1. Background
There has been an upward trend in autism spectrum disorder (ASD) in the recent decade (1). According to global statistics, its prevalence rate has become 20 times higher over the past ten years. The latest statistics indicate that one out of every 68 individuals has autism in the world. Statistics also show that one out of every 65 children is born with ASD in developed countries (2). In Iran, nearly 800 thousand people (i.e., 1% of the population) are estimated to be afflicted with the mild-to-severe spectrum of autism (3). Known as a behavioral syndrome, autism denotes a long-term transformational inability that disrupts a person’s nervous functioning and has significant effects on verbal and nonverbal communication as well as social interactions (4). According to the Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (DSM–5), the symptoms of ASD include difficulty in establishing social communications and interactions, trouble in sensual processing, and repeatedly limited behaviors (5). Symptoms of autism vary greatly in severity; however, all autistic individuals experience defects in social skills (6).
Like their peers, most children with autism love playing with others, having conversations, and blending in with their surrounding communities. Nevertheless, they are unable to automatically perceive the rules of social behaviors, thereby having difficulty establishing communication (7). In need of training, autistic children are unable to use language as a communication tool (8). This inability negatively affects their academic achievements and causes other problems, such as repetitive movements, stereotyped behaviors, and resistance to environmental changes or alterations in the daily life routine (9). Another problem that autistic children experience is difficulty in emotion regulation, a condition that is considered the major problem with these children (10).
The inability to identify emotions in autistic children can make them show self-violence or violent behavior toward others, weakening their social relationships and leading to psychological problems (11). Some studies have reported certain problems in the perception, identification, comprehension, expression, and regulation of emotions in children with ASD (12, 13). Failure in the two-sided social relation is seen as attention deficiency, failure in sharing feelings, self-restraining, and the process of staring at eyes in autistic children (14). As a result, these children miss the opportunities to participate in exciting experiences with others. They manifest instances of immaturity in communication skills, leading to emotion management defects (15, 16). In this regard, some studies have reported that autistic individuals have trouble identifying emotions (10, 17, 18). The main difficulty that individual with ASD experience is that they are unable to perceive people’s complicated psychological states by looking into their eyes (19, 20).
Nature-based play therapy or DIR/floor time play therapy is an approach that can be employed to control and mitigate ASD symptoms (21). Experience with nature in childhood can help a person know and value nature and try to protect the environment in the future (22). Playing with natural elements such as trees, flowers, soil, water, and animals can boost different stages of children’s development (23). Children with failure to thrive show further social skills and more empathetic behaviors in the presence of animals (24). The use of natural environments and animals to help autistic children will enhance their relationships with others. Making contact with animals and natural environments can be effective in drawing children’s attention and concentration (25). The complete perception of childhood experiences would necessitate knowing and paying attention to the physical and biological environments where a child exists (26). Nature is among the most important realms with which children deal in their most sensitive years of life. Autistic children can experience more stimulation and higher concentration by being present in nature and staying in contact with animals in order to become more aware of the surrounding environment (27). It is also difficult for autistic individuals to learn formal education programs and acquire social skills. The DIR/floor time play therapy can be employed to help these children. According to Ramshini et al. (28), nature-based child-oriented play therapy can improve attention and alleviate aggression in children with ASD. Divya et al. (29) reported that DIR/floor time play therapy can be effective in improving social and emotional development among children with ASD.
The inabilities caused by ASD are severe, pervasive, and dynamic, making autistic children and their parents experience numerous problems in different areas, such as stress, parenting self-efficacy, mental health and physical health of parents, marital relationships, and familial welfare in general. According to the background of the research, the application of DIR/floor time play therapy may be effective in improving the social skills and emotional regulation of children with ASD, which is one of the main problems of these children. What highlights the importance of the current research is that it is not possible to find research that has determined the effectiveness of DIR/floor time play therapy on social skills and emotional regulation in children with ASD.
