1. Background
The iliotibial band (ITB) is a connective tissue made from the continuation of muscle connections, such as tensor fascia latae and gluteal muscles, and has structural and biomechanical features of fascia (1). The ITB provides postural stability (2) and affects the biomechanics of the body, especially the lower limbs (1-5). Therefore, the proper activity and flexibility of the ITB are essential to perform the aforementioned roles. The presence of acquired or structural, biomechanical impairments, such as internal tibial torsion, hip abductor muscle weakness, flat foot, and shortness of the ITB, can cause inappropriate pressure on the distal end of the band and disrupts the biomechanics of knee flexion and extension. The continuation of these impairments and distribution of inappropriate pressures can cause a wide range of symptoms and disorders in the lower limb. One of the consequences of these disorders can be the inflammation of soft tissues that causes pain and dysfunction. According to the evidence, about half of the individuals who suffer from knee joint injuries have symptoms related to the ITB in their para-clinical images (3).
Some sports activities, such as constant and daily running, put a lot of demand and tension on the muscles that have connections to the ITB. Excessive activation causes stiffness and shortening of the postural muscles and finally causes trigger points in these muscles. Since running is an integral part of most sports activities, such as football, basketball, and rugby, a decrease in flexibility and stiffness in the ITB is very likely (5). Therefore, the necessity of correcting the lack of flexibility can be a factor in improving the overall biomechanics of the body and preventing future injuries in the knee joint.
Passive stretching techniques are used to improve flexibility and maintain muscle health by increasing the range of motion (ROM) (6). According to a systematic review, regular stretching exercises can improve the flexibility of the structures, performance, and functional activities, such as strength, jumping height, and speed (7). Additionally, myofascial release techniques are commonly used for musculoskeletal injuries in athletes (8). Releasing the connective tissue individually using a foam roller is a relatively simple technique to improve target soft tissue flexibility (5). Numerous studies have investigated the effect of using a foam roller on ROM and performance (9, 10). However, the number of studies that have compared the use of a foam roller and other techniques affecting soft tissue, especially the ITB, is limited.
Another effective treatment in improving the flexibility of soft tissues is the use of active stretching techniques, such as proprioceptive neuromuscular facilitation (PNF), through the stimulation of proprioceptive pathways. There is abundant evidence that confirms the superiority of PNF active stretching over static stretching techniques (11-14). One of the important advantages of PNF active stretching is that it inhibits muscle reflex activity, which is an obstacle to stretching. Among other benefits of stretching movements, the increase in the speed of nerve conduction velocity can be mentioned, which allows better calling of muscle fibers and subsequently increases the coordination of muscle contractions to perform the movement (13). The most common PNF active stretching is the contraction-rest technique. This technique is a combination of static stretching and isometric contraction (13).
There is abundant evidence confirming the effectiveness of PNF stretching and foam roller techniques in improving the performance and flexibility of different soft tissues (5, 10, 14, 15). To date, no studies have investigated the effect of these two types of treatment on ITB extensibility in athletes.
2. Objectives
The current study aimed to investigate the effect of active stretching techniques and self-myofascial release on improving the ITB flexibility and functional performance of athletes.
3. Methods
A convenient sample of 51 semi-elite athletes with ITB shortness, aged 20 - 40 years, participated in this study. Table 1 shows the subjects’ characteristics. All the study subjects were recruited from sports centers. Patients were included if they had at least 6 hours of sports activity per week and unilateral or bilateral ITB shortness confirmed by the modified Ober’s test without any pain or limping. The exclusion criteria were as follow: (1) a history of the lower limb and pelvic girdle surgery in the last 3 months; (2) more than two lower limb surgeries; (3) structural or postural disorders, such as kyphosis or severe scoliosis; (4) neurological disorders; (5) structural disorder in the pelvis and lower limbs; (6) pregnancy; (7) rheumatoid disease; and (8) history of any fracture or trauma in the lower limb in the last year.
