1. Background
Osteoarthritis (OA) of the knee requires lifetime care since it is a degenerative, age-related, and progressive illness (1, 2). Knee OA is one of the most frequent causes of knee discomfort globally. Repetitive mechanical loading and stress that result in inflammation inside the knee joint, articular cartilage breakdown, and chondrocyte loss are the leading causes of osteoarthritic knee pain (3). Pain, stiffness, and decreased range of motion in the affected knee are hallmarks of knee OA. They may worsen with time, significantly impacting the patient’s daily activities and overall quality of life (4, 5). Knee OA management has evolved from pharmacological administration alone to the inclusion of therapeutic exercise with or without physical modalities, such as electrical stimulation, thermal agents, therapeutic ultrasound, low-level laser therapy (LLLT), and high-intensity laser therapy (HILT) (6-10). Moreover, ozone and platelet-rich plasma have been reported to be effective for pain reduction and function improvement in knee OA (11).
Throughout the past decade, HILT has been developed to treat a wide variety of musculoskeletal conditions and has gained popularity (12). High-intensity laser therapy is a potent physical technique that causes no pain and has been reported to have significant advantages for analgesic, bio-stimulating, and anti-edema effects (13). Evidence suggests that high-intensity laser radiation causes photo-thermal, photochemical, and photo-mechanical effects (14, 15). Prior research has demonstrated the advantages of HILT in reducing pain, improving range of motion, and enhancing functional outcomes in individuals with knee OA compared to control groups (16-18). However, a standardized treatment approach for HILT in patients with knee OA is still lacking, with varying and often high numbers of treatment sessions which can negatively impact patient compliance.
Furthermore, prior systematic reviews and meta-analyses have not provided definitive findings on the effectiveness of HILT in knee OA, thus suggesting the need for additional research in this field (19, 20).
2. Objectives
Due to the small number of studies and lack of a standard protocol for HILT on the knee, the current study aimed to assess the effect of HILT on pain and function in patients with knee OA. The novelty of our study compared to other studies included fewer sessions (lower cost), the use of analgesic protocol alone, and laser on the medial side of the knee.
3. Methods
3.1. Trial Design
This parallel randomized controlled trial included patients with knee OA referred to Amin Hospital, affiliated with Isfahan University of Medical Sciences, Iran, from April 19 to August 30, 2022. The inclusion criteria were age 40 - 70 years and knee osteoarthritis grade II or III based on the Kellgren and Lawrence classification system on X-ray. The exclusion criteria were rheumatic diseases, diabetes mellitus, systemic inflammatory diseases, pes anserine bursitis, intra-articular injection of hyaluronic acid or glucosamine compounds for the treatment of knee OA within the past six months, injection of corticosteroids in the past six weeks, tumoral malignancies, and any contraindication to laser therapy (acute infection, pregnancy, and chronic skin diseases) (18, 21). Also, patients with predominantly lateral knee involvement were excluded due to HILT being performed on the medial aspect of the knee.
The study received ethics approval from the Ethics Committee of Isfahan University of Medical Sciences under the ethics code: IR.MUI.MED.REC.1400.799 and complies with the statements of the Declaration of Helsinki. Written informed consent was obtained from the patients. The trial has also been registered prospectively at the Iranian Registry of Clinical Trials (IRCT), IRCT20220214054022N1.
3.2. Interventions
Patients in both groups learned isometric exercises targeting the quadriceps muscle in three sets of ten repetitions a day for two weeks. Moreover, they received 15 mg meloxicam daily for two weeks and applied Rahamin ointment (Harpagophytum procumbens + Boswellia frereana + Olea europaea + Vitis vinifera + Oenothera biennis, Raha pharmaceutical Co., Iran) topically on the affected knee three times a day for two weeks. In addition to the above-mentioned treatments, patients in the HILT group received high-intensity laser irradiation (high-intensity laser device, LUMIX® C.P.S.®, 6 watts, Fisioline®, Italy) three times a week for two weeks (a total of six sessions). After the patient entered the laser room, special glasses to protect the eyes were provided to the patient and the attending physician. The patient was placed in a supine position, and the affected knee was placed in a non-bent position. Laser treatment was applied with a wavelength of 1064 nm, power of 2 W, and an analgesic protocol with an energy of 20 J/cm2 for an area of 25 cm2 (a total of 500 J) on the medial surface of the knee for four minutes with the probe perpendicular to the joint line.
