1. Background
The nursing practice implies working in a complex environment. Formally, nurses’ role and performance in the health system are crucial, even if they need to deal with multiple stressors over time that can lead to burnout (1). Burnout might be considered a set of reactions resulting from situations of chronic occupational stress in which the dimension of commitment is predominant (2). It might be considered characterized by three dimensions: (A) emotional exhaustion and the feeling of being emptied of one’s emotional resources, (B) depersonalization or cynicism, insensitivity to the surrounding world, dehumanization of the relationship to the other, and a negative vision of others and work, and (C) the feeling of personal non-fulfillment at work, a feeling of not being able to correctly meet the expectations of those around him/her, the depreciation of his/her results, and the feeling of waste (3).
Burnout might affect all occupations that require intense personal commitment (4). Nurses, as a professional group, are at higher risk of burnout (5). Several research studies have examined burnout among nurses worldwide (5). The findings in a meta-analysis report that burnout differs across nations due to distinct cultural and organizational frameworks (6), which included data from 49 countries and showed that the overall prevalence of burnout symptoms among nurses is 11.23%. In a regional hospital in Taiwan, nurses (66%) were the most affected by burnout (7). Around 44% of European nurses have indicated experiencing burnout (8). However, in Brazil, 35.7% of nurses were observed to be suffering from burnout (8). Emergency nurses might experience much higher levels of burnout than others due to their exposure to stress (9). In Ireland (10), 52% of nurses in an emergency department experienced high levels of burnout significantly related to the nature of their work environment. Other findings were found in intensive care settings (11). Younger age, single marital status, absence of religious affiliation, less work experience, and prior end-of-life care experience were all observed to have a significant association with a higher level of burnout (11).
Factors related to burnout might be classified into occupational, social organization, and personal traits (12). Notably, some associated factors have been largely recognized, such as gender, workload, and quality of working conditions (11). Other areas of burnout include nurses’ work environments, age, education, and length of work experience (3, 9), relationships between staff and members, the care of difficult patients (13), or decision-making to abandon sustainable treatments (11). Additionally, some personality traits, such as anxiety, irritability, depression, and narcissism, have been related to burnout (5, 14). These factors might explain the reason why, under the same workload, one nurse is exhausted while another reports no stress (12, 14).
Burnout has serious adverse consequences, affecting not only nurses but also patients, colleagues, and healthcare organizations. The burnout affects the quality of life and work efficiency of nurses over time (4). In addition, in a systematic review (3), the repercussions of burnout can directly impact the mental, physical, and behavioral well-being of nurses (15). This can lead to a significant decline in their overall quality of life and a reduction in the quality of care they provide to patients. Ultimately, this diminishes the safety and effectiveness of these healthcare professionals (15).
In addition, the adaptation theory emphasizes the active role of individuals in the interpretation and response to the main stressors of life. Similarly, behavior is better understood as a dynamic process of a transaction between the individual and life situations in a broader sociocultural context. In particular, religion does have a positive effect on adaptation strategies (16). However, spiritual and religious beliefs are important ways to handle challenges and are considered intrinsic to human nature and the deepest and most powerful healing resource available to the person (17). The importance of religious commitment would act as a resilient strategy for adaptation to illness and treatments (5). The spiritual/religious commitment of patients appears to be correlated with their psychological well-being (18). Therefore, spirituality has an impact on quality of life dimensions (19). Additionally, lower levels of burnout were associated with higher levels of spiritual well-being (11).
Furthermore, nurses utilize a variety of coping strategies to mitigate burnout (20). Among these strategies, spirituality, and religiosity hold significant sway in addressing the challenges and burnout arising from the demands of nursing care (5). Additionally, numerous studies in a systematic review consistently indicate that individuals with stronger spiritual and religious convictions tend to exhibit lower degrees of burnout, experiencing reduced levels of exhaustion and depersonalization across various contexts and environments (5). Another study discovered that elevated levels of spiritual well-being serve as a preventative measure in mitigating burnout (21).