| Demographic Variables and Groups | Mean ± Standard Deviation | Min | Max |
|---|---|---|---|
| Age (y) | |||
| Foam roller group | 29.41 ± 7.93 | 20 | 40 |
| PNF stretch group | 27.82 ± 6.86 | 20 | 40 |
| Combination of foam roller and PNF stretching | 27.94 ± 5.23 | 20 | 36 |
| Weight (kg) | |||
| Foam roller group | 64.82 ± 12.22 | 46 | 95 |
| PNF stretch group | 63.05 ± 11.59 | 48 | 90 |
| Combination of foam roller and PNF stretching | 69.52 ± 11.31 | 54 | 97 |
| Height (cm) | |||
| Foam roller group | 167.88 ± 7.43 | 154 | 180 |
| PNF stretch group | 167.17 ± 8.94 | 155 | 185 |
| Combination of foam roller and PNF stretching | 169.11 ± 11.63 | 156 | 193 |
| Body mass index (kg/m2) | |||
| Foam roller group | 22.87 ± 3.16 | 17.80 | 29.30 |
| PNF stretch group | 22.42 ± 2.46 | 18.30 | 26.30 |
| Combination of foam roller and PNF stretching | 24.38 ± 3.82 | 20.10 | 35.60 |
Mean and Standard Deviation of Demographic Indicators in the Foam Roller Group (n = 17), Proprioceptive Neuromuscular Facilitation (PNF) Stretch Group (n = 17), and Combination of Foam Roller and PNF Stretch Group (n = 17)
The present study was registered with IRCT20210505051181N1 and the ethics code of IR.IUMS.REC.1399.788. The sample size of the main study was determined based on the information obtained from a pilot study on nine subjects, with a power of 0.8 and a confidence level of 0.95. Taking into account a 10% dropout, 51 participants were recruited. If the patients met the inclusion criteria, they entered the study after signing an informed consent form.
This parallel arm randomized clinical trial was conducted in accordance with the Consolidated Standards of Reporting Trials (CONSORT) guidelines (16) (Appendix). The subjects were randomly divided into three groups, including foam roller, PNF stretching, and a combination of foam roller and PNF stretching, using the block randomization method. In order to hide the allocation of participants to the groups, non-transparent envelopes sealed with a random sequence (SNOSE: sequentially numbered, sealed, opaque envelopes) were used. It should be noted that the examiner of this study was unaware of the randomization and registration of the participants, and this was performed by another researcher. The study was assessor-blind, and the evaluation and treatment stages were performed by two different physiotherapists. The subjects were not blinded to the treatment groups.
First, the demographic information of the patients, including age, height, weight, and body mass index, was collected. The participants were evaluated before applying each treatment and immediately after the completion of the treatment. The evaluations and interventions were performed at the Biomechanical Laboratory of Iran University of Medical Sciences, Tehran, Iran.
3.1. Interventions
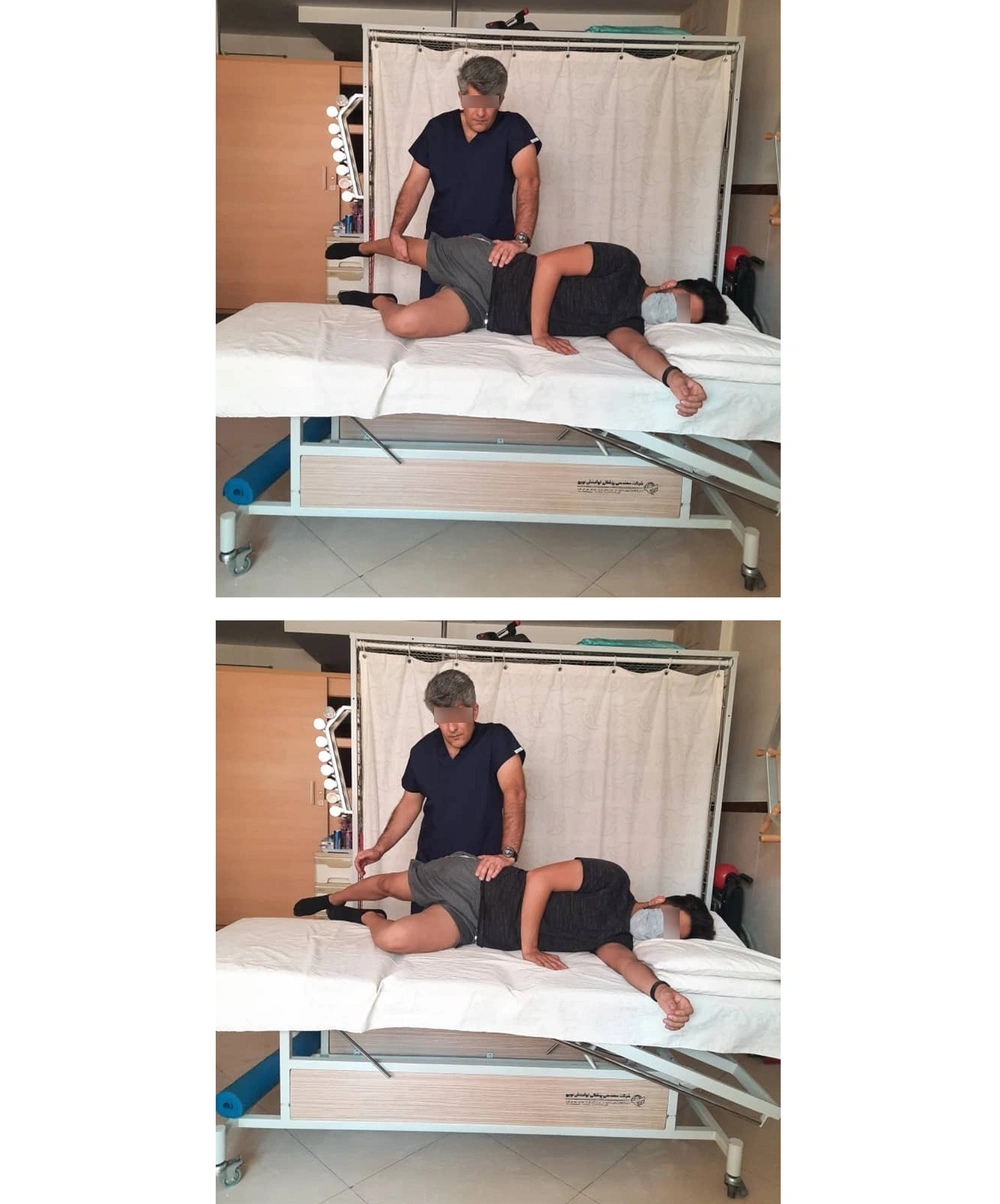
3.1.1. PNF Stretching Technique (Contraction-Relaxation)
To implement this technique, the individual lies on his/her side so that the side to be treated is up. The individual is asked to bend his/her knee to 90 degrees. The therapist is placed behind the patient in such a way that one hand of the therapist is placed on the iliac crest to maintain its stability, and with the other hand, he/she holds the knee.