3.3. Outcomes
The primary outcome was pain assessed using Visual Analog Scale (VAS) by the patients, with “0” indicating no pain and “10” indicating worse pain. The secondary outcome was the Western Ontario and McMaster Universities Osteoarthritis index (WOMAC) and its subscales (pain, stiffness, and physical function). The Persian version of WOMAC was used in the current study, with a Cronbach’s alpha of 0.811, an intra-class correlation coefficient of 0.80, and an acceptable correlation with Medical Outcomes Study 20-Item Short Form (MOS-SF-20) (22). Outcomes were evaluated at baseline (before treatment), immediately, and three months after the last treatment session.
3.4. Sample Size
The minimum sample size was calculated as at least 23 in each group based on a type I error of 0.05, power of 90%, and post-intervention VAS pain score of 3.79 ± 0.54 in the HILT group and 4.28 ± 0.56 in the physical therapy group of the study by Nazari et al. (effect size = 0.89) (18).
3.5. Randomization
First, the general characteristics of the patients, including age, sex, body mass index (BMI), and the side affected by OA, were recorded. Then, they were randomized into two groups using block randomization (block size = 2).
3.6. Blinding
Due to the nature of interventions, patients and caregivers could not be blinded.
3.7. Statistical Methods
We used mean and standard deviation to describe continuous variables and frequency and percentage to describe categorical variables. According to the central limit theorem, since the sample size was 26 in each group, we utilized the ANOVA/ANCOVA test to compare outcomes between groups at different time points, with sex as a factor and baseline values and age as covariances. The standardized mean difference (SMD) was calculated using Cohen’s d for adjusted means. Standardized mean difference interpretation was as follows: ≤ 0.19, trivial; 0.20 - 0.49, small effect; 0.50 - 0.79, medium effect; and ≥ 0.80, large effect. All data were analyzed using Stata software (version 14.2). P-values < 0.05 were regarded as statistically significant.
