1. Background
Forward head posture (FHP) is characterized by flexion of the low cervical vertebrae and a compensatory extension of the high cervical vertebrae to keep the position of the head at a horizontal sight level, ensuring that the head remains in an anterior position concerning the shoulders (1). Due to its frequency, it is considered the most prevalent alteration in the sagittal plane. In teenagers, the prevalence of FHP can reach approximately 63% (2).
This posture is considered problematic when prolonged, such as in front of a computer or using electronic devices for long periods. FHP can cause musculoskeletal symptoms and spinal degeneration at a cervical level (3) and can cause a rectification or loss of the curvature of the cervical lordosis, muscle fatigue (4), neck pain (5), and cephalea (6), as well as sensorimotor problems (7).
Multiple factors are associated with this posture, such as the excessive use of electronic devices, sending text messages, and carrying a backpack. The misalignment caused by forward head posture can produce compensatory mechanisms at different levels, as well as changes in the lumbar spine, such as lumbar and thoracic hyperlordosis and thoracic hyperkyphosis, which may be associated with compensatory FHP (8).
The curvature of the spine in the thoracic zone presents a convexity-denominated kyphosis. The normal values of thoracic kyphosis are from 20 to 40° of the Cobb angle formed between C7 and T12 (9); an increase in this angle indicates thoracic hyperkyphosis. Thoracic hyperkyphosis affects the functional biomechanics of the shoulder complex (10). It increases the craniovertebral angle, which is why it is plausible that it is associated with forward head posture (11). A systematic review found a probable association in this regard, but it included patients from various age groups; therefore, this relationship should be investigated in certain age groups, such as teenagers (8).
Despite the wealth of research on forward head posture and other spinal abnormalities (1-6, 8, 11), there remains a significant gap in the literature concerning the specific association between thoracic kyphosis and forward head posture in adolescents. This under-researched area is critical as adolescence is a pivotal period in postural development, and early interventions can mitigate progression to chronic musculoskeletal problems. Consequently, the assumption that an increase in the angle of thoracic kyphosis may correlate with a heightened forward head posture, as expressed through the craniovertebral angle, merits rigorous investigation.
2. Objectives
This study aimed to assess the association between thoracic kyphosis and forward head posture in teenagers between 11 and 17 years of age. We hypothesized that the higher the angle is, the higher the forward head posture becomes, expressed in the craniocervical angle.
3. Methods
3.1. Research Design
This study comprised cross-sectional analytical research. Data were collected between February and March 2021, with students receiving regular basic education at a private institution. The inclusion criteria were male or female students between 11 and 17 years old. Those who suffered from previous traumatic injuries in the thoracic or cervical spine, musculoskeletal and neurological disorders, or presented with COVID-19 symptoms were excluded.
The sample size was calculated through the Epidat 4.2 program to verify associations of the following variables: Forward head posture and kyphotic angle. The minimum correlation coefficient to be detected was 0.3, the reliability level was 95%, the potency was 80%, and the calculated sample size was 84 students.
3.2. Variables and Instruments
The ending variable was forward head posture, measured through the craniocervical angle. The variable of exposition was thoracic kyphosis, and the covariables were sex, age, weight, height, and body mass index (BMI).
To measure thoracic kyphosis, two instruments were used: A flexible ruler and a bubble inclinometer, and the variable was categorized as normal (20 - 40°) or hyperkyphosis (> 40°) (9). A Stadler® flexible ruler of 24 inches and 60 cm was used (Stadler® 97160, Nuremberg, Germany). The flexible ruler was validated through radiography to determine the kyphotic angle with a correlation coefficient of r = 0.72 (12) to 0.96 (13). Additionally, the flexible ruler demonstrated adequate reliability for these measurements (12).