The contraction relaxation technique was performed in three stages. In the first stage, the therapist slowly moved the limb from the hip joint to the end of the extension range, adduction and external rotation where the ITB was stretched, and the patient was comfortable and did not feel any pain. Then, in the second stage, the subject was asked to exert force for 5 to 8 seconds by pressing his/her foot on the therapist’s hand in the direction of flexion, abduction and internal rotation. In other words, the individual was asked to press his/her leg in the upward and forward direction with a maximum voluntary contraction while his/her knee was bent. Then, in the third stage, the individual was asked to relax his/her muscles, and this time the therapist slowly took the subject’s hip to the new range of extension, adduction and external rotation, and when reaching the end of the range, maintained the stretch. The three mentioned stages continued until there was no increase in the ROM. The PNF stretching technique took 3 - 5 minutes (17, 18).
3.1.2. Self-myofascial Release Using a Foam Roller
In this treatment method, a hard model foam roller manufactured by Modern Behsazan Eram Company, Iran, 60 cm long and 15 cm wide, was used. Before the intervention, the participants were taught how to use the foam roller. To perform the intervention, the individuals were asked to lie on their side according to Figure 1, place the foam roller at the highest junction of the ITB, and roll slowly by moving the body. The average speed of moving the foam roller was five movements per 30 seconds, and this speed was the same and constant in all participants. The subjects were asked to continue for 3 minutes until the distal end of the ITB (Figure 1). Using the foam roller took about 3 minutes. All foam roller steps were taken under the supervision of a physiotherapist.
The modified Ober’s test was used to enter the participants into the study (Figure 2) (19). The flexibility of the ITB (20) and the hip active adduction ROM were measured with an inclinometer (21). The level of performance of the participants was evaluated with the single-leg hop, vertical jump, and lateral hop tests (22). The participants performed the single-leg hop test three times, and their average was used for statistical analysis. The distance between the starting point and the endpoint was measured in meters and centimeters. According to studies, this test has good validity and reliability (23-26). The study subjects performed the lateral hop test three times, and the average of these three times was used for statistical analysis (27). According to studies, this test has good validity and reliability (23-25).
To perform the vertical jump test, a centimeter scale was installed on the wall. First, the individual was asked to show the maximum height he/she could reach on the screen with his/her dominant hand without jumping. Then, the individual was asked to touch the highest possible height by doing the maximum vertical jump with his/her dominant hand. The distance between the point that was touched the first time and the second time was considered the height of the individual’s jump. This test was repeated three times with a 3-minute rest interval between each test, and the best individual record was recorded for statistical analysis (20). According to studies, this test is easy with appropriate validity and reliability to measure an individual’s performance (28).
3.2. Statistical Analysis
The data obtained from this study were analyzed with SPSS software (version 26). Descriptive statistics (mean and standard deviation) were calculated. The Kolmogorov-Smirnov test was used to assess the normality of data. The one-way analysis of variance (ANOVA) test was used to compare the variables among three groups at the baseline. In order to analyze the analytical comparison of the studied variables among the three treatment groups before and after the interventions, the general linear model (GLM) was used. The statistical analysis was conducted at a 95% confidence interval. A P-value less than 0.05 was considered statistically significant.