4. Results
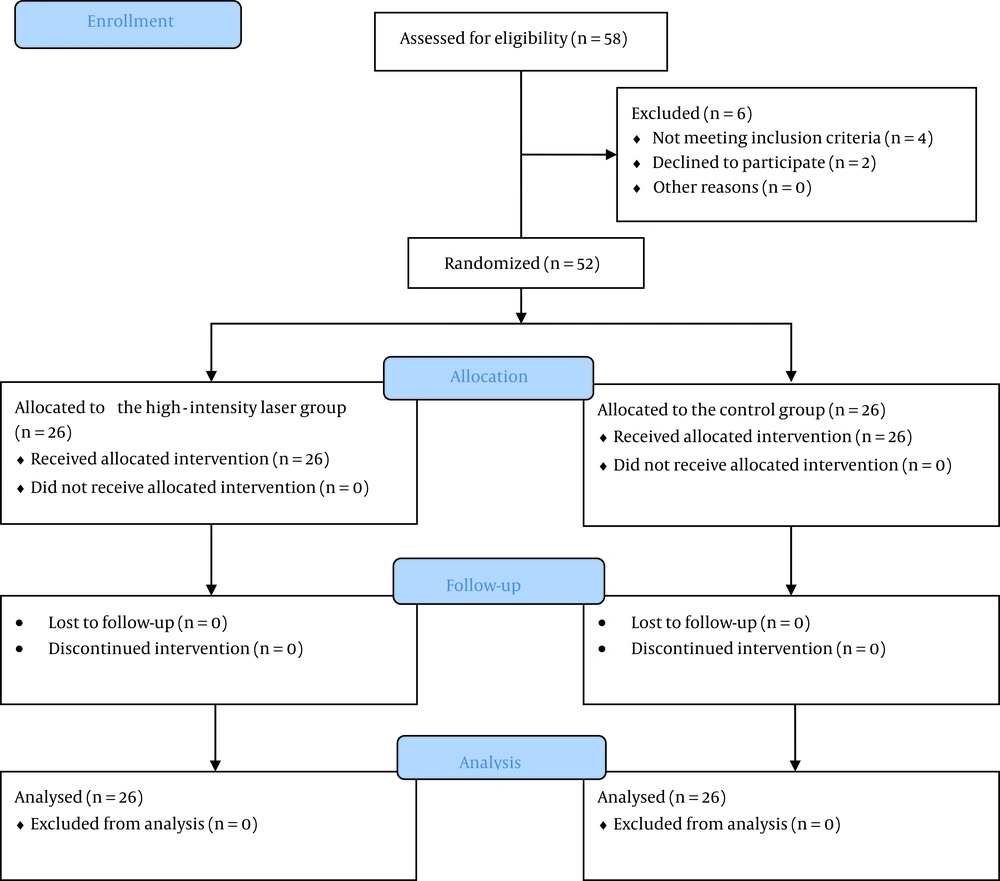
Initially, 58 patients were evaluated for eligibility; two declined to participate, and four did not meet the inclusion criteria (Figure 1). The general characteristics of the remaining 52 patients are presented in Table 1. The mean age of patients was 52.27 ± 8.30 years in the HILT group and 57.08 ± 8.06 years in the control group. Moreover, four patients (15.4%) in the HILT group and seven (26.9%) in the control group were males.
| Variables | Control (n = 26) | HILT (n = 26) |
|---|---|---|
| Age (y) | 57.08 ± 8.06 | 52.27 ± 8.30 |
| Sex | ||
| Male | 7 (26.9) | 4 (15.4) |
| Female | 19 (73.1) | 22 (84.6) |
| BMI (kg/m2) | 28.55 ± 3.79) | 28.59 ± 3.41 |
| The side affected by OA | ||
| Right knee | 13 (50.0) | 13 (50.0) |
| Left knee | 13 (50.0) | 13 (50.0) |
Abbreviations: HILT, high-intensity laser therapy; BMI, body mass index; OA, osteoarthritis; SD, standard deviation; No, number.
a Values are expressed as mean ± SD or No. (%).
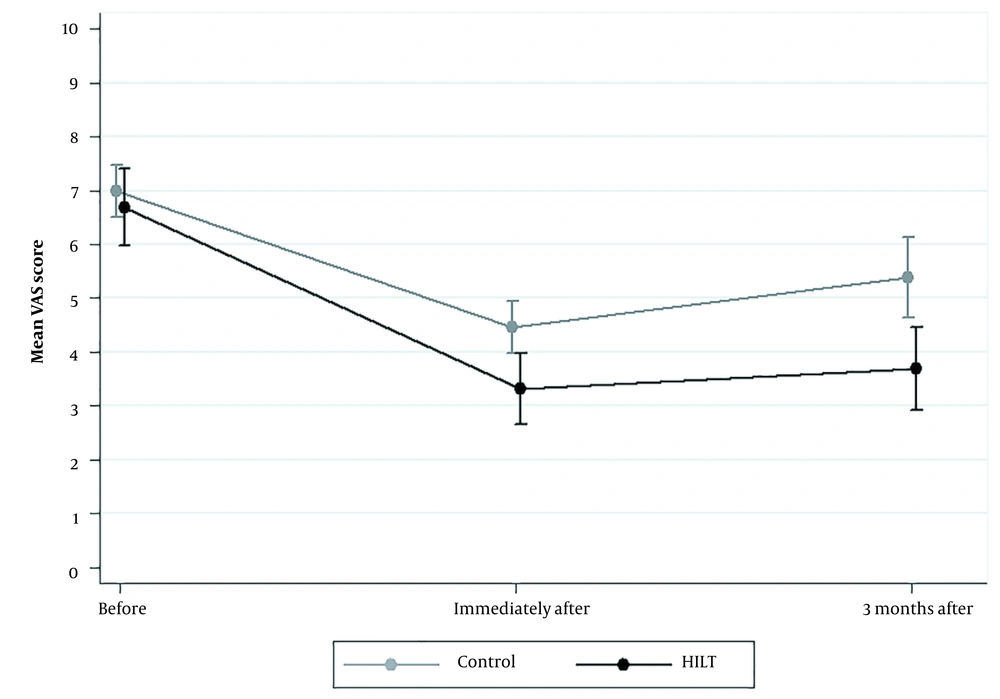
The two groups were comparable regarding VAS pain scores before treatment (P = 0.465). However, after adjusting for age, sex, and baseline values, immediately and three months after treatment, VAS pain scores were significantly lower in the HILT group than in controls (P < 0.001), with a large effect (SMD = -1.22, 95% confidence interval (CI): -1.81; -0.62 and SMD = -1.31, 95% CI: -1.90; -0.70, respectively). The results were similar for the pain subscale of WOMAC (Table 2). Figure 2 shows VAS pain scores at different time points.
