1. Background
Headache is a common and debilitating condition that affects individuals of all ages, resulting in decreased performance, disruption of quality of life, and a heavy economic burden on society (1). Cervicogenic headaches (CH) were first mentioned in medical literature in 1860 by Hilton; however, the term was coined by Sjaastad in 1983 to describe this type of chronic headache (2). The prevalence of CH in the general population is estimated to be between 0.4% and 2.5%, while in pain management clinics, it can reach up to 20% of patients with chronic headaches (3). The average age of individuals with this disorder is 42.9 years, and it is four times more common in females than in males (3). Cervicogenic headaches originate from musculoskeletal disorders of the upper cervical spine, and factors such as age, gender, and occupation can influence their prevalence (4). In recent years, physiotherapy has been identified as an effective treatment for this type of headache (4), and the use of educational methods such as pain neurophysiology education (PNE) has been suggested for managing pain associated with musculoskeletal disorders (5).
Pain neurophysiology education, or pain neurophysiology education, involves educating patients about the neurobiology and neurophysiology of pain processing in the nervous system (6, 7). This method has been used by physiotherapists since 2002 in various countries (8). The complex process of the nervous and brain system is explained in a way that is easily understood by everyone, using methods such as simple images, examples, pamphlets, and books (7, 9). Chronic pain affects sensory processing in the cerebral cortex, and beliefs play a role in modifying the pain experience, which is why psychological therapy is important (9). Pain neurophysiology education can help change inaccurate pain beliefs, which can lead to improved movement ability and reduced fear of movement (10). A 2011 review by Louw et al. found that educating patients about the neurophysiology and neurobiology of pain can have a positive impact on pain, disability, catastrophizing, and physical functioning in chronic musculoskeletal pain (7). Other studies have measured the effect of PNE on fatigue (10), fibromyalgia (11), chronic low back pain (12-15), and chronic neck pain (5, 16-18). Systematic review studies have shown strong evidence for the effectiveness of PNE in reducing pain ratings, disability, anxiety, and stress, as well as improving physical performance and reducing pain catastrophizing in patients with musculoskeletal pain (7, 19, 20).
The discussion about CHs is not solely academic. New analyses show that neck and back pain impose significant economic costs on society and are among the most important factors of disability.
2. Objectives
Considering the lack of studies on the effect of PNE in CHs and based on our findings, the purpose of this study is to investigate the effectiveness of PNE in treating cervicogenic headaches through a clinical trial.
3. Methods
3.1. Study Design
This study was a single-blind, randomized, controlled clinical trial conducted at the Physiotherapy Department of Kashani Hospital in Isfahan city, with data collected between July 2021 and December 2021. The research plan was approved by the Physiotherapy Department of Isfahan Faculty of Rehabilitation Sciences and subsequently submitted to the Ethics Committee of Isfahan University of Medical Sciences to obtain the code of ethics (IR.MUI.RESEARCH.REC.1399.301). The desired protocol was then registered in the Iranian Clinical Trial System (IRCT20200101045970N2).
3.2. Participants
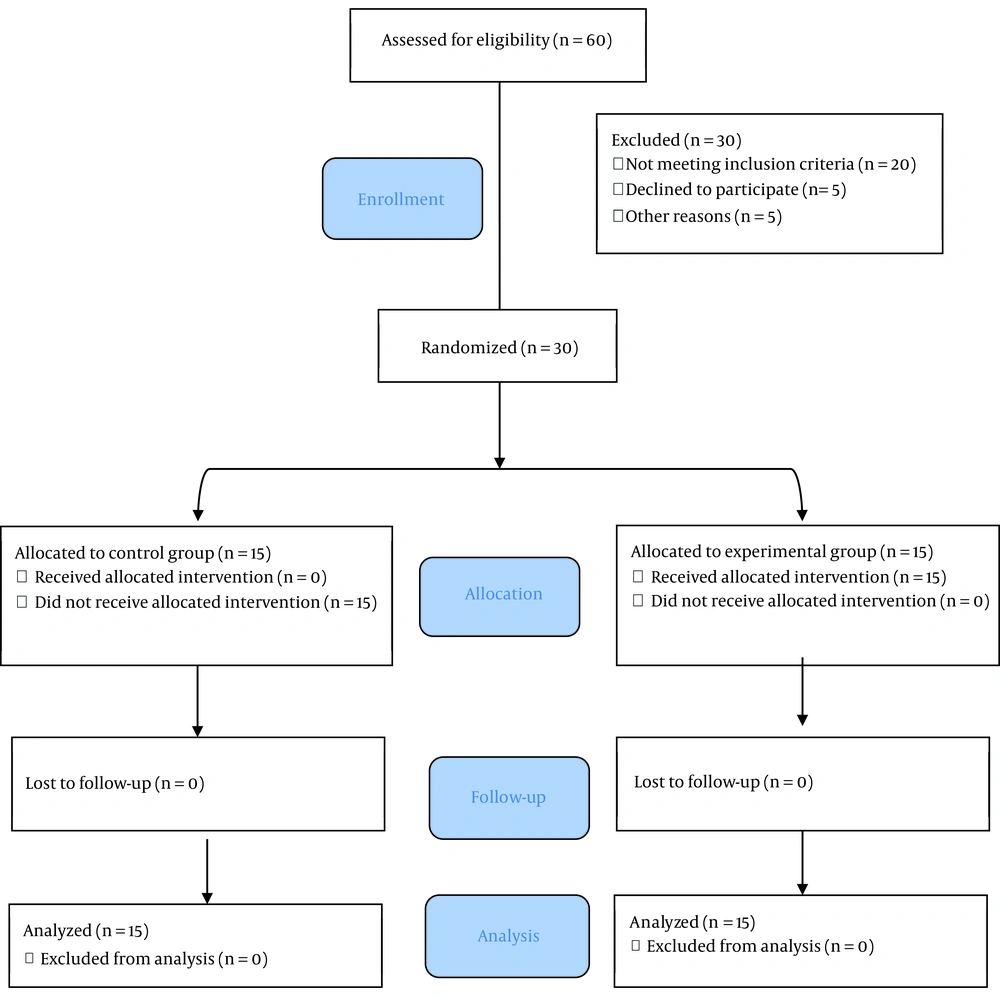
