1. Background
Abnormal head and neck postures are important in cervical spine dysfunction (1). Forward head posture (FHP) is among the most common findings in people with head and neck disorders. In this posture, the head and neck take place in a forward position relative to the line of gravity. It changes the curves of the upper cervical, lower cervical, and thoracic spine and can change the function of the muscles around this area (2). Also, FHP can cause additional compressive forces on the neck, change the cervical spine's normal movement patterns, and lead to pain by changing the neuromuscular control (3).
Pathological changes in head posture and the curve of the spine can cause disorders in the muscle length-tension relationship, the alignment of joint surfaces, the balance of muscle strength, and joint range of motion (ROM). This disorder can increase the pressure on the supporting structures, discs, and ligaments of the spine, cause fatigue and pain, and finally lead to functional dysfunction (4-6). Also, FHP does not necessarily present with symptoms and pain (7). Therefore, evaluating posture and investigating the movement of the assessed body part can be an effective way to prevent additional disorders.
Comprehensive studies of biomechanical changes in the head and neck (upper and lower parts separately) are necessary to correct postural habits and achieve proper alignment and function of the spine (8, 9). In most studies, the neck is considered one "joint," while the upper and lower parts of the cervical spine have biomechanically different actions (10). In addition, in the differential diagnosis of cervical disorders, special attention to the upper and lower parts of the cervical and thoracic spine is much more accurate and useful than the general view of the cervical spine as a "segment" (10, 11). Hence, measuring the motion range of the neck in two separate parts of the upper and lower cervical can be valuable and useful in evaluating and treating patients (11).
2. Objectives
This study aimed to use a photographic method to perform a comprehensive clinical posture evaluation in young people with FHP and non-FHP. Since timely diagnosis and appropriate treatment are important to prevent further complications of this kinematic chain disorder, postural variables of the head and neck were evaluated by focusing on their separate parts in the static and quasi-static states.
3. Methods
This observational-analytical case-control study included 175 people with no history of neck pain in the past 6 months, 138 with FHP, and 37 non-FHP. The participants included male and female students from Isfahan Universities of Medical Sciences. The sample size was calculated based on a preliminary study of 30 students without a history of neck pain using G-power software with a power of 85% and α of 95%. According to the results of quasi-static analyses of posture, the mean and SD of the craniocervical angle (CVA), which is the main angle used to detect the FHP, were used to estimate the sample size.
The age range was 18 - 27 years, and the body mass index (BMI) was 20 - 25 (12). Exclusion criteria included a history of myelopathy, rheumatoid arthritis, neck fractures and dislocations, cervical discopathy and spondylosis, head injury, head and neck surgery, muscle spasm with limited range of motion, cervical torticollis and scoliosis, any visible postural disorders (such as severe thoracic spine kyphosis, genovalgum, genu varum, and pelvic tilt), use of glasses with multifocal lenses and hearing aids, chronic respiratory disorders, cervical spine congenital anomalies, and pregnancy (13-16). This study was approved by the Ethics Committee of Tabriz University of Medical Sciences (code: TBZMED.REC.1394.97). A photographic method was used to evaluate the posture of the head and the posture of the upper and lower cervical spine in the sagittal plane (17-19). The Olympus VG170 digital camera was mounted on a tripod on the left side of the participants. A tripod was placed 1.5 meters from the participants at shoulder level. To determine the amount of FHP, the CVA was measured in a standing position. If the CVA was less than 48°, the individual was placed in the FHP group, and if it was greater than 48°, they were placed in the non-FHP group (20).
The participants were asked to stand in a natural position. To normalize the head and neck posture, the "self-adjusting posture" was used (18, 21). The anatomical landmarks included the tragus of the ear, the acromion process, the outer corner of the eye, the middle of the chin, the jugular notch, the spinous process of the seventh cervical vertebra (C7), and the first thoracic vertebra (T1).