2. Objectives
In this study, we aimed to investigate the effectiveness of DIR/floor time play therapy in the social skills and emotion regulation of children with ASD.
3. Methods
3.1. Design and Participants
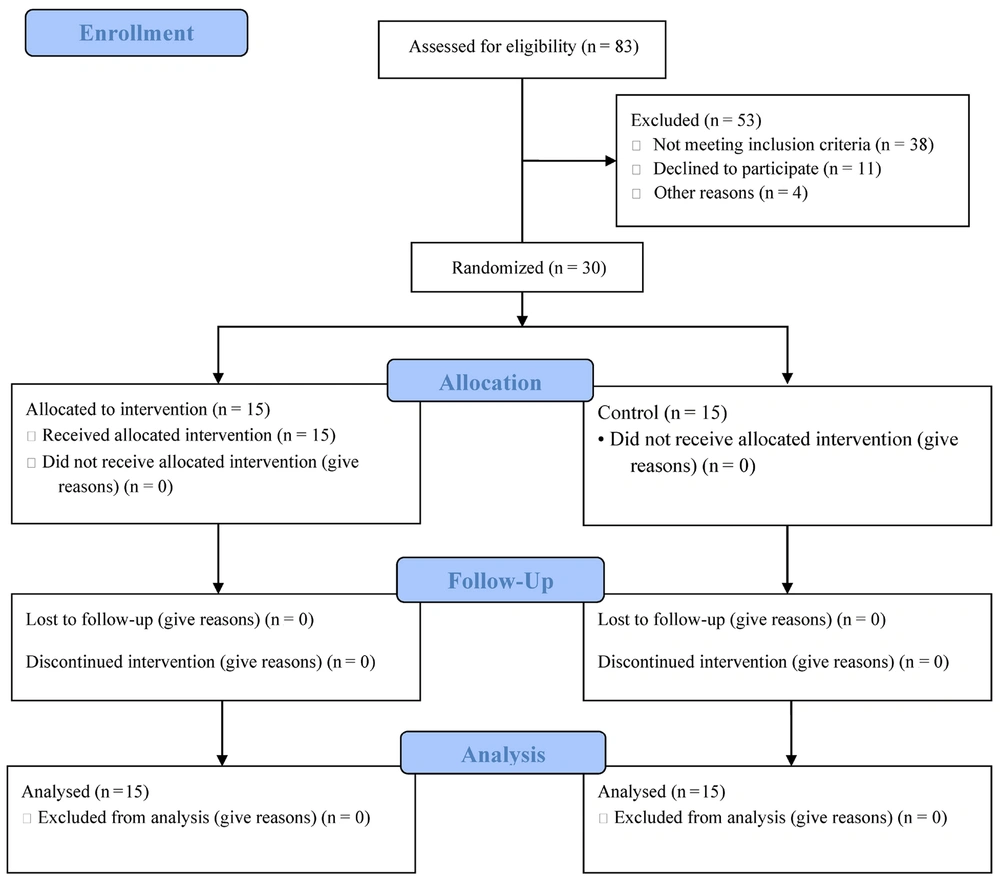
The present study was quasi-experimental with a pretest/posttest design. After the necessary permits were acquired, the research samples were selected from the children with ASD who visited Golhay-e Behesht Autism Center in Qom, Qom Province (Iran) in 2022. Parental consent was obtained before sampling, for which the convenience sampling method was adopted to select 30 autistic children, who were randomly assigned to an experimental group (n = 15) and a control group (n = 15) (Figure 1). The sample size was selected based on G*Power with a test power of 0.8, a significance level of 0.05, and a 90% effect size (30). The experimental group received the DIR/floor time play therapy intervention for 23 twenty-minute sessions. The inclusion criteria were as follows: Being diagnosed with autism level 1 based on diagnostic criteria (Diagnostic and Statistical Manual of Mental Disorders (DSM-5)) and a psychiatrist’s discretion, having an IQ above 85 based on the child's health record, having no other developmental disorders, and being aged 7 – 10 years old. The exclusion criteria were as follows: Developmental disorders, children with ASD levels 2 and 3, taking anticonvulsants and epilepsy drugs, unwillingness to participate in therapy sessions, being absent for more than two sessions and having a history of concurrent participation in the interventions used in this study. The contents of games were designed to allow children to have the most active role so that the therapist would act more as a guide in sessions. After the intervention was over, post-test analyses were conducted on the experimental group and the control group. The follow-up was implemented after two months.
