1. Background
There were substantial changes in healthcare delivery worldwide following the coronavirus disease 2019 (COVID-19) outbreak (1, 2). Due to the lockdown and attendant social distancing requirements, there was a need for a shift to remote models of healthcare delivery (2). Several terminologies have been used interchangeably to describe electronic communication for healthcare delivery remotely (e.g., telehealth, telemedicine, telerehabilitation, and digital practice) (3). In physical therapy practice, the American Physical Therapy Association (APTA) defines telehealth as the use of electronic communication to provide and deliver health-related information and healthcare services, including, but not limited to, physical therapy-related content and services over large and small distances. Telehealth encompasses a variety of healthcare and health promotion activities, including, but not limited to, education, advice, reminders, interventions, and monitoring of interventions (4).
During the COVID-19 pandemic, due to unexpected circumstances, such as lockdown and social distance requirements, the Ministry of Health in Saudi Arabia advised all healthcare organizations to provide long-distance care via telehealth programs. Physical therapists (PTs) in Saudi Arabia possess good levels of knowledge, positive attitudes, and appropriate practices regarding COVID-19 (5). This issue suggests that PTs in Saudi Arabia are well-informed about the disease, its transmission, and the recommended protocols for preventing its spread. However, worldwide training programs for telehealth services are inadequate, especially for paramedical staff.
Many PTs lack knowledge, experience (6), confidence (7), and training (8, 9) in providing healthcare via telehealth modes, which might ultimately impact patient care. The APTA acknowledged the difficulties of providing healthcare via telehealth for PTs. As a result, in April 2021, the APTA launched a telehealth course series to address the knowledge gap in providing telehealth services among PTs. Furthermore, the Saudi Health Council, in collaboration with the Saudi Commission for Health Specialties (SCFHS), provided all healthcare practitioners with a general, short, interactive medical education resource for telehealth services. However, it is important for organizations to invest in comprehensive training programs to ensure the successful implementation and delivery of telehealth services.
Recently, several studies have shown the effectiveness of telehealth in neurological and other populations in physical therapy practice (1-3, 6, 10). Recent evidence suggests that telehealth might be a more cost-effective option for delivering healthcare in comparison to traditional face-to-face interventions (11-13). These findings suggest that telehealth has the potential to improve access to physical therapy services and reduce healthcare costs, particularly in underserved or remote areas. As a result, the utilization of telehealth will rapidly increase today and in the future. Therefore, PTs should be prepared and confident when incorporating telehealth into their care plans.
2. Objectives
This study aimed to evaluate the use, attitude and willingness, experience and confidence, and barriers to delivering healthcare via telehealth services among PTs in Saudi Arabia.
3. Methods
3.1. Study Design
This open online cross-sectional survey was approved by the Institutional Review Board of the Ministry of Health in Buraidah, Saudi Arabia (1443-1167692). Before beginning the survey, all the respondents gave their informed consent.
3.2. Participants
A cross-sectional survey was conducted online between December 2021 and May 2022 with PTs who had an active PT license and were working in Saudi Arabia at the time using convenience sampling. The sample size was calculated based on the Yamane formula as follows (14):
Where n is the sample size, N is the population size (5500 PTs) (15), and e is the level of precision (0.05). Therefore, 372 participants were required to be recruited for the study. The PTs were contacted through e-mail and social media (e.g., Twitter, Telegram, and WhatsApp). The e-mail IDs of PTs already exist as a database in Excel files. A questionnaire was sent through private messages to potential participants on Twitter, PT groups, Telegram, and WhatsApp. The PTs were informed that no identifiable information would be published or released, and their participation was voluntary. All the participants received a similar broadcast message that included the time required to complete the survey (10 minutes), the purpose of the study, and a hyperlink that directed them to the survey.