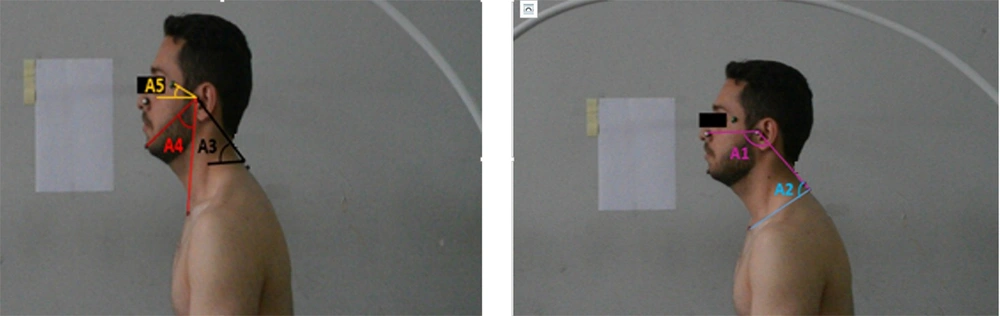
The postural angles, including the upper cervical, lower cervical, craniovertebral, head posture, and head tilt angles, were measured in the static state (head and neck neutral position) and quasi-static state (while moving head and neck in the sagittal plane) in a sitting position in two groups. AutoCAD 2010 software was used to measure the postural angles.
The upper cervical angle is the angle between the line connecting the external nasal border to the tragus and the line connecting the tragus to the spinous process of T1. The lower cervical angle is the angle between the tragus, the spinal process of T1, and the suprasternal notch (22). The craniovertebral angle is defined as the interline angle connecting the tragus to the spinal process of the C7 and the horizontal line passing through the spinal process of the C7 (21). The head posture angle is the angle between the line connecting the jugular notch to the middle of the chin and the line connecting the jugular notch to the spinal process of the C7 (18). The head tilt angle is defined as the inter-line angle that connects the canthus of the eye to the ear tragus and the horizontal line passing through the tragus (17).
Evaluating the head and neck posture in the static state:
According to the previous step, the images were prepared with photography in a sitting position, and the postural angles (upper cervical, lower cervical, craniovertebral, head posture, and head tilt angle) were calculated using AutoCAD 2010 software (Figure 1).
Evaluating the head and neck posture in a quasi-static state:
The participants were asked to uniformly perform head and neck flexion and extension at low speeds (23). They started the head and neck full flexion to reach the head and neck full extension and immediately returned to head and neck full flexion. The rhythm and speed of movement were controlled by a metronome (24, 25). A semicircular device made of polyethylene was used to reduce head tilt and rotation during the test and to ensure the movement was in the sagittal plate as possible. One belt was used under the seventh thoracic vertebra to hold the trunk firmly on the chair and prevent extra movement (26). A series of photos at the speed of one frame per second were taken during the full cervical flexion to full extension movement and return from full cervical extension to full flexion movement. Photography was repeated three times in each subject. Three measurements were done, with a two-minute rest between each measurement. The average of the three measurements was calculated for analysis.
In order to eliminate the effect of variation in the participants' ROM, five frames were selected (12): The first frame showed the beginning of the movement (full flexion), the second frame represented the middle point of neck full flexion to full extension movement, the third frame representing the end point of neck full extension, the fourth frame representing the middle point of neck full extension to full flexion movement, and the fifth frames representing the end of the movement (full flexion). In order to investigate the changes in the angles during motion, the difference between the angles in two consecutive frames was used for statistical analysis. Hence, we had four phases of movement: Phase 1 between frames one and two, phase 2 between frames two and three, phase 3 between frames three and four, and phase 4 between frames four and five. Finally, using AutoCAD 2010 software, the images were analyzed, and their angles were measured.
The examiner who marked the points to measure and calculate the angles and the statistical analyzer were blinded to the participants' presence or absence of FHP.