4. Results
The results of the Kolmogorov-Smirnov test showed that the considered variables in all three studied groups were normal (P > 0.05), except for hip joint adduction in the foam roller group before the intervention (P < 0.05), which did not follow the normal distribution. Tables 2 - 5 show the mean and standard deviation of the ROM of active hip adduction using the inclinometer before and immediately after the therapeutic interventions and the results of the functional activity tests in the three studied groups.
| Variables and Groups | Mean ± Standard Deviation | Min | Max |
|---|---|---|---|
| Active hip adduction ROM before treatment | |||
| Foam roller group | 12.58 ± 3.60 | 3 | 16 |
| PNF stretch group | 13.52 ± 3.79 | 8 | 20 |
| Combination of foam roller and PNF stretch | 12.52 ± 3.42 | 5 | 19 |
| Active hip adduction ROM after treatment | |||
| Foam roller group | 16.41 ± 5.31 | 10 | 30 |
| PNF stretch group | 14.52 ± 3.51 | 10 | 20 |
| Combination of foam roller and PNF stretch | 14.41 ± 4.78 | 8 | 25 |
Mean and Standard Deviation of Active Hip Adduction Range of Motion Before and After Treatment in the Foam Roller Group, Proprioceptive Neuromuscular Facilitation (PNF) Stretch Group, and Combination of Foam Roller and PNF Stretch Group
| Variables and Groups | Mean ± Standard Deviation | Min | Max |
|---|---|---|---|
| Single-leg hop before treatment | |||
| Foam roller group | 114.54 ± 22.77 | 87 | 160.3 |
| PNF stretch group | 109.58 ± 20.74 | 62.6 | 156.3 |
| Combination of foam roller and PNF stretch | 115.85 ± 22.80 | 80 | 157 |
| Single-leg hop after treatment | |||
| Foam roller group | 120.52 ± 20.98 | 93.6 | 167.3 |
| PNF stretch group | 115.13 ± 20.73 | 67 | 152.3 |
| Combination of foam roller and PNF stretch | 123.67 ± 25.84 | 85 | 164.6 |
Mean and Standard Deviation of Functional Activity Test Values of Single-Leg Hop Before and After Treatment in the Foam Roller Group (n = 17), Proprioceptive Neuromuscular Facilitation (PNF) Stretch Group (n = 17), and Combination of Foam Roller and PNF Stretch Group (n = 17)
| Variables and Groups | Mean ± Standard Deviation | Min | Max |
|---|---|---|---|
| Hopping to one side before treatment | |||
| Foam roll group | 300.94 ± 74.26 | 191.6 | 411.6 |
| PNF stretch group | 285.5 ± 53.72 | 144 | 360 |
| Combination of foam roller and PNF stretch | 304.95 ± 76.89 | 199.3 | 430.3 |
| Hopping to one side after treatment | |||
| Foam roller group | 321.72 ± 70.29 | 218 | 425.6 |
| PNF stretch group | 296.85 ± 52.49 | 170.6 | 394.6 |
| Combination of foam roller and PNF stretch | 326.52 ± 89.36 | 192.6 | 471 |
Mean and Standard Deviation of Functional Activity Test Values of Hopping to One Side Before and After Treatment in the Foam Roller Group (n = 17), Proprioceptive Neuromuscular Facilitation (PNF) Stretch Group (n = 17), and Combination of Foam Roller and PNF Stretch Group (n = 17)
| Variables and Groups | Mean ± Standard Deviation | Min | Max |
|---|---|---|---|
| Vertical jumping before treatment | |||
| Foam roller group | 30.05 ± 6.87 | 20 | 44 |
| PNF stretch group | 31.05 ± 6.53 | 20 | 43 |
| Combination of foam roller and PNF stretch | 33.70 ± 8.13 | 21 | 48 |
| Vertical jumping after treatment | |||
| Foam roller group | 32.32 ± 6.76 | 22 | 45 |
| PNF stretch group | 31.64 ± 6.95 | 21 | 45 |
| Combination of foam roller and PNF stretch | 34.94 ± 10.04 | 20 | 51 |
Mean and Standard Deviation of Functional Activity Test Values of Vertical Jump Before and After Treatment in the Foam Roller Group (n = 17), Proprioceptive Neuromuscular Facilitation (PNF) Stretch Group (n = 17), and Combination of Foam Roller and PNF Stretch Group (n = 17)
The one-way ANOVA test was used to examine the studied variables in three groups: foam roller, PNF stretching, and a combination of foam roller and PNF stretching in baseline values. The results showed that the investigated variables were not significantly different in their baseline values (P > 0.05).