3.3. Tools and Measures
After reviewing the relevant literature, a self-developed questionnaire was designed and evaluated for face and content validity (16, 17). The questionnaire was sent to two experts to evaluate content validity. In addition, the survey was tested on a sample of PTs (n = 7) to evaluate its structure, language, and usability. Therefore, some items were slightly edited. The questionnaire aims to gather comprehensive data on demographics with 14 items to assess the use, attitude and willingness, experience and confidence, and barriers to the integration of telehealth into physical therapy practice. The responses to the items could be classified as open questions, closed-ended questions, Likert-scale questions, or multiple answers with self-nomination.
3.4. Statistical Analysis
Only the responses of the eligible participants who completed the survey and clicked submit on the last page were analyzed. The data were analyzed using SPSS software (version 19; SPSS, Inc., Chicago, Illinois, USA). Descriptive demographic information, attitude and willingness, experience and confidence, and barriers were summarized using mean, standard deviation, count (n), and percentage (%). The chi-square test was used to assess the relationship between categorical variables. The odds ratio (OR) was used to express the effect of this relationship. Correlation (Spearman’s rho) was used to measure the relationship between ordinal variables. The size effect was considered small (± 0.1), medium (± 0.3), and large (± 0.5). The level α was set at 0.05 for all statistical analyses.
4. Results
4.1. Survey Response
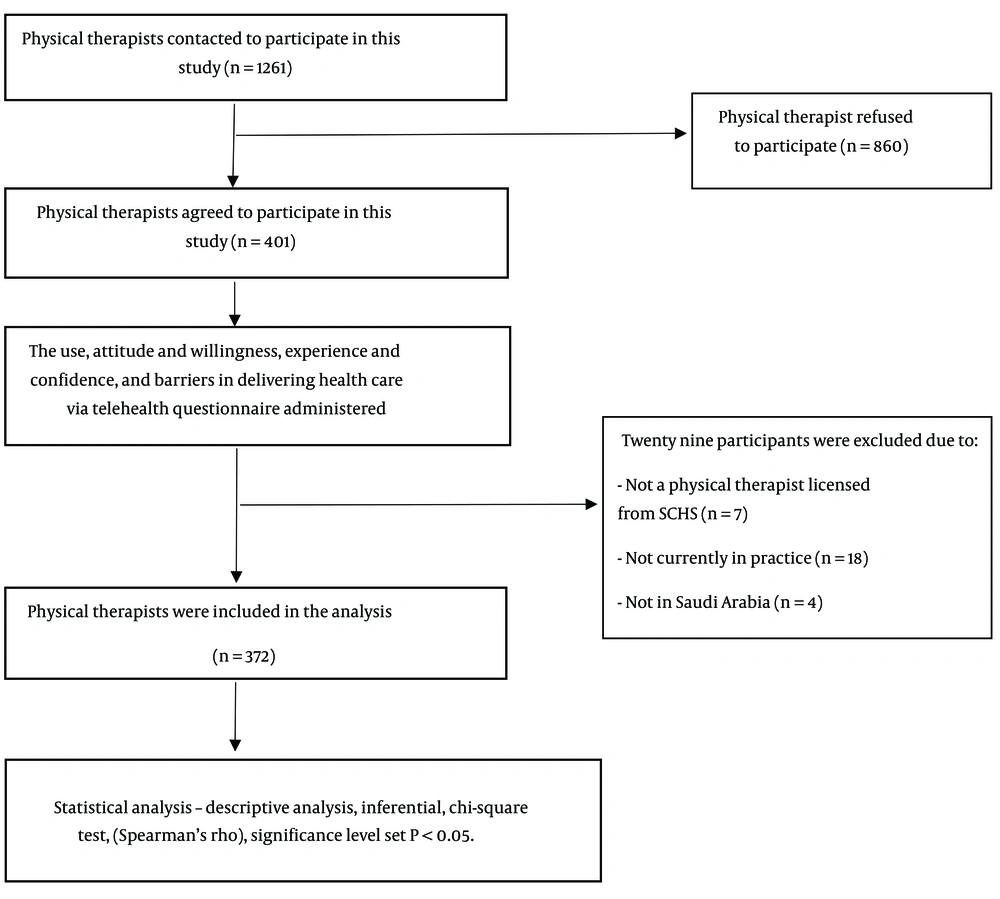
Of the 1261 potential participants who received the survey, 401 completed it. Of the 401 participants, 29 cases were excluded because they did not meet the eligibility criteria (not a PT licensed by the SCFHS [n = 7], not currently in practice [n = 18], and not in Saudi Arabia [n = 4]). Therefore, a total of 372 participants were included in the analysis. The response rate was 31.8%. The respondent PTs were from 35 cities in all regions of Saudi Arabia. Figure 1 shows the flowchart of the participants throughout the study.