A SenseAid® bubble inclinometer (SenseAid, White Plains, USA) was used, which was calibrated by an independent institution that certified it for use, with margins of error ranging from ±0° 00´ 02´´ to ±0° 00´ 22´´. The inclinometer was validated compared to the modified Cobb angle calculated in spine sagittal radiography (13, 14). In this regard, excellent validity regarding people from 10 to 30 years of age (ICC = 0.89, P < 0.0001) (15) had been documented. Thus, the reliability of the inclinometer reached 0.94 (ICC), and it was considered a reliable instrument (16).
To measure forward head posture, a mobile phone application denominated Forward Head Posture© version 1.1.2 was used (SD Net, Korea). This application uses digital photogrammetry to calculate the craniovertebral angle (17). In addition, it revises the posture of the neck when the degree of the thoracic spine is measured concerning the lateral sight of the upper part of the body according to an image of the current posture.
3.3. Procedures
To measure thoracic kyphosis with the inclinometer, the participants were instructed to hold a bipedal posture with their feet separated 5 cm and not to deviate their sight or turn their head or trunk. The evaluator was positioned behind the participants and identified the spinous processes of the C7 (prominent vertex) and T12 vertebrae through anatomical palpation. The measurement was then performed at these specific spinous processes (14).
The evaluator was positioned behind the participant to measure thoracic kyphosis with a flexible ruler. Before the measurement, the examiner identified the spinous processes of the C7 and T12 vertebrae through palpation and marked them with an erasable pen. The end of the flexible ruler was then placed on the marked C7 spinous process. From this point, the ruler was carefully molded to follow the kyphotic curvature of the spine until it reached the marked T12 spinous process. Thus, the ruler replicated the spine's curvature between the points corresponding to C7 and T12. This process followed the instructions of a previous publication (18). To measure the craniovertebral angle with the Forward Head Posture© application (17), the participants were instructed to hold a bipedal posture with the feet separated by 5 cm and not to deviate their sight or turn their head or trunk. Then, the examinator moved 2 m away from the participants to take a lateral sight photograph of the upper part of the body according to an image of their current posture. In the photograph, the locations of the reference points were established, and the craniovertebral angle was calculated.
3.4. Data Analysis
To compare the proportions and means of the exposition factors to dichotomized forward head posture (normal and altered), chi-squared tests were used for the proportions. The student's t-test was used to compare the means of forward head posture between the two groups. For the multivariate analysis, Poisson regression with robust variance was used for the multivariate analysis in order to obtain the strength of association through the prevalence ratio (PR) in its unadjusted and adjusted forms.
3.5. Ethical Considerations
This project was approved by the Degrees and Titles Committee of Federico Villarreal National University and the Ethics Committee of the Research, Innovation, and Entrepreneurship Unit of the Faculty of Medical Technology (FTM) (Dictamen-17-2022/ 126-2022-UIIE-FTM-UNFV, which was used as informed consent for the parents and informed assent for the teenagers.
4. Results
4.1. Sociodemographic and Clinical Characteristics of the Sample
The tested sample included 84 students, most of whom were male (54.4%), predominating the normal size (85.7%). Regarding BMI, which relates weight to the size and corresponds to the nutritional status of the students, 52.4% weighed over the healthy level, considering the overweight (26.2%) and obesity (26.2%) categories. Moreover, 53.6% of the students reported suffering from cervical pain and 54.8% from backache during the last 12 months (Table 1).
| Characteristic | N = 84 |
|---|---|
| Sex | |
| Male | 44 (52.4) |
| Female | 40 (47.6) |
| Age (y) | 13.8 ± 1.9 |
| 11 - 13 years old | 38 (45.2) |
| 14 - 17 years old | 46 (54.8) |
| Weight (kg) | 56.88 ± 11.94 |
| Height (m) | 156.1 ± 8.2 |
| Category of height | |
| High | 4 (4.8) |
| Normal | 72 (85.7) |
| Low | 7 (8.3) |
| Very low | 1 (1.2) |
| BMI (kg/m2) | 23.3 ± 4.6 |
| BMI category | |
| Low weight | 8 (9.5) |
| Healthy weight | 32 (38.1) |
| Overweight | 22 (26.2) |
| Obesity | 22 (26.2) |
| Cervical pain (last 12 months) | |
| Yes | 45 (53.6) |
| No | 39 (46.4) |
| Backache (last 12 months) | |
| Yes | 46 (54.8) |
| No | 38 (45.2) |
Abbreviation: BMI, Body mass index.
a Values are expressed as No. (%) or mean ± standard deviation.