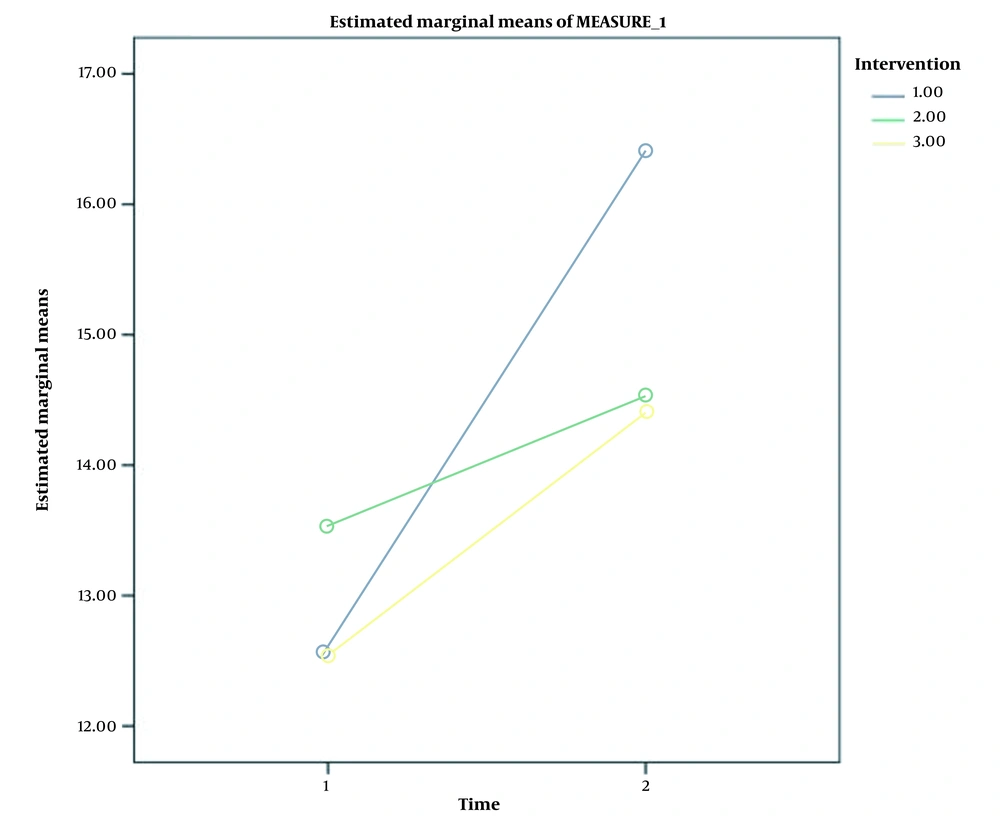
Using the GLM, the interaction effect of time and intervention on the active hip ROM was investigated in all treatment groups. It was observed that the interaction effect was not significant (P = 0.235), which indicated that all three studied groups had similar changes over time. According to the obtained results, the effect of time (P = 0.002) was significant, and the hip active adduction ROM before and after the intervention had a significant difference. The results are illustrated in Figure 3.
The interaction effect of time and intervention for the single-leg hop test was not significant (P = 0.721), which indicated that all three studied groups were not significantly different. According to the obtained results, the effect of time of the single-leg hop test was significant (P = 0.000), which indicated that the functional activity of the single-leg hop test before and immediately after treatment was significantly different. The results are illustrated in Figure 4.