4.2. Participant Characteristics
The mean age of the participants was 29 ± 5.5 years. More than half (53%) of the participants were female. Most study subjects had a clinical experience mean score of 4.4 ± 5.1 years, with the majority (73.9%) holding a bachelor’s degree in physical therapy. The predominant clinical focus was on the musculoskeletal system (29.3%). Table 1 shows detailed demographic information.
| Characteristics | Values (N = 372) |
|---|---|
| Age (y) | 29 ± 5.5 |
| Gender | |
| Male | 175 (47) |
| Female | 197 (53) |
| Nationality | |
| Saudi | 362 (97.3) |
| Non-Saudi | 10 (2.7) |
| Year of experience | 4.4 ± 5.1 |
| Highest level of education completed | |
| PT | 275 (73.9) |
| DPT | 28 (7.5) |
| MPT | 60 (16.1) |
| PhD | 9 (2.4) |
| Clinical focus | |
| Musculoskeletal system | 278 (29.3) |
| Neurology | 182 (19.2) |
| Pediatrics | 129 (13.6) |
| Cardiopulmonary diseases | 36 (3.8) |
| Geriatrics | 93 (9.8) |
| Sports injury | 54 (16.2) |
| Woman health | 33 (3.5) |
| Oncology | 20 (2.1) |
| General PT | 23 (2.5) |
| Healthcare setting | |
| Inpatient care | 157 (26.7) |
| Outpatient care | 287 (48.7) |
| Rehabilitation/Subacute rehabilitation | 117 (19.9) |
| Wellness/Prevention/Fitness | 28 (4.8) |
| Area of work | |
| Private hospital | 104 (28) |
| Public hospital | 90 (24.2) |
| Preferred not to say | 178 (47.8) |
| Living region | |
| Central | 177 (48) |
| Western | 79 (21) |
| Southern | 53 (14) |
| Northern | 43 (12) |
| Eastern | 20 (5) |
Abbreviations: SD, standard deviation; PT, physical therapist; DPT, doctor of physical therapy; MPT, master of physical therapy.
a Values are presented as No. (%) or mean ± SD.
4.3. Uses, Attitudes and Willingness, Experience, and Confidence in the Implementation of Care via Telehealth
Of the 372 participants, 143 cases (38.4%) offered telehealth consultations to an average of 23.36 ± 45.15 patients. The majority of patients (n = 121; 84.6%) used telehealth consultations during the COVID-19 pandemic. The most commonly rated platforms used in telehealth for consultation were Zoom (38.1%), FaceTime (19.1%), and Anat (11.9%). A total of 73 patients (51%) intended to continue using telehealth in the future. The majority of the participants had a moderate level of experience with using telehealth (n = 64; 44.8%). Moreover, 59.5% of the participants (n = 85) reported that using telehealth was effective for patient outcomes. Additionally, 54.5% of the participants (n = 78) were satisfied with the experience of using telehealth, and 57.4% (n = 82) received positive feedback from their patients regarding telehealth.
