1. Background
The recent coronavirus disease 2019 (COVID-19) outbreak and its rapid worldwide spread have represented a global health emergency affecting many countries and millions of people. The new virus, which is believed to be a member of the Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS) family of coronaviruses, is a unique RNA virus strain that has not been previously observed in humans (1). Researchers have demonstrated several risk factors that may contribute to the severity of this disease. The World Health Organization (WHO) suggests that older people, as well as people with underlying diseases, are at higher risk of developing more severe forms of COVID-19 (2). Several epidemiologic and clinical studies have shown that the majority of deaths in patients with COVID-19 are related to underlying diseases such as diabetes, hypertension, kidney failure, etc., and that patients have a compromised immune system (3).
Some studies show that people with diabetes and hypertension have a higher risk of being infected with this virus and a higher risk of COVID-19 complications and deaths (4, 5). In the United States, of patients over 65 years old who had a higher risk of dying from COVID-19, 26.8% suffered from type 2 diabetes, and hypertension was present in 68.4% of the people with diabetes (6). A large cohort study conducted in Catalonia that included data from 118,150 patients with COVID-19 showed that the prevalence of diabetes in the affected population was 9.3%, and 14.8% of patients in this group required hospitalization in the first month after infection (7).
Although data on the presence of diabetes in patients with COVID-19 requiring hospitalization have been reported from different countries, the most common associated phenotype is advanced age (over 60 years) (8). Clearly, metabolic diseases such as hypertension, diabetes, obesity, heart disease, and cerebrovascular disease are very common in these people (9, 10). In studies conducted in China, the presence of hypertension was found in 27 - 30% of patients with COVID-19, while other comorbidities such as diabetes and coronary heart disease were observed in 19% and 6 - 8% of patients, respectively (11). Hypertension and heart disease associated with diabetes were the most common comorbidities in critically ill patients admitted to the intensive care unit (ICU) who required mechanical ventilation or died, compared with patients with only mild disease (4, 11, 12).
2. Objectives
This study was conducted to investigate the association between the history of diabetes and hypertension and the novel COVID-19 patient’s clinical findings and length of hospital stay admitted to Motamedi Hospital in Garmsar, Iran.
3. Methods
In this descriptive-analytical and practical cross-sectional study, the statistical population included patients hospitalized from May to September 2019 with a definite diagnosis of COVID-19 based on radiology, CT scan, or reverse transcription polymerase chain reaction (RT-PCR) findings in Motamedi Hospital of Garmsar, Iran. Data collection was done after approving the plan and obtaining approval from the Ethics Committee of Semnan University of Medical Sciences (ethical code: IR.SEMUMS.REC.1399.114). Symptoms and manifestations of disease, demographic information, recovery time, and other clinical findings such as the results of chest radiography, CT scan, and blood tests were extracted from the patient's data and recorded in the data collection forms. Finally, the patients were divided into 3 groups:
(1) Patients with a positive diagnosis of COVID-19 and a history only hypertension
(2) Patients with a positive diagnosis of COVID-19 and a history of diabetes and hypertension
(3) Patients with a positive diagnosis of COVID-19 without any underlying disease
After collecting the data, they were analyzed using Minitab V17 software. The analysis of variance (ANOVA) test was performed to describe the data by mean and standard deviation and to analyze the variables due to the significant level of P < 0.05. The Pearson and Spearman correlation coefficients were used for quantitative and qualitative variables, respectively.
The inclusion criteria included confirmed cases of COVID-19 with a positive CT scan/positive CRP test/positive PCR test and a history of hypertension and diabetes confirmed by an endocrinologist. Pregnancy, breastfeeding, other pneumonia types, alcohol consumption in the past 5 years, addiction, and active cancer were the exclusion criteria.