A non-probability simple sampling method was used to select a sample of 30 people among the patients with CHs referred from neurology and physiotherapy clinics affiliated with Isfahan University of Medical Sciences. The sample size was determined based on the confidence level of 95%, the power of the test of 80%, and information (d = 1.7, σ = 1.54) obtained from a previous study (12) using the following formula. The sample size was calculated to be 26 people, with 13 people in each group. Considering the possibility of 4 people attrition, the final sample size was set at 30 people.
Subjects were selected for the study based on inclusion and exclusion criteria assessed by a neurologist. The inclusion criteria consisted of having neck headaches according to the Sjasstad criteria (2) that caused unilateral head pain without changing direction and radiated to the frontotemporal area, as well as pain intensification with movement or unsuitable neck positions. Other criteria included moderate to severe non-throbbing pain based on the pain intensity scale chart, age between 18 and 60 years, a history of headaches at least once a week for more than 3 months, and being literate and able to write. The exclusion criteria consisted of neck radiculopathy pain, a history of neck trauma, any other cause of neck pain, including osteoarthritis, having received manual therapy or dry needling for neck trigger points within the last 6 months, cognitive disorders, a previous diagnosis of primary headaches such as migraine and tension headache, history of neck or shoulder surgery, and non-cooperation of the patient.
3.3. Randomization and Blinding
After the completion of the questionnaires, the participants were randomly allocated into two groups, an experimental group (n = 15) and a control group (n = 15), using the block randomization method by a third-party individual who was blinded to the study details. The participant enrollment process is illustrated in Figure 1.
3.4. Procedure
Two trained physiotherapists performed conventional physiotherapy on all patients, both in the experimental and control groups. However, the experimental group also received PNE from one of the researchers (physiotherapists), in addition to conventional physiotherapy.
3.4.1. Treatment Method in the PNE Group
In the PNE group, pain transfer methods were taught in simple ways using face-to-face training and pictures. The group sessions consisted of 3 to 5 people and were conducted once a week for four sessions, each lasting 45 - 60 minutes. Pain neurophysiology education was taught using the book "explain pain supercharged" by Butler and Moseley (21). The training focused on providing pain information to reduce fear beliefs and behaviors and to promote self-efficacy using verbal instructions, charts, and freehand drawings. The training covered topics such as the source of acute pain in the nervous system, the transformation of acute pain into chronic pain, the role of the brain in understanding pain, psychosocial factors that affect pain, and cognitive and behavioral responses related to pain and pain management. The training did not include the anatomy and biomechanics of the cervix. Patients were encouraged to participate interactively in the educational topics during the sessions.
3.4.2. Treatment Method in Conventional Physiotherapy Group
In this study, a conventional physiotherapy treatment method was used for 10 sessions over 4 weeks. The method involved using conventional transcutaneous electrical nerve stimulation (TENS) for 20 minutes with a frequency of 100 Hz and a duration of 100 microseconds (22). In addition, continuous ultrasound waves with a frequency of 1 MHz and an intensity of 1 w/cm2 were applied for 5 minutes on the suboccipital area of the posterior muscles of the upper cervical vertebrae (23). Patients were also taught therapeutic exercises, including active exercises such as chin tucks (24).