Overall, more than half (n = 231; 62.1%) of the PTs had not received training in telehealth. About 44.1% of the participants (n = 164) reported that their department was not equipped with the necessary tools for telehealth consultation. The participants (n = 224; 60.2%) believe telehealth is an important and useful tool in physical therapy practice. Furthermore, the PTs showed a desire to learn more about telehealth practices (n = 266; 71.5%). In general, 51% of the PTs (n = 190) were confident about using telehealth for healthcare delivery. Table 2 shows details on the use, attitudes and willingness, experience, and confidence in the implementation of telehealth.
| Survey Items | Values |
|---|---|
| Have you ever offered telehealth services to your patients? | |
| Yes | 143 (38.4) |
| No | 229 (61.6) |
| When did you offer telehealth services to your patients? | |
| Before the COVID-19 pandemic | 22 (15.4) |
| During the COVID-19 pandemic | 121 (84.6) |
| How many patients did you treat using telehealth services? | 23.36 ± 45.15 |
| Were your patients satisfied and gave positive feedback on telehealth services? | |
| Unsatisfied | 28 (19.6) |
| Neutral | 33 (23.1) |
| Satisfied | 82 (57.4) |
| Are you satisfied with your experience delivering telehealth services in physical therapy? | |
| Unsatisfied | 34 (23.8) |
| Neutral | 31 (21.7) |
| Satisfied | 78 (54.5) |
| Were your telehealth services effective for patients’ outcomes? | |
| Ineffective | 27 (18.9) |
| Neutral | 31 (21.7) |
| Effective | 85 (59.5) |
| Which applications or software were used during telehealth services? | |
| Zoom | 74 (38.1) |
| FaceTime | 37 (19.1) |
| Anat | 23 (11.9) |
| Social media | 22 (11.3) |
| Microsoft teams | 19 (9.8) |
| Sehhaty | 11 (5.7) |
| Phone calls | 5 (2.6) |
| Send material | 3 (1.5) |
| Do you intend to continue using telehealth services after the COVID-19 pandemic? | |
| Yes | 73 (51) |
| No | 27 (18.9) |
| Not sure | 43 (30.1) |
| Have you ever taken training courses or lectures on practicing telehealth services? | |
| Yes | 141 (37.9) |
| No | 231 (62.1) |
| Do you believe that telehealth services are an important and beneficial part of physical therapy practice? | |
| Yes | 224 (60.2) |
| No | 52 (14) |
| I do not know | 96 (25.8) |
| Are you confident enough to provide telehealth services? | |
| Unconfident | 78 (21) |
| Neutral | 104 (28) |
| Confident | 190 (51) |
| Is your department equipped with the necessary tools to do telehealth service (e.g., Internet network, screens, and quiet rooms)? | |
| Unequipped | 164 (44.1) |
| Neutral | 75 (20.2) |
| Equipped | 133 (35.8) |
| Are you interested in learning more about telehealth services? | |
| Yes | 266 (71.5) |
| No | 39 (10.5) |
| Not sure | 67 (18) |
| Would you like to use telehealth services in the future? | |
| Yes | 211 (56.7) |
| No | 31 (8.3) |
| Maybe | 130 (34.9) |
Abbreviations: SD, standard deviation; COVID-19, coronavirus disease 2019.
a Values are presented as No. (%) or mean ± SD.
4.4. Barriers and Challenging Factors in Implementing Telehealth
“Patient beliefs or preferences in in-person care or face-to-face care” was the most rated barrier, with 247 rates (66.4%). Other barriers included the inability to evaluate and diagnose patients (58.6%), patient inability to use technology (44.9%), and technical limitations (e.g., infrastructure, Wi-Fi, or lack of signal strength) (43.5%). Table 3 shows a list of the barriers and challenging factors.
| Barriers to Telehealth | Values |
|---|---|
| Inadequate physical therapist knowledge, experience, and confidence in telehealth service | 120 (32.3) |
| Patient beliefs or preferences in in-person care or face-to-face care | 247 (66.4) |
| Technical limitations (e.g., infrastructure, Wi-Fi, and signal strength) | 162 (43.5) |
| Inability to evaluate and diagnose patients | 218 (58.6) |
| Inability to use technology from the patient side | 167 (44.9) |
| Safety concerns (e.g., falls) | 90 (24.2) |
| Lack of reimbursement | 46 (12.4) |
a Values are presented as No. (%).
Furthermore, the analysis showed that gender (X2 [1] = 7.38; P = 0.007) had a significant effect on delivering healthcare via telehealth. The OR of patient satisfaction was 1.79 times higher when males were provided with telehealth services as compared to females. Additionally, there was a significant correlation between patient satisfaction and departmental preparation (P < 0.001). The size effect of this association was medium (r = 0.32).