3.1. Reliability
The reliability of head and neck posture in 30 volunteers in two sessions (3 times each session) with an interval of one week was evaluated by a photographic method. Also, another examiner marked the designated points on the subjects' bodies independently. The average results of 3 repetitions in one session were analyzed. To check the relative reliability of these variables, the ICC model was used, and SEM was used to check the absolute repeatability. It should be noted that the confidence interval was 95%.
3.2. Statistical Analysis
We used SPSS software (version 18) for statistical data analysis. This study assessed the normal distribution assumption using the Kolmogorov-Smirnov (KS) test. An independent t-test was used to compare the studied variables. The nonparametric Mann-Whitney test was used to analyze data that did not follow a normal distribution. Pearson's correlation test was used to determine the correlation between the postural angles. The Munro classification was used to interpret the intensity of the relationship with Pearson correlation as follows: 0.8 - 1 (very strong relationship), 0.6 - 0.8 (strong relationship), 0.4 - 0.6 (moderate relationship), and 0.2 - 0.4 (low relationship) (27).
4. Results
4.1. Static State Results
Descriptive data for both groups are shown in Table 1. According to the KS test, most variables had a normal distribution, except CVA. The results showed no significant differences between the two groups in age, height, and weight. The BMI of the non-FHP group was lower than that of the FHP group, and both were within normal limits (Table 1). An independent t-test was used to compare quantitative variables between the groups. With the Mann-Whitney U test, the mean CVA was compared between the two groups with FHP and non-FHP. Significant differences were in the upper and lower cervical angles (P-value < 0.05). The upper cervical angle was higher in the FHP group than in the non-FHP group. The lower cervical angle was higher in the non-FHP group than in the FHP group (Table 1).
| Variables (Scale) | Age (y) | High (cm) | Weight (kg) | BMI (kg/m2) | Upper Cervical Angle (Degree) | Lower Cervical Angle (Degree) | Craniovertebral Angle (Degree) | Head Posture Angle (Degree) | Tilt Head Angle (Degree) |
|---|---|---|---|---|---|---|---|---|---|
| With FHP | 21.1 ± 37.44 | 170.9 ± 05.11 | 64.8 ± 47.54 | 22.1 ± 22.57 | 131 ± 24.93 | 70.6 ± 96.10 | 40.4 ± 88.27 | 44.6 ± 57.21 | 21.8 ± 30.23 |
| Non-FHP | 21.1 ± 91.92 | 171.1 ± 51.44 | 63.9 ± 81.34 | 21.1 ± 60.46 | 125.6 ± 07.97 | 75.7 ± 54.90 | 50.2 ± 53.87 | 42.5 ± 63.94 | 24.7 ± 02.43 |
| P-value | 0.11 | 0.40 | 0.68 | 0.03 b | 0.00 b | 0.00 b | 0.00 b | 0.09 | 0.07 |
Abbreviations: BMI, body mass index; FHP, forward head posture; SD, standard deviation.
a Values are expressed as mean ± SD.
b Statistical significance (P-value < 0.05).
In both groups, there was a strong and positive correlation between upper cervical angle and head posture (P-value = 0.00 and r2 = 0.68 - 0.74). Also, there was a strong and positive correlation between upper cervical angle and head tilt (P-value = 0.00 and r2 = 0.73 - 0.74). A moderate to strong positive correlation was found between head posture angle and head tilt (P-value = 0.00 and r2 = 0.59 - 0.66).
4.2. Quasi-static State Results
The first phase:
The differences in changes in the lower cervical angle and CVA were significant between the two groups (P-value < 0.05). The number of differences was higher in the non-FHP group than in the FHP group (Table 2).