| VAS | Mean (95% CI) | ES b (95% CI) | P-Value c | |
|---|---|---|---|---|
| Control (n = 26) | HILT (n = 26) | |||
| Before treatment | 7.00 (6.41; 7.59) | 6.69 (6.10; 7.29) | -0.20 (-0.75; 0.34) | 0.465 |
| Immediately after treatment a | 4.34 (4.05; 4.63) | 3.43 (3.14; 3.72) | -1.22 (-1.81; -0.62) | < 0.001 |
| Three months after treatment a | 5.27 (4.83; 5.72) | 3.80 (3.36; 4.25) | -1.31 (-1.90; -0.70) | < 0.001 |
Abbreviations: CI, confidence interval; ES, effect size; HILT, high-intensity laser therapy; VAS, Visual Analog Scale.
a Means adjusted for age, sex, and baseline values.
b ES indicates the standardized mean difference (SMD) by Cohen’s d.
c Analyzed by the ANOVA/ANCOVA test.
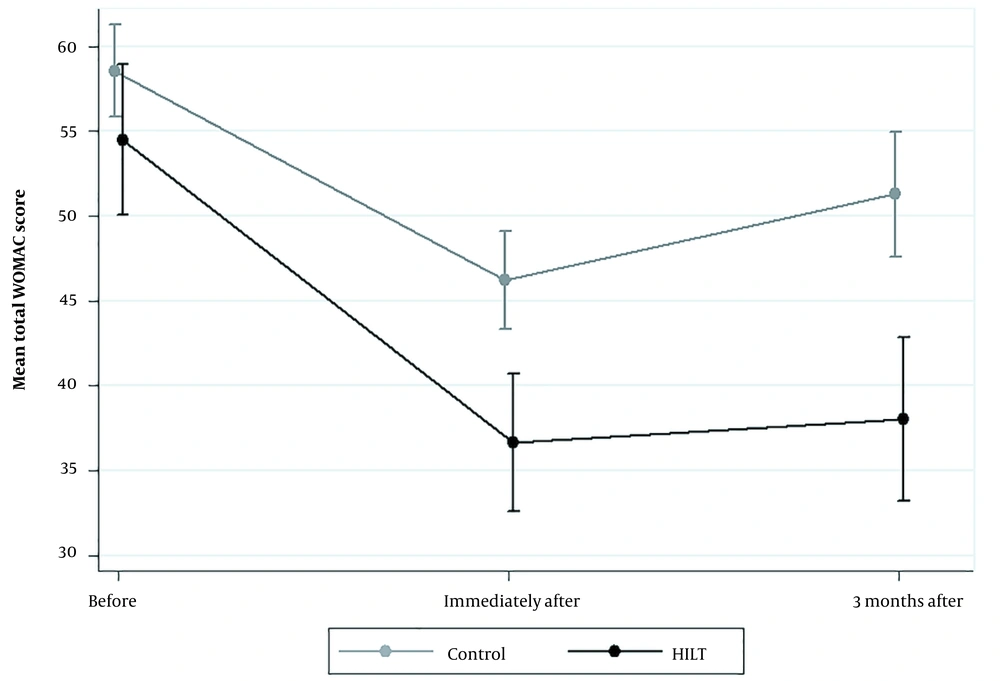
On the other hand, the WOMAC stiffness score was significantly lower in the HILT group at baseline (P = 0.003). Nevertheless, despite a comparable WOMAC stiffness score immediately after treatment (P = 0.135), this score was significantly lower in the HILT group than in the control group (SMD = -0.98, 95% CI: -1.56; -0.40, P = 0.002) three months after treatment (Table 3). Furthermore, WOMAC physical function scores were significantly lower with HILT immediately and three months after treatment (P < 0.001). The same was true for the total WOMAC score (Figure 3).