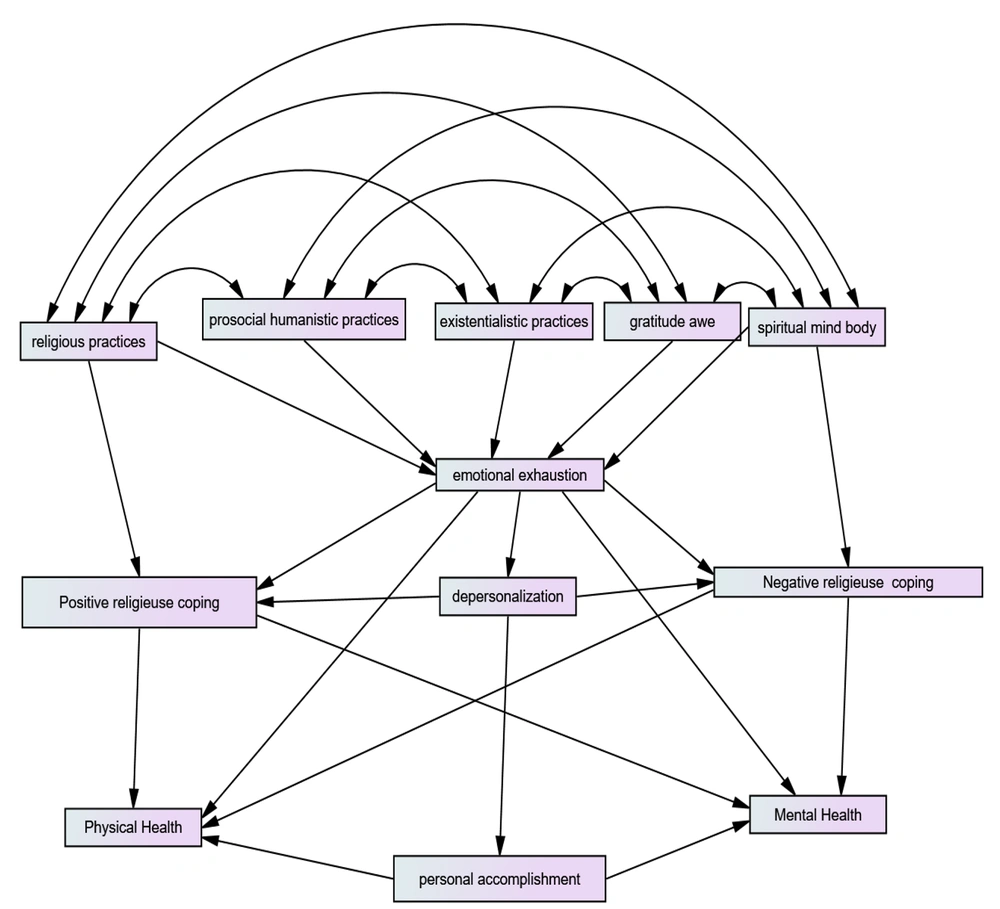
As argued in different studies, the spiritual commitment and religious adaptation among nursing staff are poor (22, 23). The present study was conducted as a multi-center cross-sectional survey at university and regional hospital centers, whose main objective was to assess the relationships between spiritual and religious commitment and adaptation strategies with burnout dimensions, in addition to the interrelation between burnout and quality of life among nurses in the emergency, intensive care, and psychiatry units and maternity departments of regional and university hospitals in Morocco. This study hypothesized that burnout dimensions might play as mediators and be negatively associated with mental and physical health, religious dimensions, and quality of life. Specifically, it was investigated whether spiritual commitment would have been associated with positive and negative religious adaptation and whether burnout dimensions would have been associated with quality of life. This hypothesis is modeled in Figure 1.
2. Methods
2.1. Participants
This multicenter quantitative cross-sectional survey was conducted among nurses working in the emergency departments, intensive care, resuscitation, psychiatry units, and midwifery departments in the maternity departments of regional and university hospitals in Morocco. No formula was used to determine the sample size for this study. A convenience sample of 575 (nursing personnel were advised, and participants voluntarily joined the survey) was selected. The sample included nurses from the emergency, intensive care and resuscitation, and psychiatry units and midwives from the maternity units in 12 regional and 4 university hospitals of Morocco. The survey was based on an anonymous questionnaire. The records of responses to the present study’s questionnaires did not contain any information useful to the identification of participants, and there was no collection of personal data. The distribution and collection of the questionnaire were realized in each hospital from March 2018 to February 2019.
Out of the 575 nurses who were contacted and invited to participate in the current survey, we successfully received responses from 535 participants, resulting in a high participation rate of 93.00%. The participants’ questionnaires were deemed acceptable if they were completed in their entirety, and the participants were able to successfully fill out the measurement scales with no instances of missing data. However, the present study excluded 40 participants from the present analysis due to a significant amount of missing data, and the participants were unable to complete two measurement scales that were not included. The questionnaire was administered exclusively to nurses who were physically present at their workplace during the distribution. The initial two authors (IA and GK) were responsible for data collection from all nurses in a face-to-face format. This approach was chosen to ensure participants’ confidence and enhance their engagement with the study.