4. Results
4.1. Age and Sex Distribution
Of the 69 patients studied, 25 were in the hypertension group, 21 were in the diabetes + hypertension group, and 23 people were in the group without underlying diseases (control). Table 1 shows the age distribution of patients in the studied groups. In the hypertension group and diabetes + hypertension group, most of the patients were in the age range of 61 - 80 years, and in the control group, they were in the age range of 41 - 60 years. The average age was 66.84 years in the hypertension group, 67.10 years in the diabetes + hypertension group, and 49.04 years in the control group. Tukey's analysis showed that the average age was significantly (P = 0.000) higher in the hypertension group and the diabetes + hypertension group than in the control group (Table 2). As can be seen, the age range of the studied patients was wide, which can be due to the fact that hypertension and diabetes are more frequently seen in the elderly. Therefore, patients without these diseases (the control group) were younger.
| Age Category (y) | Groups (%) | ||
|---|---|---|---|
| Hypertension | Hypertension + Diabetes | Control | |
| 20 - 40 | 8.00 | 0.00 | 30.43 |
| 41 - 60 | 16.00 | 19.05 | 43.48 |
| 61 - 80 | 56.00 | 71.43 | 17.39 |
| 81 - 100 | 20.00 | 9.52 | 8.70 |
| Total | 100 | 100 | 100 |
| Groups | Number | Average | Standard Deviation | Standard Error | First Quartile | Third Quartile | Minimum | Maximum | Statistical Indicators | |
|---|---|---|---|---|---|---|---|---|---|---|
| F Value | P Value | |||||||||
| Hypertension | 25 | 66.84 | 15.23 | 3.05 | 59.0 | 78.0 | 38 | 92 | 12.27 | 0.000 |
| Hypertension + diabetes | 21 | 67.10 | 10.57 | 2.31 | 62.0 | 73.0 | 43 | 89 | ||
| Control | 23 | 49.04 | 15.71 | 3.27 | 37.0 | 61.0 | 29 | 85 | ||
Also, statistical analysis showed that the frequency distribution of gender was not significantly different between the three groups of patients (P = 0.943).
4.2. Symptoms
The most common disease symptoms in all patients were weakness, lethargy, shortness of breath, fever, and chills. The loss of consciousness was statistically significantly lower in the control group than in the other groups (P = 0.039). However, Pearson's chi-square index of 0.24 and P value of 0.742 showed that there was no relationship between the occurrence of early symptoms of patients with COVID-19 in people with different underlying diseases and also in the control group (Table 3). A pairwise comparison between the groups showed a statistically significant difference in the incidence of loss of consciousness between the diabetes + hypertension group and the control group (P value = 0.039). However, there was no significant difference between the hypertension group and the diabetes + hypertension group.
| Early Symptoms | Groups | Statistical Indicators (P-Value) | ||
|---|---|---|---|---|
| Hypertension | Hypertension + Diabetes | Control | ||
| Fever and chills | 72.0 | 71.4 | 65.2 | 0.857 |
| Nausea and vomiting | 40.0 | 38.1 | 21.7 | 0.349 |
| Loss of consciousness | 16.0 | 33.3 | 4.3 | 0.039 |
| Weakness and lethargy | 100.0 | 95.2 | 95.7 | 0.555 |
| Shortness of breath | 84.0 | 76.2 | 82.6 | 0.778 |
| Low blood pressure | 16.0 | 14.3 | 21.7 | 0.788 |
4.3. Laboratory and Clinical Parameters
Table 4 compares the results of CRP and ESR tests, O2 saturation, body temperature, and blood pressure. The number of CRP-positive cases was higher in the hypertension group (90 ± 50.9) and diabetes + hypertension group (80.45 ± 37.39) than in the control group (61.87 ± 44.46), but this difference was not statistically significant. The P-values in Table 4 show that ESR (P = 0.016), saturated blood oxygen (P = 0.012), and blood pressure (P = 0.002) were statistically different between the groups. A pairwise comparison between the groups showed that the ESR level was significantly lower (P = 0.006) in the control group than in the hypertension + diabetes group, and the O2 saturation level was significantly higher (P = 0.0024) than in the hypertension group. As expected, the blood pressure level was significantly lower in the control group than in the hypertension group (P = 0.0016) and the hypertension + diabetes group (P = 0.0039). However, in terms of the highest body temperature (fever), there was no significant difference between the groups (P = 0.0670).
| Groups | Statistical Indicators (P Value) | |||
|---|---|---|---|---|
| Hypertension | Hypertension + Diabetes | Control | ||
| ANOVA test results (SD ± mean) | ||||
| CRP | 90.1 ± 50.9 | 80.45 ± 37.39 | 61.78 ± 44.46 | 0.102 |
| Kruskal-Wallis non-parametric test results (median) | ||||
| ESR | 38.5 | 56.0 | 27.0 | 0.016 |
| Sat O2 | 88.0 | 87.5 | 88.0 | 0.012 |
| Highest body temperature | 37.5 | 37.5 | 37 | 0.67 |
| Highest blood pressure | 140.9 | 145.8 | 130.7 | 0.002 |
4.4. CT Scan Reports
The CT scan reports of the patients were reviewed for the presence of acute respiratory distress syndrome (ARDS). Also, 80% of the patients in the hypertension group, 76.2% in the diabetes + hypertension group, and 69.6% in the control group had ARDS. Although the level of respiratory distress was lower in the control group than in the groups with underlying diseases, there was no statistically significant difference (P = 0.7) (Table 5).