| Variables | Mean (95% CI) | ES b (95% CI) | P-Value c | |
|---|---|---|---|---|
| Control (n = 26) | HILT (n = 26) | |||
| Pain | ||||
| Before treatment | 12.46 (11.49; 13.43) | 11.15 (10.19; 12.12) | 0.53 (-0.02; 1.08) | 0.061 |
| Immediately after treatment a | 8.90 (8.45; 9.36) | 7.21 (6.76; 7.67) | -1.46 (-2.07; -0.84) | < 0.001 |
| Three months after treatment a | 10.13 (9.44; 10.82) | 7.52 (6.83; 8.22) | -1.49 (-2.10; -0.86) | < 0.001 |
| Stiffness | ||||
| Before treatment | 5.38 (4.84; 5.93) | 4.19 (3.65; 4.74) | -0.86 (-1.42; -0.29) | 0.003 |
| Immediately after treatment a | 3.85 (3.60; 4.10) | 3.57 (3.32; 3.82) | -0.45 (-1.00; 0.10) | 0.135 |
| Three months after treatment a | 4.45 (4.15; 4.75) | 3.70 (3.40; 4.00) | -0.98 (-1.56; -0.40) | 0.002 |
| Physical function | ||||
| Before treatment | 40.69 (38.18; 43.21) | 39.15 (36.64; 41.67) | -0.24 (-0.79; 0.31) | 0.389 |
| Immediately after treatment a | 32.27 (30.58; 33.96) | 27.04 (25.35; 28.72) | -1.22 (-1.81; -0.63) | < 0.001 |
| Three months after treatment a | 35.27 (33.28; 37.26) | 28.23 (26.24; 30.22) | -1.40 (-2.00; -0.78) | < 0.001 |
| Total WOMAC score | ||||
| Before treatment | 58.54 (54.96; 62.12) | 54.50 (50.92; 58.08) | -0.44 (-0.99; 0.11) | 0.116 |
| Immediately after treatment a | 44.85 (42.81; 46.89) | 38.00 (35.96; 40.03) | -1.33 (-1.92; -0.72) | < 0.001 |
| Three months after treatment a | 49.65 (47.05; 52.25) | 39.66 (37.06; 42.25) | -1.52 (-2.13; -0.89) | < 0.001 |
Abbreviations: CI, confidence interval; ES, effect size; HILT, high-intensity laser therapy; WOMAC, Western Ontario and McMaster Universities Osteoarthritis index.
a Means adjusted for age, sex, and baseline values.
b ES indicates the standardized mean difference (SMD) by Cohen’s d.
c Analyzed by the ANOVA/ANCOVA test.
5. Discussion
The results of the current study demonstrated that HILT led to a significant reduction in pain compared to the control group immediately and three months after the last treatment session. Patients in the HILT group of this study received six treatment sessions over two weeks. The major results of this research agree with those of other studies regarding pain reduction. After seven days to three months of HILT therapy, these trials also revealed a significant decrease in pain (6, 16-18, 23-25). However, these studies differed in the study population, the total energy of laser treatment, duration of treatment, follow-up period, and control groups. In another study by Samaan et al., HILT plus exercise therapy yielded better improvement in pain than low-intensity pulsed ultrasound plus exercise therapy or exercise therapy alone (26). Mostafa et al. have also demonstrated the superiority of HILT over extracorporeal shock wave therapy for pain reduction in knee OA (27). Furthermore, in two recent systematic reviews, HILT has been reported to be more effective than LLLT and other physical therapy modalities for improving pain in individuals with knee OA (28, 29).