2.2. Data Collection
This study employed a cross-sectional design using a questionnaire that included a set of instruments previously used and validated in previous studies (2, 24-26). The distribution of the questionnaire occurred between March 2018 and February 2019.
2.3. Measures
The sociodemographic characteristics, including gender (male and female), age (year), level of education (without a bachelor’s degree, bachelor’s degree, and a master’s degree), and marital status, were collected. Professional characteristics recorded were specialty (nurse, anesthetist nurse, psychiatric nurse, and midwife), the workplace (regional hospital center and university hospital center), and departments (emergencies, resuscitation, maternity, and psychiatry).
2.4. Instruments
The Maslach Burnout Inventory (MBI) (2): The Maslach Burnout Inventory (MBI) is a valid, easy-to-use instrument whose psychometric qualities have been enormously studied and translated into several languages. The main psychometric properties of reliability and validity of the Arabic version of the Maslach Burnout Inventory-Human Services Survey (MBI-HSS) appear to be satisfactory. The result of the reliability test with Cronbach’s alpha was 0.845 (emotional exhaustion [EE]), 0.732 (depersonalization [DP]), and 0.858 (personal accomplishment [PA]); these results are in line with the psychometric properties of the original MBI (27). It is considered the most used instrument to measure the symptoms of exhaustion. The tool is subdivided into three parts: (A) Emotional exhaustion (EE) (9 items), (B) depersonalization (DP) (5 items), and (C) personal accomplishment (PA) (8 items). For each element, participants might indicate their feelings on a Likert scale (0 = never to 6 = every day). The total items for each subscale were then ranked for interpretation (low, moderate, and high) as EE (≤ 16, 17 - 26, and ≥ 27), DP (≤ 6, 7 - 12, and ≥ 13), and PA (≥ 37, 31 - 36, and ≤ 30). A high score on EE and DP and a low score on the sense of lack of PA subscale define burnout.
Spiritual and Religions Attitudes Questionnaire (28): The spiritual and religious attitudes questionnaire in the shortened version SpREUK-P (29) is composed of 17 items exploring each person’s spiritual and religious attitude. The Arabic version SpREUK A2.b is a valid questionnaire, with Cronbach’s alpha 0.958 (30). The elements of the SpREUK-P are marked on a 4-point scale (0-never, 1-rarely, 2-often, and 3-regularly). The scores can be referenced to a level of 100%, reflecting the degree of commitment to distinct forms of spiritual/religious practice (engagement scores). Scores > 50% indicate a higher commitment; nevertheless, scores < 50% indicate a rare commitment. The SpREUK-P SF17, shortened to 17 elements, differentiates the same 5 factors, namely Religious, Humanistic, Existential, Gratitude/Reverence, and Spiritual (body of the spirit).
Religious Adaptation (RCOPE) (25): The Religious Coping Questionnaire (RCOPE) consists of 14 elements comprising two subscales that measure two models of religious adaptation methods, positive and negative attacks. Individuals indicate how often they engage in each form of religious adaptation on a 4-point scale from 0 (not at all) to 3 (a lot). Negative adaptation is seen as a spiritual struggle: “efforts to conserve or transform a spirituality that has been threatened or hurt”. The religious struggle was measured by the negative religious adaptation subscale, which consists of 7 elements that evaluate God’s punitive assessments, interpersonal religious discontent, demonic evaluations, spiritual discontent, and questioning of God’s powers. This evaluation gives only negative results (elements 8 - 14). Positive religious adaptation consists of 7 elements that measure the search for spiritual support, the search for a spiritual connection, collaboration with God in problem-solving, religious forgiveness, and benevolent religious assessments of illness. This instrument has demonstrated good construction validity and internal consistency in medical samples and in individuals facing major life stress. The Arabic Religious Adaptation Scale had acceptable reliability; Cronbach’s alphas ranged from 0.82 to 0.86 for the positive subscale and the negative subscale (31).