| Groups | Upper Cervical Angle | P-Value | Lower Cervical Angle | P-Value | Craniovertebral Angle | P-Value | Head Posture Angle | P-Value | Tilt Head Angle | P-Value |
|---|---|---|---|---|---|---|---|---|---|---|
| Phase 1 | 0.61 | 0.05 c | 0.03 c | 0.86 | 0.91 | |||||
| With FHP | 35.8 ± 69.27 | 24.5 ± 98.91 | 41.9 ± 38.19 | 37.7 ± 54.30 | 72.1 ± 04.80 | |||||
| Non-FHP | 34.6 ± 94.97 | 27.6 ± 18.8 | 45.9 ± 09.85 | 37.6 ± 31.68 | 72.1 ± 30.61 | |||||
| Phase 2 | 0.04 c | 0.03 c | 0.05 c | 0.04 c | 0.03 c | |||||
| With FHP | 22.7 ± 57.37 | 15.6 ± 37.46 | 27.8 ± 91.58 | 22.6 ± 19.48 | 49.12 ± 38.23 | |||||
| Non-FHP | 25.7 ± 26.25 | 17.6 ± 91.10 | 31.10 ± 17.93 | 24.6 ± 63.81 | 54.14 ± 59.82 | |||||
| Phase 3 | 0.00 c | 0.00 c | 0.01 c | 0.00 c | 0.00 c | |||||
| With FHP | -21.6 ± 00.87 | -21.6 ± 00.87 | -28.8 ± 12.47 | -21.6 ± 46.22 | -48.11 ± 28.71 | |||||
| Non-FHP | -25.8 ± 05.00 | -25.8 ± 05.00 | -32.10 ± 44.44 | -25.8 ± 48.10 | -55.16 ± 37.08 | |||||
| Phase 4 | 0.27 | 0.29 | 0.06 | 0.36 | 0.47 | |||||
| With FHP | -37.8 ± 42.75 | -25.5 ± 49.76 | -41.9 ± 67.46 | -38.7 ± 39.45 | -37.8 ± 42.75 | |||||
| Non-FHP | -35.6 ± 72.94 | -26.7 ± 94.82 | -45.10 ± 01.48 | -37.6 ± 18.03 | -35.6 ± 72.94 | |||||
| Full flexion to full extension | 0.25 | 0.00 c | 0.00 c | 0.13 | 0.07 | |||||
| With FHP | 58.9 ± 26.03 | 40.7 ± 35.38 | 69.12 ± 30.79 | 59.7 ± 74.60 | 121.15 ± 43.51 | |||||
| Non-FHP | 60.9 ± 21.95 | 45.8 ± 09.69 | 76.15 ± 27.45 | 61.8 ± 94.74 | 126.20 ± 90.31 | |||||
| Full extension to full flexion | 0.18 | 0.00 c | 0.00 c | 0.06 | 0.00 c | |||||
| With FHP | -58.9 ± 43.30 | -40.7 ± 55.42 | -69.12 ± 79.92 | -59.7 ± 85.86 | -121.16 ± 69.84 | |||||
| Non-FHP | -60.9 ± 77.94 | -45.8 ± 53.89 | -77.15 ± 46.11 | -62.8 ± 67.80 | -130.18 ± 57.83 |
Abbreviations: FHP, forward head posture; SD, standard deviation.
a Values are expressed as mean ± SD.
b An independent t-test was used to check the parametric variables, and the Mann-Whitney U test was used to compare the two groups' craniovertebral angles.
c Statistically significant (P-value < 0.05).
The second phase:
The changes in the upper cervical, lower cervical, craniovertebral, head postural, and head tilt angles significantly differed between the two groups (P-value < 0.05). They were higher in the non-FHP group than in the FHP group (Table 2).
The third phase:
There were significant differences between the two groups in the changes in the upper and lower cervical, head posture, and head tilt angles (P-value < 0.05). They were higher in the non-FHP group. The CVA changes were significantly lower in the non-FHP group (Table 2).
The fourth phase:
There was a significant difference in changes in the CVA between the two groups (P-value < 0.05). It was significantly lower in the non-FHP group than in the FHP group (Table 2).