| Lung CT Scan Reports | Groups | Statistical Indicators | |||
|---|---|---|---|---|---|
| Hypertension | Hypertension + Diabetes | Control | P-Value | Pearson Chi-Square Index | |
| ARDS | 80.0 | 76.2 | 69.6 | 0.714 | 0.700 |
| Healthy | 20.0 | 23.8 | 30.4 | ||
| Total | 100 | 100 | 100 | ||
4.5. Prescribed Medications
Table 6 shows the frequency distribution of the drugs used to treat COVID-19 and the underlying diseases in different groups. Systemic corticosteroids, antivirals, anticoagulants, antibiotics, and antipyretics were prescribed for COVID-19.
| Drugs | Groups | ||
|---|---|---|---|
| Hypertension | Hypertension + Diabetes | Control | |
| Antiviral | |||
| ReciGen | 40.0 | 47.6 | 26.1 |
| Kaletra | 12.0 | 9.5 | 13.0 |
| Remdesivir | 44 | 28.6 | 52.2 |
| Favipiravir | 0.0 | 4.8 | 4.3 |
| Digestive | |||
| Pantoprazole | 80.0 | 71.4 | 91.3 |
| Ondansetron | 16.0 | 14.3 | 8.7 |
| Magnesium syrup | 0.0 | 4.8 | 0.0 |
| Clidinium C | 4.0 | 0.0 | 0.0 |
| Dimethicone | 4.0 | 0.0 | 0.0 |
| Lactulose | 4.0 | 0.0 | 0.0 |
| Antibiotics | |||
| Ceftriaxone | 16.0 | 9.5 | 13.0 |
| Vancomycin | 0.0 | 23.8 | 4.3 |
| Meropenem | 4.0 | 28.6 | 0.0 |
| Ceftazidime | 0.0 | 4.8 | 0.0 |
| Cefazolin | 4.0 | 0.0 | 0.0 |
| Antipyretic and analgesic | |||
| Apotel | 52.0 | 52.4 | 69.6 |
| Cortone | |||
| Dexamethasone | 72.0 | 57.1 | 73.9 |
| Betamethasone | 0.0 | 0.0 | 4.3 |
| Hydrocortisone | 0.0 | 4.8 | 4.3 |
| Prednisolone | 20.0 | 14.3 | 0.0 |
| Anti-asthma | |||
| Salbutamol spray | 4.0 | 9.5 | 8.7 |
| Fluticasone | 4.0 | 0.0 | 0.0 |
| Betamethasone spray | 0.0 | 4.8 | 0.0 |
| Beclomethasone spray | 4.0 | 4.8 | 0.0 |
| Anticoagulant | |||
| Enoxaparin (selexan) | 44.0 | 42.9 | 73.9 |
| Heparin | 40.0 | 28.6 | 0.0 |
| Plavix | 4.0 | 0.0 | 0.0 |
| Aspirin | 16.0 | 19.0 | 0.0 |
| Anti-hypertension | |||
| Metoprolol | 8.0 | 9.5 | 4.3 |
| Lasix | 12.0 | 9.5 | 4.3 |
| Amlodipine | 8.0 | 4.8 | 4.3 |
| Losartan | 52.0 | 38.1 | 0.0 |
| Captopril | 8.0 | 4.8 | 0.0 |
| Hydrochlorothiazide | 4.0 | 0.0 | 0.0 |
| Antipsychotic benzodiazepine and anti-anxiety | |||
| Clonazepam | 0.0 | 0.0 | 4.3 |
| Lorazepam | 4.0 | 0.0 | 0.0 |
| Oxazepam | 4.0 | 0.0 | 0.0 |
| Diabetes | |||
| Insulin | 0.0 | 47.6 | 0.0 |
| Metformin | 0.0 | 4.8 | 0.0 |
| Antitussive | |||
| Dextromethorphan | 12.0 | 0.0 | 0.0 |
| Blood fat | |||
| Atorvastatin | 12.0 | 23.8 | 0.0 |
| Nitroglycerin | |||
| Nitrocontin | 4.0 | 0.0 | 0.0 |
| Antihistamine | |||
| Chlorpheniramine | 0.0 | 0.0 | 4.0 |
| Hyperkalemia | |||
| Potassium oxalate | 0.0 | 4.8 | 0.0 |
| Inotrope | |||
| Digoxin | 0.0 | 4.8 | 0.0 |
| Anticonvulsant | |||
| Midazolam | 4.0 | 0.0 | 0.0 |
| Anti-inflammatory | |||
| Actemra | 8.0 | 4.8 | 0.0 |
| Vasopressor | |||
| Epinephrine | 4.0 | 0.0 | 0.0 |
| Beta-blocker | |||
| Propranolol | 4.0 | 0.0 | 0.0 |
| Supportive treatment | |||
| Vitamin C | 8.0 | 0.0 | 0.0 |
| Vitamin D | 4.0 | 0.0 | 0.0 |
| Sodium valproate | 4.0 | 0.0 | 0.0 |
As expected, the hypertension and hypertension + diabetes groups used antihypertensive and blood lipid-lowering drugs more frequently than the control group. Also, insulin and metformin were prescribed only for diabetic patients.