The Moroccan Arabic SF-12 Health Survey (SF: Short form) (26): The SF-12 is a measure developed to provide a shorter, more specific, valid alternative to the SF-36. The SF-12 is weighted and summed to provide easily interpretable scales for physical and mental health. Composite scores for physical and mental health (Physical Composite Scale [PCS] and Mental Composite Scale [MCS]) are calculated using scores of 12 questions and ranged from 0 to 100, where a score of 0 indicates the lowest level of health measured by the scales and 100 indicates the highest level of health. The psychometric properties of the Moroccan Arabic SF-12 Health Survey appear to be valid in measuring health status in large-scale samples of the Moroccan population. Cronbach’s alpha was 0.80 for the SF-12 PCS and 0.79 for the SF-12 MCS (26). The SF-12 includes 12 items from the SF-36 Health Survey (version 1). These items include 2 questions regarding physical functioning, 2 questions about role limits due to physical health issues, 1 question about body pain, 1 question on general perceptions of health, 1 question about vitality (energy/fatigue), 1 question about social functioning, 2 questions about role limits due to emotional issues, and 2 questions on general mental health (psychological distress and psychological well-being). It can be administered to any patient or general population.
2.5. Data Analysis
The collected data were analyzed descriptively, and correlations were computed. The Statistical Package for the Social Science (SPSS) software (version 23; IBM CORP, Armork, USA) and AMOS software (version 23.0) were used for data analyses. The characteristics of the sample were analyzed descriptively; therefore, in the absence of normality of the sample data, the maximum likelihood estimation method with Bootstrap was used. The structural equation model (SEM) (32) for the path analysis was constructed to analyze the direct and indirect effects of health subscale burnout on mental and physical health. A model was established using adaptation and religious/spiritual engagement as the independent variables, physical and psychological health as the dependent variables, and EE, DP, and PA (burnout) as the mediators. The fitness of the overall measurement model was assessed using various goodness and badness indices, including chi-square χ2, comparative fit index (CFI), Tucker-Lewis index (TLI), and the root mean square error of approximation (RMSEA); the CFI and TLI ≥0.90 indicated acceptable fit, and RMSEA values of less than 0.06 were considered excellent (≤0.08 for adequate fit and ≤0.10 for acceptable fit) (33). To determine the model’s adequacy, this study followed established guidelines. Goodness indices should exceed 0.9, badness indices should remain below 0.10, and the χ2/df value should be less than 5 (34).
2.6. Ethical Approval
The study was approved by the Appropriate Ethics Committee of Biomedical Research of the Faculty of Medicine and Pharmacy, Mohamed V University in Rabat, Morocco, under file number 125/2018. All the participants gave their written informed consent in order to join the survey. The data were anonymous and treated with confidentiality, equality, and justice, respecting the Helsinki principles.
3. Results
A total of 535 participants from 16 hospitals located across the country (mainly emergency departments, maternity, intensive care, resuscitation units, and psychiatric departments) responded positively to completing the questionnaire. The sample included general nurses (36%), midwives (28%), psychiatric nurses (20.6%), and emergency and intensive care nurses (15.4%). The majority of the sample was represented by the female gender (74%) and a mean age of 34.1 ± 10.5 years. More than 57.2% of the participants were married. Almost 97% of the participants reported having a degree in nursing, and 58.3% were in regional hospitals; nevertheless, 42.7% of the participants were in university hospitals. More descriptive findings for the questionnaires are shown in Table 1.
| Mean ± SD | Religious Practices | Prosocial Humanistic Practices | Existentialistic Practices | Gratitude Awe | Spiritual Mind-Body Practices | Emotional Exhaustion | Depersonalization | Personal Accomplishment | Positive Religious Adaptation RCOPE | Negative Religious Adaptation RCOPE | Physical Health | Mental Health | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Religious practices | 54.15 ± 21.72 | 1 | 0.25** (0.000) | 0.29** (0.000) | 0.22** (0.000) | 0.51** (0.000) | -0.03 (0.420) | 0.034 (0.426) | 0.15** (0.000) | 0.41** (0.000) | -0.008 (0.85) | -0.02 (0.57) | 0.06 (0.15) |