3.2. Intervention
The intervention of DIR/floor time play therapy was implemented by the first author with the help of parents of children with ASD at Golhay-e Behesht Autism Center in Qom. The first author had already completed the training courses and workshops for this treatment. The DIR/floor time play therapy is a child-oriented approach, with therapist-led sessions and parental support. In therapy sessions, a therapist tries to open communication windows toward a child through interesting games. There are different instances of activities in the DIR/floor time play therapy model: Passing through a tunnel (i.e., a child is instructed how to move a toy car on the ground. A tunnel is made by using the other toys. The child is encouraged to take the toy car into the tunnel and move to pass it through), reading books (i.e., a book that the child liked was selected. The actions and reactions in the book such as sounds and contacts were prepared to improve the child’s experiences), playing with balls, matching colors, house building, dancing together, taking combinatorial steps, and doing puzzles (31).
3.3. Instruments
The Autism Social Skills Profile (ASSP): Designed by Bellini and Hopf (32), this 48-item questionnaire is scored on a four-point Likert scale (i.e., 1= “never”, 2= “sometimes”, 3= “often”, and 4= “always”). Higher scores correspond to appropriate and positive social behaviors. Most of the items were designed as positive behaviors, whereas some others were designed as negative behaviors and scored inversely. This scale applies to 5–17-year-old individuals. An informed individual (i.e., parents, teachers, or therapists) requires 15 – 20 minutes to complete this tool based on children’s behaviors. This profile consists of three subscales, including social interaction skills, social participation, and socially detrimental behavior. The total score is obtained from the social functioning of an autistic child or adolescent (32). Ashori and Jalil-Abkenar (33) reported an alpha Cronbach coefficient of 0.85 for the Persian version of ASSP.
Emotion Regulation Checklist (ERC): Designed by Shields and Cicchetti (34), this 24-item checklist is employed to evaluate the emotion regulation of 5–12-year-old children. The ERC measure targets such processes as affective lability, intensity, valence, flexibility, and situational appropriateness. The checklist includes both positively and negatively weighted items to be rated on a 4-point Likert scale. This checklist can be completed by adults who know the targeted child really well (e.g., parents, caretakers, or teachers) (34). Meybodi et al. (35) reported an alpha Cronbach coefficient of 0.74 for the Persian version of the ERC.
3.4. Statistical Analyses
The Shapiro–Wilk test was conducted to test the normality of data distribution, whereas Levene’s test was employed with Mauchly’s test of sphericity to analyze the homogeneity of error variances. Descriptive statistics and the repeated measures ANOVA were adopted for data analysis in SPSS 22. The significance level of the research was considered to be α = 0.05.
4. Results
The autistic children were divided into a DIR/floor time play therapy group (consisting of 6 girls and 9 boys) and a control group (including 7 females and 8 males). The mean age of children was 7.65 ± 2.61 years old in the DIR/floor time play therapy group, whereas it was 7.44 ± 2.84 years old in the control group. The mothers of three, ten, and two participants in the DIR/floor time play therapy group had junior high school education, senior high school education, and academic degrees, respectively. The mothers of two, 12, and one participant in the control group had junior high school education, senior high school education, and academic degrees, respectively (Table 1).
| Groups | Age, y | Gender | Education | |||
|---|---|---|---|---|---|---|
| Females | Males | Junior High School | Senior High School | Academic Education | ||
| DIR/floor time play therapy group | 7.65 ± 2.61 | 6 (40.0) | 9 (60.0) | 3 (20.0) | 10 (66.7) | 2 (13.3) |
| Control group | 7.44 ± 2.84 | 7 (46.7) | 8 (53.3) | 2 (13.3) | 12 (80.0) | 1 (6.7) |
a Values are expressed as mean ± SD or No (%).