4.6. Other Treatment Methods
Table 7 shows the frequency distribution of oxygen therapy and the use of mechanical ventilation in the three groups. Most of the patients needed oxygen therapy in all groups, but none of them in the control group required mechanical ventilation. The Pearson chi-square index of 4.238 and P value of 0.120 showed no relationship between the treatment method of the COVID-19 patients with underlying diseases and the control group.
| Treatment Methods | Groups (%) | Statistical Indicators (P Value) | ||
|---|---|---|---|---|
| Hypertension | Hypertension + Diabetes | Control | ||
| Oxygen therapy | 88.0 | 81.0 | 73.9 | 0.459 |
| Mechanical ventilation | 20.0 | 19.1 | 0.0 | 0.075 |
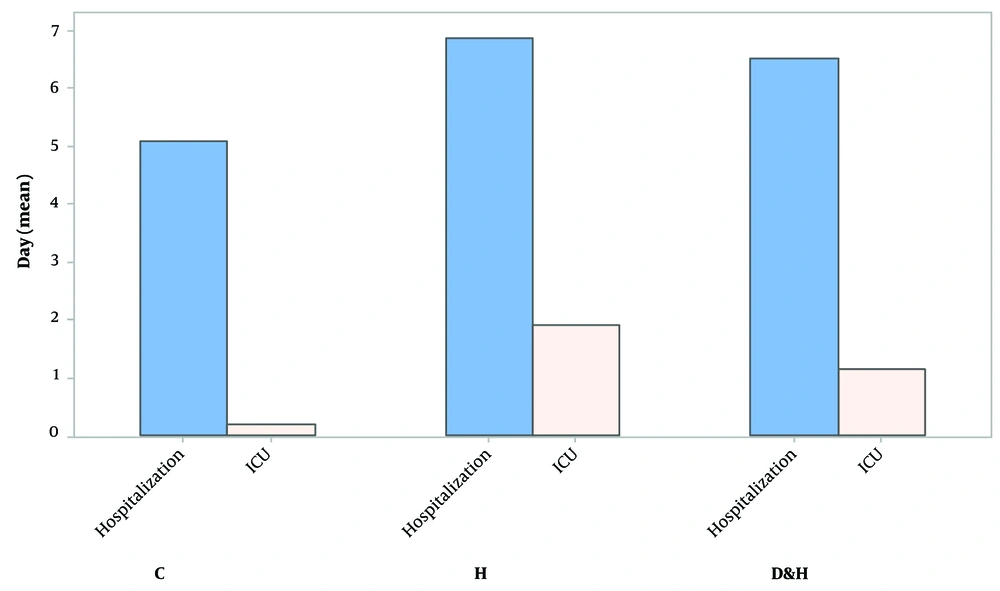
4.7. Duration of Hospitalization and Death Rate
Table 8 and Figure 1 show the results of statistical analysis comparing the length of hospital stay between different groups of COVID-19 patients. The duration of hospitalization was relatively lower in the control group than in the other groups with underlying diseases. Nevertheless, this difference was not statistically significant (P = 0.068) at the 95% confidence level. Meanwhile, none of the patients needed hospitalization in the ICU. Moreover, the mortality rate was higher in the hypertension group and diabetes + hypertension group than in the control group. However, this difference was not statistically significant (P = 0.18).