| Prosocial humanistic practices | 78.83 ± 17.44 | 1 | 0.32** (0.000) | 0.52** (0.000) | 0.18** (0.000) | 0.09* (0.028) | 0.025 (0.559) | 0.27** (0.000) | 0.25** (0.000) | -0.07 (0.13) | -0.020 (0.64) | 0.01 (0.71) | |
| Existentialistic practices | 65.99 ± 23.79 | 1 | 0.32** (0.000) | 0.35** (0.000) | 0.17** (0.000) | 0.111* (0.010) | 0.191** (0.000) | 0.21** (0.000) | 0.05 (0.21) | -0.017 (0.69) | -0.01 (0.74) | ||
| Gratitude awe | 66.95 ± 20.08 | 1 | 0.24** (0.000) | 0.21** (0.000) | 0.1* (0.025) | 0.175** (0.000) | 0.19** (0.000) | -0.01 (0.73) | -0.03 (0.40) | 0.02 (0.7) | |||
| Spiritual mind-body practices | 37.65 ± 25.66 | 1 | 0.03 (0.539) | 0.14** (0.001) | 0.11** (0.008) | 0.23** (0.000) | 0.158** (0.000) | -0.06 (0.14) | 0.10* (0.02) | ||||
| Emotional exhaustion | 30.56 ± 11.18 | 1 | 0.44** (0.000) | 0.171** (0.000) | 0.09* (0.026) | 0.05 (0.26) | -0.15** (0.001) | -0.29** (0.000) | |||||
| Depersonalization | 11.12 ± 6.11 | 1 | -0.079 (0.069) | 0.03 (0.545) | 0.171** (0.000) | -0.07 (0.08) | -0.18** (0.000) | ||||||
| Personal accomplishment | 31.22 ± 8.41 | 1 | 0.174** (0.000) | -0.03 (0.42) | -0.08 (0.07) | -0.010 (0.82) | |||||||
| Positive religious adaptation RCOPE | 17.03 ± 4.53 | 1 | -0.14** (0.001) | -0.08 (0.06) | 0.01 (0.7) | ||||||||
| Negative religious adaptation RCOPE | 4.36 ± 4.74 | 1 | -0.010 (0.81) | -0.15** (0.001) | |||||||||
| Physical health | 42.08 ± 8.01 | 1 | -0.06 (0.17) | ||||||||||
| Mental health | 40.06 ± 8.35 | 1 |
Descriptive Statistics and Pearson’s Correlation Coefficients of Variables a
Cronbach’s alpha coefficients were computed for each subscale of the scales under investigation. Specifically, the reliability for positive and negative religious adaptation subscales was 0.9 and 0.84, respectively. The religious commitment subscale demonstrated a reliability of 0.8. The overall reliability was generally high, indicating good internal consistency, surpassing the threshold of 0.7, with the exception of DP, which achieved a score of 0.65.
Almost 63.6% and 41.3% of the participants reported a high score for the EE and DP dimensions, respectively, and 29.2% of the respondents reported a low score on the PA dimension. The majority of the respondents reported a high engagement of religiousness. Moreover, 52.1% of the participants scored high in religious practice, 93.1% higher in prosocial humanistic, and 77.4% higher in existentialistic practices. In this study, 81.5% of the respondents were highly engaged in gratitude awe; nevertheless, 72.1% of the participants reported a rare engagement in spiritual mind-body practices.
The participants showed mean physical health and mental health scores of 42.0 ± 8.01 and 40.0 ± 8.35, respectively. The lower level of physical health was associated with higher levels of EE (53.27% of participants); however, the lower level of mental health was associated with higher levels of EE (57.75% of participants) and DP (37% of participants).
According to the hypothesized model, a correlation matrix was shown, using Pearson’s correlation, in order to explore the relationships between the variables in the path model, which is shown in Table 1. The findings of this correlation matrix propose several significant relationships that were predicted, including the relationships between dimensions of religious engagement and all other variables in the model, the relationship between religious adaptation and quality of life, and the relationship between burnout dimensions and negative and positive adaptation. Some other relationships were not significant, including those between PA and mental and physical health in the model. Furthermore, physical health was not significantly linked to positive and negative adaptation.
The initial model (Figure 1) was developed and tested with the dimensions of religious, humanistic, and existential practices, gratitude, spiritual mind-body practices, burnout, and quality of life as latent variables. The model was based on a theoretical and empirical approach. All hypothesized pathways were not significant, and certain model dimensions were significantly correlated. The testing of the initial SEM revealed a poor fit to the data (df = 35, χ2 = 148.56, χ2/df = 4.24, P < 0.0001, CFI = 0.88, TLI = 0.778, and RMSEA = 0.08).