3.5. Data Collection Tools and Methods
Measurements related to headaches were taken before and after the treatment sessions and one month after completing the treatment sessions. The data was collected by a person who was completely unaware of the two groups.
In this study, pain intensity data was collected using the visual analog scale (VAS), and information regarding the disability of the patients was gathered using the headache disability index (HDI). The pain catastrophizing scale (PCS) was used to measure the degree of catastrophizing.
3.5.1. Pain Intensity
The intensity of pain was measured using the VAS. This scale consisted of a 10-cm straight line with two endpoints, "no pain" and "most severe pain". The distance between the "no pain" point and the point marked by the patient indicated the intensity of their pain. In the reliability study, the P-values varied from 0.60 to 0.77, and in the validity study, the P-values for VAS pain scores ranged from 0.76 to 0.84 (25).
3.5.2. Headache Disability Index
To evaluate the impact of headaches on daily life, the Persian version of HDI was used. The questionnaire comprised 25 items, and each item was answered with "yes" (score 4), "sometimes" (score 2), or "no" (score 0) based on the patient's experience. The questionnaire also included emotional and functional subscales. The total score ranged from zero to 100, with a higher score indicating greater disability. The validity and reliability of the HDI were assessed by Jabbari et al. (26). The content validity indices were 0.85, 0.99, and 0.97 for simplicity, relevance, and clarity, respectively. The internal consistency reliability was evaluated using Cronbach's alpha, which was found to be 0.91.
3.5.3. Pain Catastrophizing Scale
This scale, created by Sullivan and colleagues, aims to measure various dimensions of pain catastrophizing and its mechanisms. The scale comprises 13 questions with three subscales: Rumination, magnification, and helplessness, all of which evaluate negative thoughts related to pain. Participants rated each question on a scale from zero (never) to 4 (always) to describe 13 different feelings and thoughts related to their pain experience. Lower scores indicate lower levels of catastrophizing (27). In Rahmati et al.'s research, they measured the validity and reliability of the PCS and its subscales (28). Results indicated good internal consistency (alphas ranged from 0.80 to 0.89). Correlation analyses between the PCS and its subscales with measures of pain, interference, disability, depression, anxiety, catastrophizing, positive and negative effects, and pain self-efficacy beliefs support both convergent and divergent validity for the PCS and the two subscales of magnification and rumination/helplessness.
3.6. Data Analysis Method
In this study, the normal distribution of the data was checked using the Shapiro-Wilk test, and the homogeneity of dependent variables was checked using Levene's test. After confirming both, a 2 × 3 mixed model of repeated measures, ANOVA (group × time) with Bonferroni correction post hoc, was conducted. Frequency distribution in the two intervention and control groups was compared using a t-test. A P-value < 0.05 was considered statistically significant, and effect size (ES) was calculated using partial eta squared
4. Results
Before testing the research hypotheses, the normality of the variables was confirmed. Each group comprised 12 females and 3 males, and there was no significant difference between the two groups in terms of age (P = 0.22) and duration of the disease (P = 0.86), as shown in Table 1.
| Experimental (N = 15) | Control (N = 15) | |
|---|---|---|
| Age (y) | ||
| 26 - 60 | 46.33 ± 11.13 | |
| 28 - 60 | 41.40 ± 10.37 | |
| Duration of disease (mo) | ||
| 3 - 60 | 31.20 ± 25.35 | 32.80 ± 23.20 |
| Gender | ||
| Male | 4 | 4 |
| Female | 11 | 11 |
| Educational level | ||
| Diploma | 6 | 7 |
| Undergraduate | 7 | 6 |
| Master degree | 2 | 2 |
4.1. Pain Intensity
Table 2 shows the pain intensity variables of the study participants. A significant difference was observed in the various stages of pain intensity assessment (F = 49.051; P < 0.001;
| Variables | Baseline | P | Post Treatment | P | Follow Up | P | |||
|---|---|---|---|---|---|---|---|---|---|
| Experimental (n = 15) | Control (n = 15) | Experimental (n = 15) | Control (n = 15) | Experimental (n = 15) | Control (n = 15) | ||||
| VAS | 6.80 ± 1.47 | 5.93 ± 2.02 | 0.190 | 3.07 ± 1.39 | 4.27 ±1.62 | 0.038 | 4.07 ±2.09 | 4.67± 1.99 | 0.427 |
| HDI | 39.87± 13.38 | 38.13± 26.77 | 0.824 | 22.93± 12.55 | 32.67± 23.86 | 0.173 | 29.07± 16.78 | 35.07± 23.84 | 0.432 |
| PCS | 29.87 ± 8.21 | 22.47± 12.58 | 0.067 | 16.00± 7.86 | 18.13± 12.76 | 0.586 | 16.27 ± 8.89 | 19.80± 12.14 | 0.371 |
Abbreviations: VAS, visual analog scale; HDI, headache disability index; PCS, pain catastrophizing scale.
a Values are expressed as mean ± SD.