| Groups (Median) | Statistical Indicators (P Value) | |||
|---|---|---|---|---|
| Hypertension | Hypertension & Diabetes | Control | ||
| Hospitalization period (days) | 6 | 5 | 4 | 0.068 |
| Length of stay in ICU (days) | 0 | 0 | 0 | 0.247 |
5. Discussion
As a public health crisis, COVID-19 was first reported in China but soon affected many regions of the world. The virus accesses host cells through angiotensin-converting enzyme 2 (ACE2), which is highly expressed in the lung (13). Of course, this receptor is also provided by endothelial cells. Studies show that the elderly have a higher risk of prolonged hospitalization, admission to the intensive care unit, and death from COVID-19 (14). On the other hand, increasing age is related to various underlying diseases, and the severity of the disease caused by COVID-19 may be related to the underlying diseases (15).
Hypertension is a common and chronic disease associated with age and a major risk factor for heart disease and stroke. Treatment of high blood pressure with ACE inhibitors can increase the expression of the ACE2 gene and, as a result, facilitate the entry of the coronavirus into target cells and SARS-CoV into the respiratory system. Therefore, the potential increase in ACE2 in the airway tissue of hypertension patients after treatment with RAS blockers may contribute to an increased risk of SARS-CoV-2 infection and possibly a more severe course of COVID-19 (11). One of the largest studies on blood pressure and coronavirus was conducted by Zhou et al. between December 1, 2019, and January 29, 2020, in 1 099 hospitalized and non-hospitalized patients with a positive COVID-19 test. In this cohort study, 165 patients (15%) had hypertension (11). The authors also examined the severity of the disease, the outcome of hospitalization in the ICU, the need for mechanical ventilation, and the death of the patients. Their results indicated that 23.7% of patients with high blood pressure showed severe disease, 35.8% required ICU hospitalization and mechanical ventilation, and finally, death was reported in this group. In another similar study in China, 58 (30%) cases had hypertension, and 26 (48%) patients died from the disease, while 32 (23%) survived (11).
Another chronic disease that is common in the elderly is diabetes mellitus. This is a series of diseases characterized by high blood glucose levels, in which genetic and environmental factors play an important role (8). Several factors are affected by hyperglycemia, such as impaired glucose-dependent pulmonary function, increased inflammatory response, dysregulation of the renin-angiotensin system, dysfunction of immunoglobulins, increased coagulation activity, increased risk of bacterial infections, and direct damage to the pancreas (13). In addition, glucose in lung epithelial cells in diabetic patients significantly increases the risk of influenza virus infection, and the increase in glucose levels disrupts the antiviral immune response (14). Diabetes is associated with several structural changes in the lung, including increased pulmonary vascular permeability and alveolar epithelial breakdown, and the respiratory dysfunction caused by COVID-19 is exacerbated in patients with diabetes. While restoration of normal blood glucose levels appears to be associated with a better prognosis in bacterial infections and viral diseases, especially COVID-19, the effect of anti-hyperglycemic treatments on the outcomes of this disease is still under investigation (15).
Diabetes is one of the causes of high blood pressure. In other words, these patients are more susceptible to hypertension than other patients. These two diseases are also important risk factors for atherosclerosis and have a synergistic effect on the development of cardiovascular damage (15). The prevalence of diabetes and hypertension in patients with COVID-19 has been reported in various studies. The prevalence ranges from 9.7% to 11.9% for diabetes and 17.1% to 20% for hypertension. Most studies showed an association between mortality and ICU hospitalization (5, 16).
In the present study, we compared the clinical findings, length of hospital stay, and mortality rates between three groups of patients with diabetes, diabetes + hypertension, and without underlying diseases who were infected with COVID-19. Of the 69 patients studied who met the conditions for participation in the study, 25 were in the group with hypertension, 21 were in the group with diabetes + hypertension, and 23 were in the group without underlying diseases (control group). As expected, the mean age was significantly higher in the groups with hypertension and diabetes + hypertension than in the control group; however, the frequency distribution of sex was not significantly different between the three groups.