According to the results of descriptive data, the mean scores of instability/negativity and socially detrimental behaviors in the experimental group decreased in the post-test and follow-up steps (P < 0.001). However, the mean scores of emotion regulation, social interaction, and social participation increased (P < 0.001). The results indicated that there were significant differences between the mean scores of emotion regulation and social skills in the pretest–posttest and posttest–follow-up steps (P < 0.001). However, there were no significant differences between their mean scores in the posttest–follow-up steps (Table 2).
| Variables | Floortime Play Therapy Group, Mean ± SD | Control Group, Mean ± SD | P-Value |
|---|---|---|---|
| Emotion Regulation | |||
| Instability/negativity | |||
| Pretest | 45.00 ± 6.83 | 44.40 ± 6.50 | 0.807 |
| Posttest | 32.20 ± 4.80 | 43.13 ± 7.03 | 0.001 |
| Follow-up | 31.20 ± 5.63 | 42.00 ± 6.59 | 0.001 |
| Emotion regulation | |||
| Pretest | 13.73 ± 3.01 | 13.07 ± 2.74 | 0.535 |
| Posttest | 19.00 ± 3.62 | 13.27 ± 2.63 | 0.001 |
| Follow-up | 19.33 ± 3.77 | 13.73 ± 3.58 | 0.001 |
| Social Skills | |||
| Social interaction | |||
| Pretest | 36.33 ± 6.74 | 38.80 ± 8.23 | 0.386 |
| Posttest | 53.33 ± 7.63 | 40.70 ± 8.25 | 0.001 |
| Follow-up | 54.00 ± 7.91 | 39.07 ± 7.85 | 0.001 |
| Social participation | |||
| Pretest | 30.67 ± 7.08 | 30.93 ± 7.41 | 0.922 |
| Posttest | 43.20 ± 8.21 | 31.53 ± 7.31 | 0.001 |
| Follow-up | 45.67 ± 7.76 | 32.33 ± 6.32 | 0.001 |
| Detrimental behaviors | |||
| Pretest | 42.67 ± 8.08 | 43.20 ± 7.23 | 0.851 |
| Posttest | 26.13 ± 6.27 | 43.80 ± 7.87 | 0.001 |
| Follow-up | 25.20 ± 5.49 | 45.60 ± 8.89 | 0.001 |
The Shapiro–Wilk test results indicated the normal distribution of data. According to Levene’s test, there were no significant differences in the error variances of scores for any components of emotion regulation and social skills in both groups and all three implementation steps. Hence, the error variances of data were homogenous. Finally, Mauchly’s test of sphericity indicated that no Chi-squared values of emotion regulation and social skills were significant. This finding showed that the sphericity hypothesis was confirmed for the components of both dependent variables.
Table 3 reports the repeated measures ANOVA to compare the effects of the DIR/floor time play therapy on the components of emotion regulation and social skills. According to the results, the interactive effect of group × time was significant on the component of instability/negativity and the component of emotion regulation. Moreover, the interactive effect of group × time was significant on the components of social interaction, social participation, and detrimental behaviors.