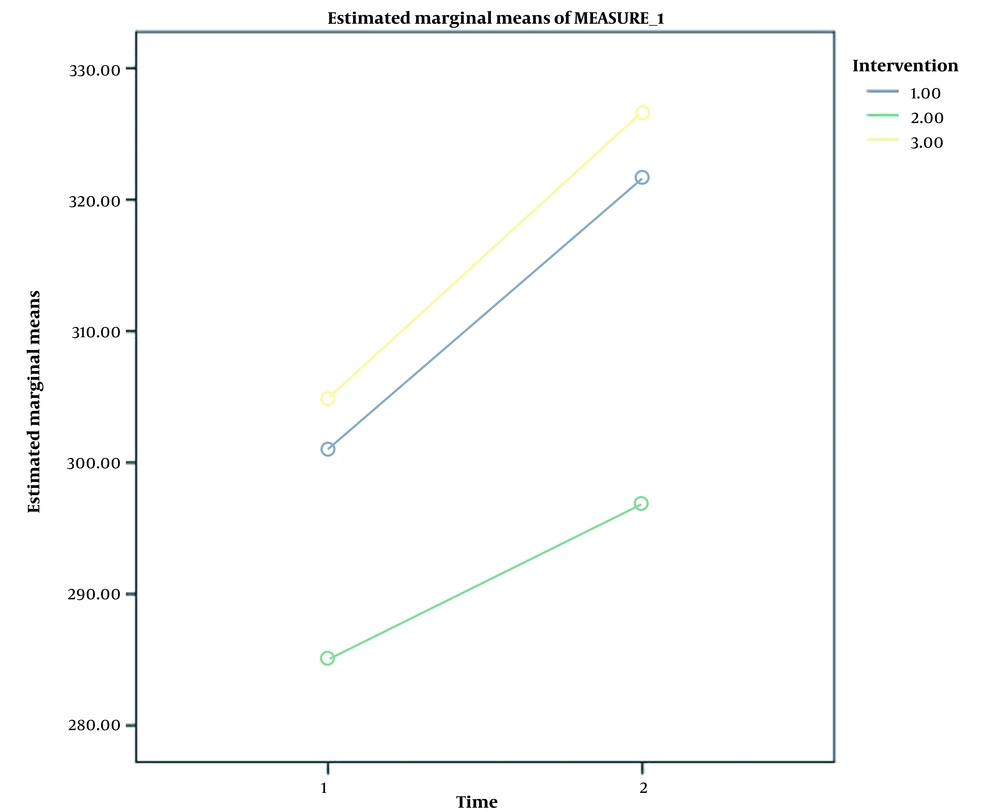
The interaction effect of time and intervention on the functional activity of the lateral hop test was not significant in all three groups (P = 0.352), which indicated that all three studied groups had similar changes. According to the obtained results, the effect of time on the functional activity of lateral hop was significant (P = 0.000), which indicated that the functional activity of lateral hop, before and immediately after the treatment, was significantly different from each other. The results are illustrated in Figure 5.
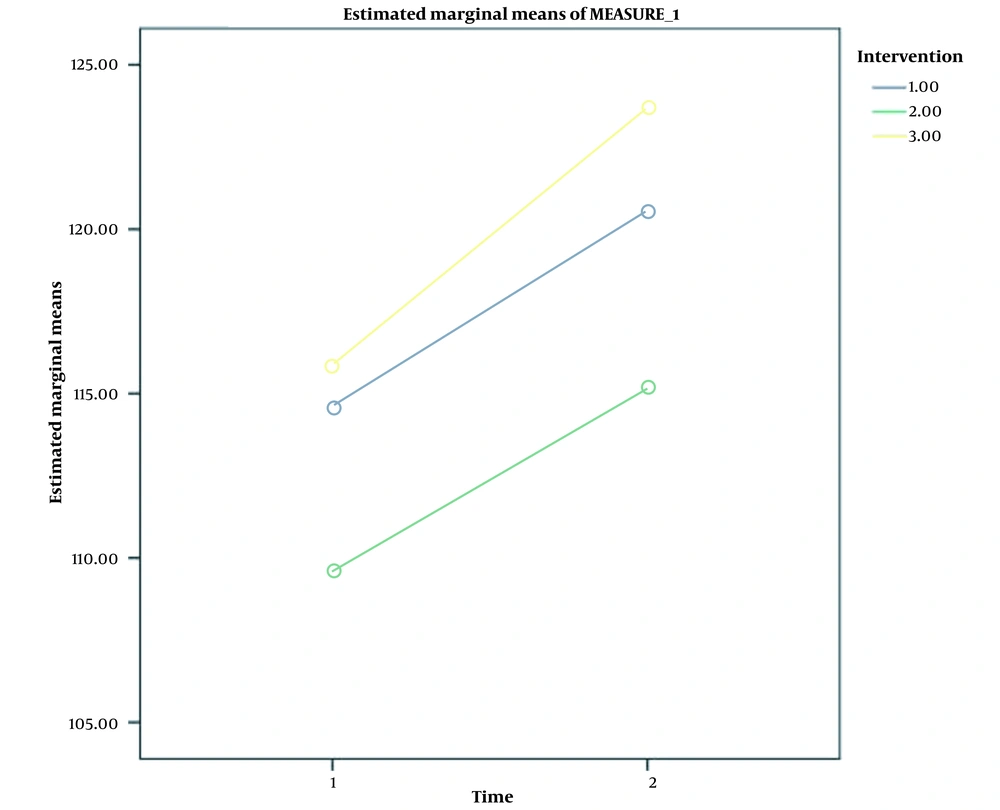
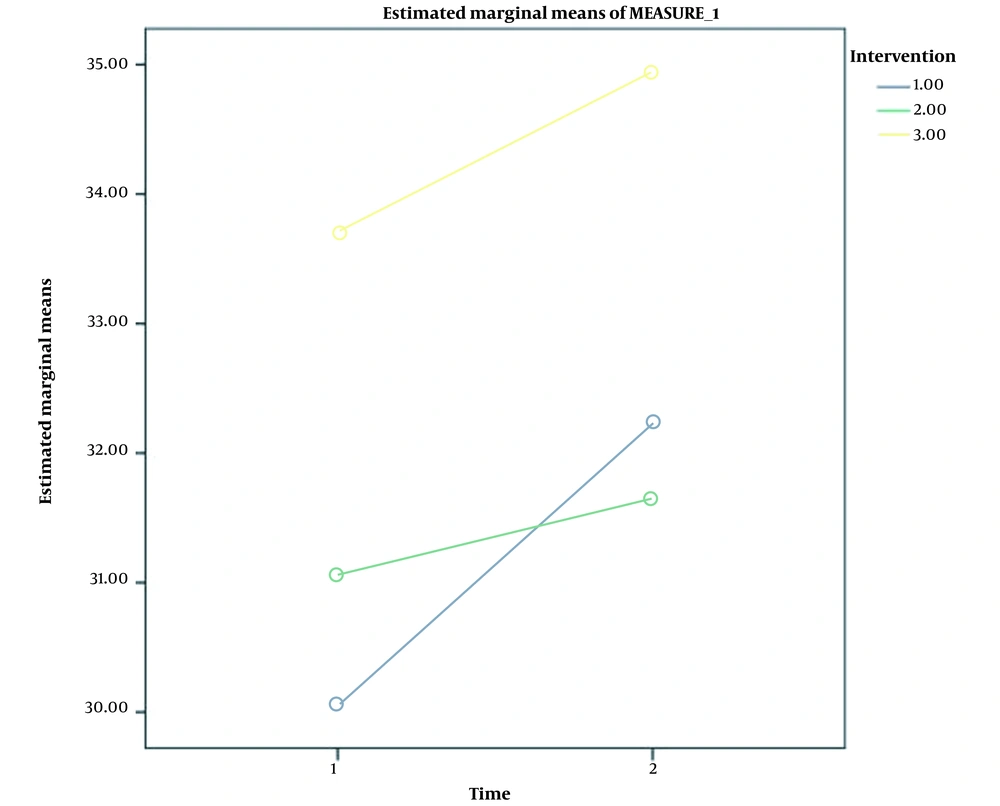
The interaction effect of time and intervention on the functional activity of vertical jump in all three groups was not significant (P = 0.264), which indicated that all three studied groups had similar changes. According to the obtained results, the effect of time on the functional activity of the vertical jump was significant (P = 0.001). Therefore, the functional activity of the vertical jump before and immediately after the treatment had significant differences from each other. The results are illustrated in Figure 6. Table 6 shows the results of a paired t-test to compare the studied variables in three groups before and after the treatment.
| Intervention and Variables | Mean Difference ± Standard Deviation | P-Value |
|---|---|---|
| Foam roller group (n = 17) | ||
| Active hip adduction ROM before and after treatment | 1.59 ± 6.57 | 0.029 |
| Single-leg hop before and after treatment | 1.49 ± 6.18 | 0.001 |
| Lateral hop before and after treatment | 4.84 ± 19.9 | 0.001 |