The most common symptoms of illness included weakness and lethargy, shortness of breath, fever, and chills. The decrease in the level of consciousness was statistically significantly lower in the control group than in the other groups. However, there was no significant difference in the occurrence of the initial symptoms of COVID-19 between the different studied groups. Statistically, there was a significant difference in the frequency of loss of consciousness between the diabetes + hypertension group and the control group. However, there was no significant difference between the hypertension group and the diabetes + hypertension group. In most previous studies, fever and cough were the main symptoms of the disease, and digestive symptoms were reported less (11, 17).
Biological factors such as CRP, ferritin, lactate dehydrogenase, and ESR increase significantly in infectious diseases such as COVID-19 (15). A study in China showed that the levels of CRP, ferritin, IL6, and coagulation factors were higher in diabetic patients with COVID-19 than in non-diabetic patients (16). In the present study, the rate of CRP-positive cases was higher in the hypertension and diabetes group than in the control group, but it was not statistically significant. Of course, there were statistical differences between the groups in ESR, saturated blood oxygen, and blood pressure. A pairwise comparison between the groups showed that ESR was significantly lower in the control group than in the hypertension and diabetes groups, and O2 saturation was higher than in the hypertension group. As expected, blood pressure was significantly lower in the control group than in the hypertension group and the hypertension + diabetes group, but there was no significant difference between the groups in terms of the highest body temperature (fever).
Patients' CT examination reports were reviewed for the presence of ARDS. Also, 80% in the hypertension group, 76.2% in the diabetes + hypertension group, and 69.6% in the control group were reported to have ARDS. Although the extent of respiratory distress was less in the control group than in the groups with underlying diseases, there was no statistically significant difference.
Most patients required oxygen therapy, but none of the patients in the control group required mechanical ventilation. There was no association between the treatment methods of patients with COVID-19 in people with underlying diseases and in the control group. Regarding drug treatment, the proportion of antibiotics was higher in the groups with underlying diseases.
In a study in Singapore, of 717 COVID-19-positive individuals, 139 (19.4%) had hypertension, and 76 (10.6%) had type 2 diabetes. In the hypertension group, the use of ACE-I inhibitors was associated with a lower risk of ICU admission and mechanical ventilation (18, 19).
A systematic review examining 7 studies of the association of COVID-19 with diabetes and hypertension showed that diabetes was lower in the survivors and non-severe patients. No association of diabetes was found with ICU care, but blood pressure was positively related to death, ICU hospitalization, and severity of illness (16).
In our study, we compared the length of hospital stay in patients with COVID-19 between the studied groups. Although the length of hospital stay was relatively lower in the control group than in the groups with underlying diseases, this difference was not statistically significant. In addition, none of the patients studied required the intensive care unit stay.
In a study conducted by Wargny et al. in France, diabetic people with COVID-19 were followed for 28 days. Fifty percent of patients were discharged within 9 days, but 20% died. The average CRP level of the patients was 86 mg/L (40 - 148), and this high level was associated with a reduction in the patients' discharge time (20).
In our study, the mortality rate was 16% in the hypertension group, 23% in the diabetes + hypertension group, and 4% in the group without underlying disease. These values are similar to other studies. However, these differences were not statistically significant in our study. We believe that a larger sample size is needed to obtain meaningful results.
In another systematic review, Barrera et al. reviewed 65 observational studies. They concluded that, compared with previous reviews, the prevalence of diabetes and hypertension was lower in hospitalized patients with COVID-19, and there was no association between these conditions and this disease's severity and mortality (5). A French study of 2 796 patients also found that the use of anti-hypertension drugs in diabetic patients, particularly ACE inhibitors, did not increase mortality (17).
A limitation of this study was the sparsity of data on some variables. However, attempts were made to reduce the impact of this factor on the results as much as possible by using appropriate statistical methods. Another limitation was the relatively small size of our sample population. Therefore, larger, multi-center studies are required to confirm our findings, which would provide more robust evidence.
5.1. Conclusions
The COVID-19 pandemic has brought an unprecedented healthcare challenge. Several risk factors are associated with the progression of this disease. Recognition of such factors can help identify at-risk populations and establish preventive strategies. Age, chronic disease, respiratory disease, and cardiovascular disease have been studied extensively and found to be significantly associated with the severity of COVID-19.
The present study showed that the extent of respiratory distress and the length of hospital stay were lower in the control group than in the diabetes and hypertension groups. However, there was no significant association between these diseases and the risk of mortality and long hospital stays due to COVID-19 infection.