4.3. Correlation
In both groups, the correlation between the upper cervical angle and head posture was very strong and positive in all phases (P-value = 0.00 and r2 = 0.81 - 0.92). A moderate to very strong and positive correlation existed between the upper cervical angle and head tilt (P-value = 0.00 and r2 = 0.55 - 0.87). The correlation between the lower cervical angle and CVA was strong to very strong and positive (P-value = 0.00 and r2 = 0.60 - 0.82). A moderate to strong and positive correlation was seen between the lower cervical angle and head tilt (P-value = 0.00 and r2 = 0.51 - 0.75) (except in the FHP group in the third phase). The CVA and head tilt had a moderate to very strong and positive correlation (P-value = 0.00 and r2 = 0.55 - 0.92). Also, the correlation between the head posture angle and head tilt was moderate to very strong and positive (P-value = 0.00 and r2 = 0.56 - 0.89) (except in the non-FHP group in the first phase). There was a strong and positive correlation between the upper cervical angle and the CVA only at the third phase in the non-FHP group (P-value = 0.00 and r2 = 0.63). The correlation between the lower cervical angle and head posture was strong and positive (P-value = 0.00 and r2 = 0.61). The CVA and head posture correlation was strong and positive (P-value = 0.00 and r2 = 0.70).
The relative and absolute intra-session, inter-examiner, and intra-examiner reliability results of postural variables (upper cervical, lower cervical, craniovertebral, head posture, and head tilt angles) were obtained as high to very high (ICC: 0.785 - 0.949; SEM: 0.01 - 0.14 degrees).
5. Discussion
In an optimal posture, the spine has natural arches and creates muscular-skeletal balance with minimal muscle force through proper function. In this case, it applies the least amount of stress and strain on the body so that it helps the functioning of the internal organs, nervous system, and respiratory system, as well (13). The present study assessed static and quasi-static states to investigate the effects of FHP on the upper and lower cervical position changes during the flexion and extension movements of the head and neck.
5.1. Static State
The results showed that the C and lower cervical angles were more in non-FHP subjects than in the FHP group. Mostafaee et al. showed that the CVA angle was significantly lower in people with moderate to severe FHP than in people with mild FHP (13). A lower cervical angle in the FHP group indicates more flexion in the lower cervical spine. Also, the upper cervical angle was higher in the FHP group than in the non-FHP group. Higher upper cervical angles in FHP subjects indicate greater cervical spine extension. Both findings are consistent with a study by Kuo et al. Following FHP, the suboccipital muscles contract, shorten and increase in tension, which can cause the upper cervical spine to become more extended (22). Hence, in static conditions, the upper cervical vertebrae are in extension, and the lower cervical vertebrae are in flexion in people with FHP (P-value < 0.001).
On the other hand, the head tilt and posture angles did not differ between the FHP and non-FHP groups. It means that the posture of the head was not different between the groups. Different studies show a great variation in the amounts of the head tilt angle. In non-FHP people, their average has been reported to be 4.4 - 18 degrees (28). Raine and Twomey reported that the head tilt angle in healthy subjects at a standing position was 2.6 ± 2.7 (29). Salahzadeh et al. reported that the head tilt angles as 17.74 ± 4.9 degrees in people with normal head posture and 16.1 ± 5.7 degrees in people with severe FHP, and 15.57 ± 7.72 in people with neck pain (8). Silva et al. showed that the head tilt angle was 0.21 ± 6.4 in people with pain and 18.7 ± 7.7 in people without pain. Also, they stated that the increase in FHP was associated with an increase in head tilt and upper cervical spine extension (28).
Raine and Twomey acknowledged that the amount of the head tilt was not related to the amount of CVA angle in the photographic method, and a decreased CVA angle was not necessarily accompanied by an increased head tilt angle or head extension (29). This study pointed out that the mean head tilt angle was 21.8 ± 30.23 in FHP and 24.7 ± 02.43 in the non-FHP group.