| Vertical jump before and after treatment | 0.64 ± 2.67 | 0.004 |
| PNF stretch group (n = 17) | ||
| Active hip adduction ROM before and after treatment | 1.04 ± 4.31 | 0.354 |
| Single-leg hop before and after treatment | 2.75 ± 11.36 | 0.061 |
| Lateral hop before and after treatment | 4.14 ± 17.08 | 0.012 |
| Vertical jump before and after treatment | 0.60 ± 2.47 | 0.342 |
| Combination group of foam roller and PNF stretch (n = 17) | ||
| Active hip adduction ROM before and after treatment | 0.74 ± 3.05 | 0.022 |
| Single-leg hop before and after treatment | 1.85 ± 7.63 | 0.001 |
| Lateral hop before and after treatment | 6.47 ± 26.7 | 0.004 |
| Vertical jump before and after treatment | 0.73 ± 3.23 | 0.135 |
Paired t-Test Results in the Foam Roller Group, Proprioceptive Neuromuscular Facilitation (PNF) Stretch Group, and Combination of Foam Roller with PNF Stretch Group Before and After Treatment
5. Discussion
The results of the present study showed that the use of a foam roller alone or in combination with the active stretching technique could increase the hip adduction ROM instantly. Nevertheless, the active stretching technique alone did not cause a significant change in the amount of hip adduction ROM. In Shere’s study, which was conducted to investigate the long-term effect of a foam roller on the flexibility of the hamstring muscle, the results indicated a significant effect of using the self-myofascial release technique on the flexibility of the hamstring muscle (10). Additionally, in the study of Patel et al., it was observed that using a foam roller can instantly increase the flexibility of the hamstring muscle (29).