| Variables and Sources | MS | F | P-Value | |
|---|---|---|---|---|
| Instability/negativity | ||||
| Group | 1656.89 | 18.07 | 0.001 | 0.45 |
| Time | 1677.47 | 43.19 | 0.001 | 0.51 |
| Group × time | 3379.78 | 4.53 | 0.002 | 0.17 |
| Emotion regulation | ||||
| Group | 578.40 | 13.89 | 0.001 | 0.40 |
| Time | 366.67 | 31.37 | 0.001 | 0.43 |
| Group × time | 586.27 | 5.15 | 0.001 | 0.20 |
| Social interaction | ||||
| Group | 2325.02 | 14.76 | 0.001 | 0.41 |
| Time | 3023.33 | 32.80 | 0.001 | 0.44 |
| Group × time | 5414.98 | 5.54 | 0.001 | 0.21 |
| Social participation | ||||
| Group | 3171.44 | 10.36 | 0.001 | 0.33 |
| Time | 1945.60 | 45.39 | 0.001 | 0.52 |
| Group × time | 3910.22 | 5.20 | 0.001 | 0.20 |
| Detrimental behaviors | ||||
| Group | 2687.87 | 31.87 | 0.001 | 0.60 |
| Time | 2081.53 | 35.51 | 0.001 | 0.46 |
| Group × time | 4108.27 | 9.45 | 0.001 | 0.31 |
5. Discussion
The present study aimed to investigate the effectiveness of DIR/floor time play therapy in the social skills and emotion regulation of children with ASD. According to the research results, the DIR/floor time play therapy made significant differences between the posttest and pretest scores of emotion regulation and social skills in the experimental group. The results also indicated that the autistic children of the experimental group who received the DIR/floor time play therapy sessions had better emotional functions and social interactions than those of the control group. In line with the findings of this study, Elbeltagi et al. (22) reported that play therapy helps children with ASD to experience feeling out various interaction styles. In addition, Tilmont-Pittala et al. (26) reported that play therapy improved the social and communication interactions of children with ASD.
We can argue that play therapy interventions will change the social behaviors of autistic children. The findings also indicate that acquiring play skills in the early stages of life can exacerbate challenging behaviors in autistic children. Therapists use games to teach more adaptive behaviors to autistic children with poor social or emotional skills (22). Play therapy is the best form of counseling intervention for children. In this type of intervention, children can express their worries in a psychologically secure environment, practice new skills, and discover creative solutions to their challenges to overcome difficult situations (26). In play therapy, children with autism can express their emotions and fears. This intervention also helps them develop their ability to analyze structures and emotions. Play therapy is considered a kind of assistance for a learning environment and also an experience that helps children maximize their learning opportunities and social communications (27). In this method, a play therapist uses different tools such as painting, flashcards, handcrafts, or display games to help children express their feelings without giving direct verbal explanations.
Children with ASD are innately characterized by failure to establish initial communications, have social interactions, and start learning new things. This failure may affect their interactions with peers (4). In mixed environments where autistic children participate in premature development plans alongside normal children, autistic children usually play in solitary. Playing, interacting, and cooperating with peers can provide fundamental experiences for children to develop and improve their communication skills; hence, they can acquire communication skills and verbal skills (26). Play therapy methods were designed to solve children’s verbal, sensual, and emotional problems. In play therapies, children can express their emotions naturally through interactions with their parents (27). In fact, play therapy techniques can directly help autistic children to learn skills. Parents can also learn how to employ these techniques at home.
This study faced certain limitations, such as the small number of research samples, including only the autistic children of Qom, Qom Province (Iran). Therefore, caution should be taken into account in the generalization of results. For future research, it is suggested to conduct DIR/floor time play therapy for other children with mental disorders. It is suggested that this therapeutic intervention be investigated on other psychological characteristics of children with ASD. Also, in future research, it is suggested to use interviews in addition to questionnaires to collect data.
5.1. Conclusions
In general, the findings of this study indicated that the DIR/floor time play therapy mitigated challenging behaviors in children’s social interactions, emotion regulation, and negativity. It is suggested that special education officials and authorities at the State Welfare Organization of Iran arrange DIR/floor time play therapy training courses for teachers, instructors, and therapists involved with autistic children. It is also suggested that DIR/floor time play therapy should be implemented constantly and regularly as rehabilitation and therapy services at the centers and schools dedicated to children with ASD in order to mitigate many of their problems.