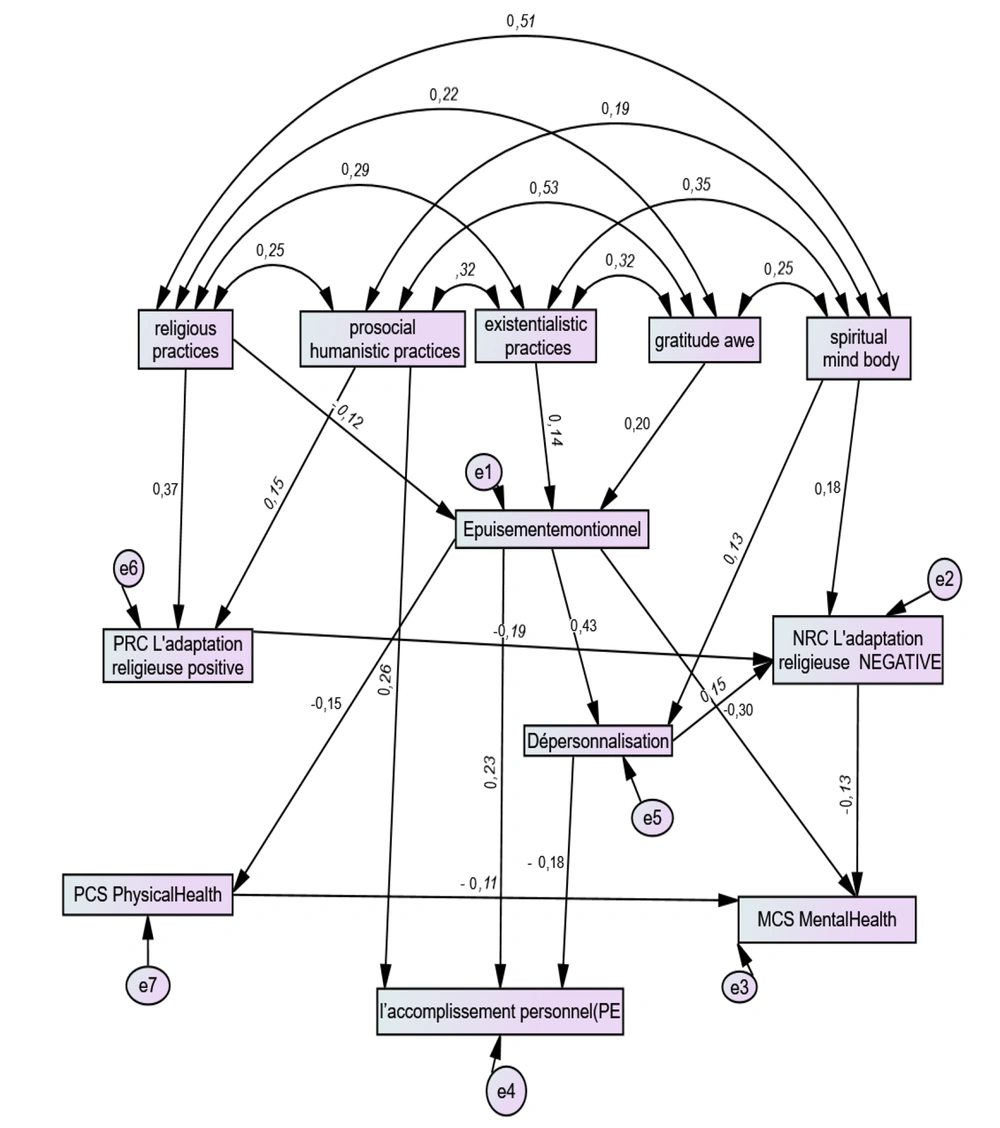
Then, various adjustments and improvements, reformulating the model, were accepted, especially the removal and addition of certain pathways between dimensions guided by modification indices (MI), as shown in Table 2 and on empirical and theoretical grounds. Additional direct paths were accepted between EE and PA (MI = 22.73), as suggested by Pehlivanoğlu and Civelek (35), between negative and positive religious adaptation (MI = 16.829) as reported in empirical studies (25, 36), between prosocial humanistic practices and PA (MI = 40.32), and later with positive religious adaptation (MI = 16.70) and physical and mental health (MI = 5.95) as the findings of Ohrnberger et al.’s study (37). At last, the link between spiritual mind-body and DP emerged as given by MI. According to the aforementioned evidence, some not statistically significant pathways were deleted from the model.
| Variables | MI | Expected Parameter Change |
|---|---|---|
| Depersonalization←Spiritual mind-body practices | 10.626 | 0.030 |
| Negative religious adaptation←Positive religious adaptation | 16.829 | -0.181 |
| Positive religious adaptation←Prosocial humanistic practices | 11.115 | 0.034 |
| Personal accomplishment←Prosocial humanistic practices | 40.316 | 0.132 |
| Personal accomplishment←Positive religious adaptation | 16.701 | 0.327 |
| Personal accomplishment←Exhaustion emotional | 22.737 | 0.155 |
| Mental health←Physical health | 5.957 | -0.104 |
Modified Indices of the Model
The quality of fit of the improved model is shown in Figure 2. The absolute fit measure showed and confirmed an adequate and satisfactory fit of the improved model (df = 39, χ2 = 46.29, χ2/df = 1.19 ≤ 2, CFI = 0.99, TLI = 0.98 > 0.90, and RMSEA = 0.019).