Hall and Chadwick Smith showed that a one-session application of the myofascial release technique on the gluteal muscles improves hip adduction ROM (30). The results of the present study are consistent with the results of Hall and Chadwick Smith’s study. Although the one-session application of the myofascial release technique on the ITB alone did not significantly change the hip adduction ROM, it might be possible to understand the important role of releasing the gluteal muscles in increasing the active hip adduction ROM. Unlike the present study, none of the parameters related to ROM and performance had significant changes in Sharp’s study (5). The different results might be related to the method of performing the myofascial release technique.
In Hodgeston et al.’s study, applying the self-myofascial release technique for 4 weeks did not have a significant effect on hip ROM (31). In the study of Peacock et al., the self-myofascial release technique did not affect ROM and flexibility (9). In general, according to the results of studies, using a foam roller before or after exercise with mechanisms, such as increasing flexibility, improving neuromuscular efficiency, increasing blood circulation, and reducing pain and psychological effects, can increase the joints’ ROM, reduce functional disorders caused by microtraumas, and ultimately improve an individual’s functional activity. Additionally, one of the advantages of using the foam roller technique is the ease of performing the technique, not requiring many facilities, and saving the patient’s time. On the other hand, one of the disadvantages of this technique is the possibility of not performing correctly by the treated individual. Sometimes, heavy-weight athletes have problems implementing this technique (32).
The results of this study showed that the application of PNF stretching techniques did not improve the ROM, unlike Mahieu et al.’s study (33). It should be noted that the reason for the difference in the results can be related to the fact that in Mahieu et al.’s study, stretching techniques were applied for a long time; nevertheless, in the current study, only the immediate effect of this technique was investigated. Furthermore, the target tissue in the present study was the ITB; however, in the study by Mahieu et al., the target tissue was the calf muscles (33).
The present study’s results are consistent with those of Yuktasir’s study (14). In both studies, performing active stretching techniques led to the improvement of the ROM. In Yuktasir’s study, the effect of stretching techniques was applied in a long-term manner, and the target tissue was the hamstring muscle (14). In Yuktasir’s study, the jump test was used to assess an individual’s performance. The results of the current study were consistent with creating any significant changes in a performance test (14).
In López-Bedoya et al.’s study, applying the active stretching technique for 9 weeks improved hip ROM (34); however, in the present study, no significant change was observed in hip adduction ROM. The different results can be explained by considering the fact that in López-Bedoya et al.’s study, stretching techniques were applied for a long time.
Nakamura et al. examined the immediate effect of active stretching exercises on gastrocnemius muscles and improved ankle ROM unlike the present study (15). The reason for the difference in the results of the two studies can be attributed to the difference in the target tissues. The PNF stretching techniques facilitate stretching by affecting the stretch reflex of the muscle, which plays a role in creating muscle tone, is an obstacle to stretching, increases the speed of nerve conduction, allows better calling of muscle fibers, and subsequently increases the coordination of muscle contraction to perform the movement.
In Peacock et al.’s study, it was observed that the application of the self-myofascial release technique could increase vertical jump performance and single-leg hop tests (9). The results of the present study are consistent with those of Peacock et al.’s study (9).
In Hodgeston et al.’s study, unlike the present study, applying the self-myofascial release technique for 4 weeks did not show any effect on the individual’s performance during the jump test (31). The reason for this difference can be attributed to the difference in the target tissue. In Hodgeston’s study, a foam roller was applied to the hamstring and quadriceps muscles (31). In a study by Yuktasir, 6 weeks of static stretching and active stretching techniques had no effect on participants’ performance (14) as in the present study.
Vaughan et al. showed that a foam roller could instantly increase the pain threshold of the ITB (35). Else’s study also showed that the long-term application of myofascial release exercises could reduce the pain of individuals with ITB syndrome (36).
5.1. Conclusions
It is possible to conclude that the self-myofascial release technique on the ITB and the muscles connected to this band, such as the gluteal muscles, leads to the improvement of the hip adduction ROM. Additionally, the results of this study showed that applying the active PNF stretching technique is effective in lateral hop functional activity. Moreover, the combination of self-myofascial release and the active stretching technique, in addition to improving the hip active adduction ROM, enhances the individual’s performance during the functional activities of lateral hop and single-leg hop. Flexibility and ROM increased significantly in all three treatment groups, and no group was superior to the others.
5.2. Limitations
One of the weak points of this study is the lack of examination of the participants over longer periods of time to check the durability of these techniques.
5.3. Suggestions
It is suggested to carry out future studies with larger populations and in longer time intervals to determine the durability of these techniques. It is also suggested to investigate the effectiveness of these interventions in individuals with symptoms of ITB syndrome.