Several mechanisms are hypothesized to be responsible for HILT's analgesic effects. At the peripheral nerves where nociceptors are found, laser aids in promoting the production of endogenous opioids such as beta-endorphins and serotonin (30). Nerve fiber regeneration and gate control theory are the other significant HILT analgesic effects (16, 18). Additionally, the laser's photo-thermal and photochemical actions might encourage cell metabolism, blood flow, nerve fiber regeneration, adjacent collateral sprouting, and the growth of Schwann cells (31). Moreover, the dorsal root ganglion neurons' ATP generation and calcium influx are decreased by laser therapy, while intracellular reactive oxygen species (ROS) are enhanced. This disrupts the transmission of the pain action potential and lessens pain (32, 33). Also, there is evidence that lasers may help reduce inflammation by decreasing inflammatory mediators and proinflammatory cytokines (34). Another function of lasers is the enhancement of bio-stimulation in knee OA, confirmed by a significant increase in synovial and femoral cartilage thickness in previous studies (6, 25).
Compared to the control group, we discovered that HILT significantly improved the WOMAC score immediately after the final treatment session and three months afterward. This is in line with the findings of prior studies, which revealed a considerable improvement in the WOMAC score after receiving four to twelve weeks of HILT therapy (6, 17, 18, 24). Contrarily, by comparing a sham laser with HILT, Siriratna et al. reported no significant difference in WOMAC score immediately after ten treatment sessions (23). The discrepancy between the current study's findings and those of Siriratna et al. (23) can be explained by the difference in treatment duration, laser intensity, OA severity, and type of exercises.
Of note, patients in the HILT group of our study had a significantly lower WOMAC stiffness score at baseline compared to controls. To eliminate the effect of this baseline difference, we adjusted the immediate- and intermediate-term scores for baseline values as well as sex and age. Nonetheless, immediately after treatment, the two groups were similar regarding the WOMAC stiffness score, which shows that stiffness improvement might only appear after three months. For individuals with knee OA, knee stiffness has major clinical ramifications (35). The degree to which knee OA patients believe their ability to do physical activities is correlated with how stiff their knees feel (36). Moreover, stiffness shows some link to physiological factors that increase the probability of falling in the elderly (37). Consequently, knee stiffness is a significant symptom of knee OA that requires attention.
In the current study, HILT was applied to the medial aspect of the knee. Interestingly, the manifestation of osteoarthritis in the medial compartment, with the lateral compartment and patella-femoral joint exhibiting relatively less damage, is a frequently encountered orthopedic condition (38). This can be explained by load distribution and anatomy; during routine activities such as standing and walking, the medial compartment of the knee experiences greater load-bearing capacity than the lateral compartment. The augmented load has the potential to induce greater degeneration of the cartilage located in the medial compartment as time progresses. The anatomy of the knee articulation may also contribute to the onset of osteoarthritis within the medial compartment. The medial meniscus exhibits greater size and firmer attachment to the joint capsule than its lateral counterpart, rendering it more vulnerable to potential damage (39).
The present study was not without limitations. First, due to the nature of the interventions and the outcome assessment, blinding of neither patients, caregivers, nor assessors could be performed. Furthermore, the control group was not subjected to a sham laser, which could be deemed a plausible technique for patient blinding. Second, we did not evaluate the patient's long-term outcomes.
5.1. Conclusions
Compared with the control group, HILT substantially reduced pain and improved WOMAC scores in patients with knee OA immediately after the final treatment session and three months later. Larger studies with a longer follow-up period are required to confirm our findings and determine the long-term efficacy of HILT for knee OA. Also, considering a sham laser for blinding would enhance the quality of future studies.