4.2. Disability
The details of the disability variables of the study participants are given in Table 2.
There was a significant difference in the levels of disability among participants at different assessment stages (F = 6.653; P = 0.003;
4.3. Pain Catastrophizing
The pain catastrophizing variables for the study participants are presented in Table 2. The analysis revealed a significant difference in pain catastrophizing evaluation across different stages (F = 25.528; P < 0.001;
5. Discussion
The results of this study indicate that the combination of pain neurophysiology training and conventional physiotherapy leads to a significant improvement in pain intensity, disability, and psychosocial factors compared to conventional physiotherapy alone among patients with CHs. These effects were sustained during a short-term follow-up period of one month.
5.1. Pain Intensity
However, while pain intensity declined in both groups, the combination of pain neurophysiology training and physical therapy produced a more significant improvement at all stages. These results are consistent with previous studies that used PNE alone (29), in combination with other treatments (6, 12, 16, 30), or with exercise therapy (14, 15, 17, 31, 32). Pain is a complex phenomenon, and the authors emphasize that pain perception is often a better indicator of potential harm than actual tissue damage. For topics related to chronic pain rehabilitation, factors such as pain, beliefs, attitudes toward pain, and strategies for managing chronic pain are crucial (33). Pain neurophysiology education is effective in changing a person's understanding and beliefs about pain, a concept often referred to as "reconceptualization" (9). Since neurophysiology training does not specifically focus on tissue damage (such as disc or joint damage) but instead targets pain processing, it may be considered a possible mechanism for reducing the perceived threat and subsequently reducing the patient's perception of pain (34).
5.2. Disability
Our study findings demonstrate that although the difference between the groups was not significant, the combination of PNE and conventional physical therapy resulted in improved performance, which is consistent with several studies (14, 16, 17, 31). In contrast, Pires et al. reported that PNE combined with aquatic exercises did not offer any advantage over pain neurophysiology training alone in improving patient performance (32). A change in pain perception can alter the perception of received pain, which in turn can affect pain generation and the ability to perform tasks (35). Patients who receive pain neurophysiology education are more likely to develop coping strategies and behaviors that lead to a reduced fear of movement and improved functioning (5). Pain neuroscience education is believed to be a useful strategy to provide people with chronic pain with the knowledge to manage their fear of movement and dependence on disability (9). The cognitive restructuring obtained through pain neuroscience education can lead to changes in the quantity and quality of movement (36).
5.3. Pain Catastrophizing
This study demonstrates that pain neurophysiology training, in combination with conventional physical therapy, resulted in a reduction in pain catastrophizing in patients with CH. These findings are consistent with previous studies on patients with chronic back pain (7, 8, 14, 29), chronic fatigue (10), fibromyalgia (11), lumbar radiculopathy (15), and chronic neck pain (17). However, some studies have failed to identify significant differences between PNE and other treatments in different patient populations (18, 37). The present study also found that PNE increased patients' awareness of the physiopathology of headaches with cervical origin, leading to a change in attitude and a reduction in pain catastrophizing when headaches occur. These results align with the findings of Javdaneh et al.'s study, which reported a significant reduction in pain catastrophizing following pain neuroscience education (17).
The use of PNE is increasing today. Pain neurophysiology education provides a detailed explanation of the biology and physiology of the nervous system and the brain's processing of pain and pain input. This concept is in direct contrast to common biomedical models that focus solely on tissues and tissue damage. Orthopedic-based professionals such as orthopedic surgeons and physical therapists commonly use models based on anatomy and anatomic pathology to describe pain to their patients. However, these models have not only shown limited effects in reducing pain and disability, but may also increase fear in patients, which in turn can amplify their pain (29, 31).
The primary limitation of this study was the lack of registration of social and demographic factors, such as occupation, social status, and economic status, which could potentially affect the results. As all evaluation criteria were assessed using self-report tools, different social statuses could be among the confounding factors in the results. Therefore, future studies aiming to evaluate outcome measures with objective measurements, such as accelerometers, are needed. Furthermore, due to the COVID-19 pandemic, it was not possible to implement the ideal grouping of participants into different groups.
Future studies should aim to evaluate outcome measures using objective measures, such as an ergometer. Additionally, the effect of the intervention was only evaluated at the 1-month follow-up, making it necessary to investigate the long-term effects of this combined intervention in future studies.
5.4. Conclusions
The use of PNE can have a positive impact on the attitude and knowledge of individuals experiencing pain in the short term. It has been shown to decrease pain and improve the ability of patients with CH. The findings of this study indicate that PNE leads to greater improvements in reducing pain and pain catastrophizing, and to some extent in reducing disability and improving physical performance.