5. Discussion
This study aimed to evaluate the use, attitudes, willingness, experience, confidence, and barriers to delivering healthcare via telehealth services among PTs in Saudi Arabia. The study results showed that most PTs (61.6%; 229/372) did not use telehealth, while 38.4% (143/372) did. This finding indicated that most PTs did not adopt telehealth during the pandemic, which could be due to a lack of training. However, there was an extraordinary shift toward using telehealth services from 15.4% (22/143) before the COVID-19 pandemic to 84.6% (121/143) after the onset of the COVID-19 pandemic.
The gender disparity in telehealth provision by PTs, with male PTs providing telehealth services 1.79 times more than female PTs, might be related to potential barriers or biases impacting female PTs’ ability to provide telehealth services. Prior interviews identified cultural and social barriers to telehealth, including gender issues that might prevent female PTs from attending virtual sessions in the presence of male caregivers (18). Therefore, further investigations are needed to identify and address these barriers to ensure equitable access to telehealth services for all patients, regardless of gender.
The current study experience is consistent with recent evidence on telehealth practices in physical therapy. Malliaras et al. (16) reported that two-thirds of clinicians did not use telehealth; nevertheless, a previous study reported that before the COVID pandemic, telehealth usage was reported by only 48.96% of the participants. However, during the outbreak, the usage rate significantly increased to 64.06% (19). Moreover, several studies have reported that PTs lack knowledge due to insufficient training in telehealth (16-18). Bennell et al. (17) and Malliaras et al. (16) reported that only 15% and 21% of PTs in their studies had been trained in telehealth, respectively.
The present study showed that 62.1% of the PTs did not receive training in telehealth, which could be a contributing factor to why 61.6% of PTs did not utilize this method for delivering services through telehealth. This finding highlights the need for increased education and training opportunities for PTs and patients to effectively utilize telehealth in their practice and improve patient outcomes (18). The focus on delivering care via telehealth came with the COVID-19 pandemic and restrictions on mobility due to the lockdown, which made it difficult to arrange courses for training. Therefore, it is recommended to arrange training courses or programs in telehealth for PTs after the pandemic subsides. These programs could also be included in the curricula of undergraduate and postgraduate schools to provide telehealth services beyond the pandemic.
Additionally, more than half (54.5%) of the PTs expressed positive satisfaction with delivering care via telehealth. Moreover, 56.7% of the PTs were planning to continue using telehealth services in the future. Consistent with Bennell et al.’s study results (17), PTs had moderate to high (7.1 out of 10) positive satisfaction with delivering care via telehealth, and 81% of PTs intend to continue using telehealth in the future. A previous study reported that the majority of PTs were willing to use telerehabilitation for practicing physiotherapy at a distance, had positive perceptions toward using video calls with patients or colleagues, and agreed that telerehabilitation systems could be integrated with existing conventional systems (18). Therefore, the initial evidence suggests that PTs can adopt telehealth practices if they have adequate training.
The PTs in this study rated their patient satisfaction with telehealth at a total positive rate of 57.4%. However, some PTs mentioned that patients had had at least one in-person visit for the same problem. This finding suggests that at least one visit should be in the clinic to perform the necessary assessments and examinations and to alleviate the patient’s concern about face-to-face intervention. The present study’s findings are similar to those of other studies that reported the overall satisfaction of PTs and patients (16, 18, 20-23). This satisfaction might come from the flexibility of schedules, less waiting time for treatment, lower cost of care, and easy access to technologies, such as smartphones (11, 12), in addition to successful outcomes (24-27).