5.2. Quasi-static State
To interpret the results of the quasi-static state, refining the differences in postural angles during the neck motion is necessary. To measure the amount of the ROM of the upper cervical spine, the difference in upper cervical spine angles between the two movement frames has been calculated. Also, this method has been used to measure the lower cervical spine ROM. The CVA angle differences between the two phases of movement mean changing the position of the head relative to the neck. The difference between head tilt angles in the two phases of movement represents changes in the position of the head relative to the horizontal line. The difference in the head posture angle values between the two movement frames reflects the changes in the position of the head relative to the trunk during the neck movement.
According to the present study, during the head and neck flexion and extension movement, the changes in the upper cervical, lower cervical, head posture, and head tilt angles were less in the FHP group than in the non-FHP group. These findings show that in the FHP group, the upper and lower cervical spines' mobility and overall head and neck mobility in both directions (extension and flexion) were decreased. These results are consistent with the findings of Wu et al. and Rudolfsson et al. (11, 15). In the FHP group, when the direction of the cervical spine deviates from the neutral, adaptive shortening of the upper cervical muscles and ligaments occurs. On the other hand, ligament stretching and lower cervical muscle weakness lead to decreased mobility of these parts during the head and neck extension movement (22).
Studies have shown that biomechanical spine disorders, such as FHP, can alter the cervical range of motion, tissue balance, and respiratory efficiency (30-33). In people with neck pain, reducing cervical ROM is a common finding. Therefore, a reduced ROM following FHP may predispose a person to neck pain.
The CVA angle during full flexion to full extension changed more in non-FHP people than in people with FHP. Nevertheless, the changes in returning from full extension to full flexion were more in people with FHP than those with non-FHP. Fewer changes in CVA and head posture angles during extension movements indicated reduced head-to-neck and head-to-trunk mobility in the FHP group, respectively. The measurement of the head tilt angle may represent the upper cervical flexion or extension position.
The CVA angle represents the angle between the eye line and the C7 spine. Head or gaze orientation changes may affect perceived eye-head and head-space orientation due to changes in one's visual field (including peripheral visual inputs). Finally, they may contribute to the fundamental changes in the control of spinal flexion movement. However, directional effects may be produced by gaze alone (34).
5.3. Correlation
It is an interesting finding that in both static and quasi-static states (all movement phases), the correlations between "upper cervical and head posture" angles, "upper cervical and head tilt" angles, and "head posture and head tilt" angles in all participants were strong and positive. Therefore, regardless of the presence or absence of FHP, changes in the upper cervical angle are correlated with changes in the head tilt and head posture angles in the same direction. On the other hand, in static and quasi-static state analyses, measurements of head posture and head tilt may represent the flexion or extension position of the upper cervical spine rather than the FHP. Thus, with the increase in extension in the upper cervical spine, the head tilt and head posture angles increase. According to the more discrimination ability of CVA to detect the FHP (28), head posture angle may not be an accurate variable to measure the FHP. However, it is a good variable to measure the posture of the head relative to the trunk.
In the quasi-static state, the correlations between "lower cervical and craniovertebral" angles, "lower cervical and head tilt" angles, and "CVA and head tilt" angles were positive and strong. This means that more FHP is associated with more flexion positions of the lower cervical spine during movement. This may be due to the increased compression forces on the discs and the anterior part of the spine during neck movement.
5.4. Limitations
They are declared as follows:
(1) The difference in the number of participants with FHP and non-FHP.
Due to the absence of examiner bias, all volunteers participated in the test regardless of whether they had FHP or not.
(2) The use of sequential photography for motion analysis has limitations compared to the motion analysis system because a certain number of frames are captured, and it is impossible to capture all of the moments.
5.5. Suggestions
They are as follows:
(1) Carrying out studies on other societies
(2) Studying an equal or similar number of participants with FHP and non-FHP
(3) Investigating the effect of postural correction exercises for head protrusion according to changes in postural angles compared between the two groups with FHP and non-FHP
5.6. Conclusions
During full flexion to full extension of the neck, subjects with FHP had less mobility in the cervical spine, especially in the lower cervical spine. The position of the head relative to the neck did not change in this group.