathering method, it was suggested that future HL studies should be carried out in Qom and other cities of Iran in order to eliminate the ambiguities surrounding the field of HL and its determinants.
5.2. Limitations
This study faced some limitations. First, some participants in the sampling may have been lost due to the adoption of internet-based method to collect the data, which, in turn, may have led to bias in sampling and limited the study’s generalizability. Second, the bias of social desirability may not have been ruled out based on the self-reported data; however, the sufficient sample size may have increased the reliability of our findings. Third, individuals residing in urban regions and those with high levels of education were over-represented in the study sample. Greater participation of individuals from rural regions or of those with low educational levels may have affected the HL levels. Fourth, some Iranians did not have a smartphone to participate in the research, which was a selection bias.
5.3. Suggestions
Individuals with low HL suffer from poorer health conditions and do not use preventive care adequately. They are more likely to be hospitalized and suffer serious health consequences. Lower health literacy is associated with higher mortality rates and is likely responsible for additional costs in healthcare. Moreover, adults with low HL are less likely to adhere prescribed treatment and self-care and make more treatment and medication errors (22-25).
Rates of inadequate HL are disproportionately higher among those with lower socioeconomic status and limited education; therefore, it is recommended that the policymakers should:
Invest more in research on health interventions in diverse settings to improve HL;
Improve health literacy by creating centers to promote research and increase evidence-based health knowledge;
Reconsider the existing policies and related activities to improve HL policies for the benefit of patients, individuals, and communities;
Expand the scope of the fields of activity required for the overall HL Policy to include environmental, workplace, media, and digital health at all levels of society;
Collect ample evidence based on the effectiveness of HL, and ensure that the policies address the specific needs of regional contexts;
Support quantitative and qualitative research in order to produce conclusive evidence confirming the effectiveness of HL for all levels of the community;
Incorporate the facilitators of successful implementation (e.g., intersectoral collaboration, political leadership, and strategies to overcome cultural barriers) into the health literacy policy;
Provide necessary resources to overcome the cultural and social barriers to the development of health literacy;
Integrate HL into education and training programs for healthcare professionals.