The PTs identified some barriers and challenges in delivering care via telehealth with negative consequences for telehealth services in the future. Patient perceptions or preferences in in-person care and the inability to evaluate and diagnose patients were the two most commonly rated barriers. For both factors, a lack of physical contact also has a negative impact on patients and PTs (18). The lack of physical contact, lack of rapport, and patient trust have been identified as barriers to telehealth (8, 28). As a result, a hybrid approach that combines in-person and telehealth care is recommended (18). Therefore, at least one visit, probably the first, will be in person for examination and assessment, and the last visit will be for discharge. Miller et al. (22) demonstrated that PTs’ satisfaction with telehealth practices could be highest with a combination of face-to-face and telehealth sessions. Cottrell and Russell (10) reported that telehealth is mostly appropriate for observational assessments, such as pain, swelling, and balance, but not for those assessments that require physical contact, such as some special tests. In this situation, one or two in-person visits could help alleviate these barriers.
Technological issues were also identified as barriers to telehealth in this study and other studies (29, 30). Both PTs and patients were relatively inexperienced in telehealth practice. Probably, with training, more practice, and further experience, these technical issues will be reduced. Moreover, designing a telehealth application or software (a telehealth toolkit) for physical therapy might be helpful. Anat and Sehhaty are applications launched recently by the Ministry of Health after COVID-19. Anat is a telemedicine application that allows patients to consult with healthcare providers remotely. Nevertheless, Sehhaty is a health services application that provides various healthcare services, such as booking appointments and having access to medical records. However, PTs in this study mostly used the Zoom platform, which was not designed for physical therapy telehealth practice.
Unequipped departments and a lack of infrastructure for telehealth services are also known as barriers to telehealth services in this study and other studies (16-18, 29). In this study, only 36% of the therapists were satisfied with the department’s infrastructure and preparation for telehealth services. Telehealth services require an appropriate environment and room setup, such as a quiet room, good camera angles, lighting, a good working space, computers, and strong Wi-Fi signals. Addressing the aforementioned gaps in telehealth practices will increase the effectiveness and feasibility of telehealth services. In particular, in this study, patient satisfaction was positively associated with department preparation.
Contrary to other studies’ results, a lack of reimbursement was rated as the lowest barrier to telehealth services at 4.4%. In Saudi Arabia, patients who visit public hospitals for treatment are not charged fees. Additionally, all public hospitals do not require insurance for treatment. Despite untrained therapists, technological barriers, and the inability to evaluate and diagnose patients, 59.5% of the PTs in this study believed that telehealth was effective for their patients’ outcomes, 60.2% believed that telehealth is an important and useful tool in physical therapy, and 51% felt confident using telehealth to treat their patients. Similarly, several studies reported that telehealth is an effective intervention in physical therapy, or even better than in-person care (17), for musculoskeletal conditions (31), neurological conditions (24, 32), joint surgery rehabilitation (33), and cardiac rehabilitation (34). Nevertheless, Malliaras et al. (16) reported that only 42% of the participants agreed that telehealth was as effective as face-to-face care. Importantly, a systematic review study showed high patient satisfaction and effective clinical outcomes for musculoskeletal pain conditions in favor of telerehabilitation (25). The aforementioned findings suggest that patient perceptions of telehealth might vary depending on the specific health condition being treated. It is important for healthcare providers to consider patient preferences and needs when deciding whether to use telehealth or face-to-face care.
This study has some limitations. Firstly, the survey was an open online survey that might have included duplicate submissions. This is despite the statement that the authors issued (i.e., “Please submit only once”). Secondly, only one-third of the participants had telehealth experience necessitating exercising caution when generalizing the results to telehealth practice in physical therapy. However, this study has provided insights into the perceptions of PTs about practicing telehealth during the COVID-19 pandemic. Thirdly, this study did not assess the patients’ perceptions of telehealth practices. It is recommended that future studies focus on patients’ and therapists’ experiences with telehealth services.
5.1. Conclusions
In conclusion, this study showed that PTs had a trend toward positive experience, effectiveness, and confidence in telehealth. These positive findings make telehealth practice feasible and acceptable in healthcare services for physical therapy interventions. However, some physical and technological barriers need to be addressed to improve the services. Further research can shed light on the types of interventions best supported by telehealth, timing, and delivery methodology. Further studies would also highlight the patient profile best suited to this mode of delivery and best practices for integration with face-to-face contact.