4.2. Anthropometric Characteristics of Thoracic Kyphosis and Forward Head Posture
The presence of hyperkyphosis was 61.9%, measured with the flexible ruler, and 75%, measured with the inclinometer. The measurement of forward head posture was obtained through the craniovertebral angle, indicating that 57.1% of the participants presented forward head posture in some phases (see Table 2).
| Characteristic | N = 84 |
|---|---|
| Flexible Ruler | |
| Kyphotic index | 43.9 ± 9.41 |
| Normal | 32 (38.1) |
| Hyperkyphosis | 52 (61.9) |
| Inclinometer | |
| Kyphotic index | 47.3 ± 8.8 |
| Normal | 21 (25) |
| Hyperkyphosis | 63 (75) |
| FHP | |
| Craniovertebral angle degrees | 12.7 ± 7.1 |
| Category of the craniovertebral angle | |
| Phase 1/normal | 36 (42.9) |
| Phase 2 | 28 (33.3) |
| Phase 3 | 19 (22.6) |
| Phase 4 | 1 (1.2) |
Abbreviation: FHP, forward head posture.
a Values are expressed as mean ± standard deviation or No. (%).
4.3. Association Between Thoracic Kyphosis and Forward Head Posture
It was found that the measurement of the kyphotic index with the flexible ruler (r = 0.47; IC95% = 0.28 - 0.62; P < 0.0001) and the inclinometer (r = 0.357; IC95% = 0.15 - 0.53; P = 0.0011) were correlated with forward head posture. The association between the kyphotic index's numeric and categorical values and forward head posture categorized as normal and forwarded are shown in Table 3.
| Characteristic | Forward Head Posture | Dif. | P | |
|---|---|---|---|---|
| Normal | Altered | |||
| Flexible Ruler | ||||
| Kyphotic index | 39.7 ± 8.59 | 47.14 ± 8.77 | -7.49 | 0.0002 b |
| Kyphosis | -31.7 | 0.004 c | ||
| Normal | 20 (62.5) | 12 (37.5) | ||
| Hyperkyphosis | 16 (30.8) | 36 (69.2) | ||
| Inclinometer | ||||
| Kyphotic index | 44 ± 8.85 | 49.8 ± 8.05 | -5.77 | 0.0025 b |
| Kyphosis | -38.1 | 0.002 c | ||
| Normal | 15 (71.4) | 6 (28.6) | ||
| Hyperkyphosis | 21 (33.3) | 42 (66.7) | ||
a Values are expressed as mean ± standard deviation or No. (%).
b Student’s t-test.
c Chi-squared test.
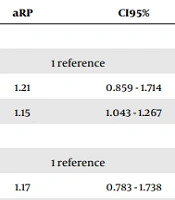
The factors associated with kyphosis and forward head posture were analyzed by Poisson regression through calculation of the unadjusted and adjusted prevalence ratio (uPR and aPR) for multiple variables. The aPR was statistically significant for the variable of age calculated in years, where the students were 15% more likely to suffer from forward head posture per year. In this way, those students who suffered from backache were 36% less likely to suffer from forward head posture. Likewise, the presence of hyperkyphosis tested with the flexible ruler was two times more likely to cause forward head posture. For the case of the inclinometer, this probability increased 2.8 folds (see Table 4).