In brief, the model is illustrated in Figure 2. The SEM for the path analysis was constructed to analyze the direct and indirect effects of spiritual/religious commitment and burnout on mental and physical health. Table 3 shows the direct effects, indirect effects, and total effects among all the constructs.
| Variebles | Effects | Direct | Indirect | Total |
|---|---|---|---|---|
| Emotional exhaustion | Religious | -0.06 a | - | -0.06 a |
| Existantialistic | 0.07 a | - | 0.07 a | |
| Gratitude | 0.11 a | - | 0.11 a | |
| Positive religious adaptation | Emotional exhaustion | 0.04 b | - | 0.04 b |
| Religious | 0.079 a | -0.002 | 0.077 a | |
| Prosocial humanistic | 0.04 a | - | 0.04 a | |
| Existentialistic | - | 0.003 | 0.003 | |
| Gratitude | - | 0.004 b | 0.004 b | |
| Personal accomplishment | Emotional exhaustion | 0.165 | -0.052 a | 0.113 a |
| Depersonalization | -0.252 a | - | -0.252 a | |
| Positive religious adaptation | 0.19 b | - | 0.19 b | |
| Religious | 0.008 | 0.008 | ||
| Prosocial humanistic | 0.11 a | 0.01 | 0.12 a | |
| Existantialistic | - | 0.007 b | 0.007 b | |
| Spiritual mind-body practices | - | -0.008 b | -0.008 b | |
| Gratitude | - | 0.012 b | 0.012 b | |
| Mental health MCS | Emotional exhaustion | -0.23 a | -0.01 | -0.22 a |
| Positive religious adaptation | - | 0.05 | 0.05 | |
| Depersonalization | -0.03 | -0.03 | ||
| Negative religious adaptation | -0.23 b | - | -0.23 b | |
| Religious | - | 0.02 | 0.02 | |
| Prosocial humanistic | - | 0.002 | 0.002 | |
| Existantialistic | - | -0.014 b | -0.014 b | |
| Spiritual mind-body practices | - | -0.009 | -0.009 | |
| Gratitude | - | -0.024 a | -0.024 a | |
| Physical health PCS | -0.11 b | - | -0.11 b | |
| Depersonalization | Emotional exhaustion | 0.24 a | - | 0.24 a |
| Religious | - | -0.015 b | -0.015 b | |
| Prosocial humanistic | - | |||
| Existantialistic | - | 0.016 b | 0.016 b | |
| Gratitude | - | 0.03 a | 0.03 a | |
| Negative religious adaptation | Emotional exhaustion | 0.02 a | 0.02 | |
| Depersonalization | 0.12 a | - | 0.122 a | |
| Religious | -0.017 | -0.017 | ||
| Prosocial humanistic | -0.007 | -0.007 | ||
| Existantialistic | 0.001 | 0.001 | ||
| Spiritual mind-body practices | 0.033 a | 0.004 b | 0.037 a | |
| Gratitude | - | 0.002 | 0.002 | |
| Positive religious adaptation | -0.194 a | -0.194 a | ||
| Physical health PCS | Emotional exhaustion | -0.11 a | -- | -0.11 a |
| Religious | - | 0.006 | 0.006 | |
| Existantialistic | - | -0.007 b | -0.007 b | |
| Gratitude | - | -0.012 b | -0.012 b |
Direct and Indirect Effects of Variables in the Final Model
A model was established using religious adaptation and spiritual commitment as independent variables, physical and mental health as dependent variables, and EE, DP, and PA (burnout) as mediators in this relationship. In addition, the model enunciates that some factors, namely dimensions of religious practice, existentialistic, and gratitude awe, had an impact on EE. Prosocial humanistic practice had a significant direct impact on PA and positive religious adaptation. In addition, EE had a direct effect on DP and PA and an inverse effect on negative religious adaptation and mental and physical health dimensions. Finally, the final model showed the direct effect of positive religious adaptation on PA. Physical health had a direct effect on mental health, as expected. Positive religious adaptation had an indirect impact on mental health variables through negative religious adaptation. Mind-body spiritual practices had a direct impact on DP and on negative religious adaptation. The variances in mental and physical health explained by this model were 10.4% and 3.3%, respectively.
4. Discussion
One of the main aims of this study was to investigate the relationships between burnout dimensions, religious adaptation and spiritual commitment, and quality of life using mental and physical health scores. The obtained results confirm previous evidence regarding the effects of spiritual commitment and religious adaptation on quality of life across burnout dimensions.