| Characteristics | Unadjusted Model | Adjusted Model | ||||
|---|---|---|---|---|---|---|
| uPR | CI95% | P | aPR | CI95% | P | |
| Sex | ||||||
| Male | 1 reference | 1 reference | ||||
| Female | 1.1 | 0.758 - 1.596 | 0.616 | 1.21 | 0.859 - 1.714 | 0.272 a |
| Age (y) | 1.07 | 0.97 - 1.18 | 0.172 | 1.15 | 1.043 - 1.267 | 0.005 a |
| Cervical pain (last 12 months) | ||||||
| No | 1 reference | 1 reference | ||||
| Yes | 1.21 | 0.827 - 1781 | 0.323 | 1.17 | 0.783 - 1.738 | 0.448 a |
| Backache (last 12 months) | ||||||
| No | 1 reference | 1 reference | ||||
| Yes | 0.83 | 0.57 - 1.196 | 0.312 | 0.64 | 0.43 - 0.944 | 0.025 a |
| Flexible Ruler | ||||||
| Kyphotic index | 1.04 | 1.019 - 1.061 | < 0.001 | 1.04 | 1.024 - 1.063 | < 0.001 b |
| Normal | 1 reference | 1 reference | < 0.002 b | |||
| Hyperkyphosis | 1.85 | 1.136 - 2.99 | < 0.001 | 2.02 | 1.252 - 3.169 | 0.002 b |
| Inclinometer | ||||||
| Kyphotic index | 1.04 | 1.013 -1.059 | < 0.001 | 1.04 | 1.02 - 1.07 | < 0.001 b |
| Normal | 1 reference | 1 reference | ||||
| Hyperkyphosis | 2.33 | 1.156 - 4.711 | < 0.001 | 2.8 | 1.466 - 5.343 | 0.002 b |
Abbreviation: PR, prevalence ratio.
a PR adjusted to sex, age, cervical pain, backache, and body mass index and categorization of kyphosis measured with an inclinometer.
b PR adjusted to sex, age, cervical pain, backache, and body mass index.
5. Discussion
The main finding of this study was that the kyphotic angle and forward head posture were associated, as expressed through the cervical vertebral angle. Similar results were found in the research on the influence of the proximal thoracic angle (T1 and T5) on the global thoracic kyphosis and its impact on cervical alignment (lordotic, kyphotic, or straight), demonstrating that the proximal sagittal thoracic Cobb segment was significantly and positively correlated with cervical alignment (19). This was also documented in an elderly population, where the craniocervical angle was found to be correlated with thoracic kyphosis (11).
In contrast, in other research, the relationship between forward head posture, rounded shoulders, and increased thoracic kyphosis was studied in more detail. In our study, it was determined that the values of cervical lordosis were significantly related to the values of thoracic kyphosis (8). Likewise, a similarity was found regarding this study, which can be explained by the biomechanical mechanisms involved in the static posture of the spine and the head, as well as the mechanics of the craniovertebral relationship (20) and the structures involved in craniovertebral stability (21, 22).
Concerning the existing relationship between thoracic kyphosis, forward head posture, and sociodemographic sex, no relationship with sex was found. Thus, it was determined that increased computer usage was related to increased neck and head flexion in male teenagers, while increased lumbar lordosis was observed in women (23).
Other secondary findings included the clinical presentation of backache in the last 12 months, from which 54.8% of the tested teenagers suffered, as well as the association with FHP adjusted to potential confounding factors. This finding was similar to a systematic review of the association between cervicalgia and forward head posture (5).
5.1. Limitations
This research had some limitations due to its cross-sectional design, and it was not possible to establish the temporality of the variables, but it was possible to investigate their association. Another limitation was that the measurement of exposition as photogrammetry is not the gold standard for the assessment of FHP. However, it demonstrated acceptable validity for the current research.
5.2. Conclusions
It can be concluded that there seems to be a positive correlation and a statistically significant association between forward head posture and thoracic kyphosis in teenagers between 11 and 17 years of age.