The dimensions of religion are highly complex, and further studies explaining the causal relationship between variables will be needed. Overall, the results supported the hypothesized path model, proposing that the religious practice dimension has a significant relationship with positive religious adaptation and EE and has an indirect impact on mental health through negative religious adaptation. These findings are consistent with the documented importance of religious and spiritual strategies used by professionals to cope with burnout and improve their mental health (5). The current study’s results also showed a relationship between negative and positive religious adaptation; these two dimensions are not opposite (36). In addition, spirituality and religiousness are different constructs but significantly correlated (38). In addition, some review studies have shown an inverse relationship between spiritual/religious commitment and burnout in nurses (3).
Some studies (39, 40) have pointed out that dimensions of burnout (EE, DP, and PA) show a mediating role between religious commitment and religious adaptation and between mental and physical health. The variables of religious/spiritual commitment and religious adaptation showed indirect impacts on mental and physical health (39, 40). Koenig noted that the connections between religious/spiritual factors and mental health are more robust than those with physical health (41).
Negative and positive religious adaptation held a mediating position. These results are consistent with a study’s findings (42), which indicated that negative religious adaptation impacts mental health. Additionally, in line with other pieces of evidence (43, 44), religious adaptation significantly correlates with both depressive and anxiety symptoms: the more negative religious adaptation, the greater anxiety and depressive symptoms. There was no significant statistical correlation between positive religious adaptation and physical health (45), probably influenced by a range of dysfunctional religious adjustments. A significant relationship between positive health outcomes and positive religious adaptation is associated with some adaptive abilities in a range of situations (46). Spirituality is crucial in the health setting as a source of healing (47). Therefore, religion positively impacts health through a social mediation of health values (48).
In addition, burnout and depression are “distinct”, and their relationship might be misleading (49). The articles included in an adaptation review (5) show that the consequences of burnout might directly influence the mental, physical, and behavioral health of nurses (5). The findings confirmed the hypothesis in the improved model, whereby EE is a mediator of the impact of religious commitment on DP, and DP mediates the relationship between EE and PA (5). Consistent with other pieces of evidence (50, 51), the present study showed a direct impact of EE on DP and an indirect impact of EE on PA. There was no association between PA and mental and physical health in the current study; in contrast, quality of life improves the factors associated with the model of burnout dimensions, notably EE and PA (52).
This study aimed to potentially provide a solution to the routine burnout faced by nurses and healthcare professionals. However, more aspects need to be explored, including how the nurses use spirituality and religion as adaptation strategies. These findings might show significant implications for nurse training and education in healthcare. The positive correlation between spiritual and religious beliefs and lower levels of burnout suggests implementing targeted strategies in order to mitigate burnout and enhance the well-being of nurses, including spiritual and religious support mechanisms in the workplace environment, creating a culture of inclusivity respecting diverse spiritual and religious beliefs with a more supportive and nurturing work environment. Furthermore, educational programs for nurses should include modules on self-care and stress management and the importance of spiritual well-being. These strategies might reduce burnout rates among nurses and enhance the overall quality of healthcare delivery. Additionally, this study’s findings help describe different levels of adaptation among nursing members and leaders.
Priorities include establishing a comprehensive strategy for enhancing the working environment and conditions of professionals. This multifaceted approach aims to promote physical well-being and mental health support, foster leadership development, recognize employee contributions, and ensure a healthy work-life balance.
The current study might have some limitations, including (1) the cross-sectional design of the study, which did not allow for the establishment of a causal relationship between variables, (2) the convenience sampling, and (3) the participants who were only from large hospitals, whereas nurses and midwives working in rural health centers have been not recruited in this study. Future longitudinal studies should include nurses from different settings. Finally, the present study’s results should not be generalized to all Moroccan nurses since the survey covered four major health departments but did not include all national departments. The study strengths might be (1) the use of validated tools, (2) the innovation of this study, and (3) the number of participants. Finally, the data were collected from 12 regions.
4.1. Conclusions
Nursing is considered a significantly stressful profession. The model has been proposed on theoretical assumptions and previous study findings on adaptation strategies leading to better physical health and mental health. A lower level of EE will lead to higher perceived physical and mental health among nurses. In particular, the results suggested a significant relationship between religious/spiritual commitment and religious adaptation dimensions with physical and mental health mediated by burnout dimensions in this group of healthcare professionals. It is suggested that nurses might approach religious and spiritual practices in order to reduce burnout and improve their physical and mental health.