1. Background
The coronavirus disease 2019 (COVID‐19) ravaged the world, leading to a global pandemic. The disease with persistent, long-lasting symptoms, termed long COVID, has been considered a significant public health concern. Long COVID generally afflicts severely ill patients or those with comorbidities (1). Any symptom that remains beyond 12 weeks after the onset of the initial presentation that cannot be explained by alternative diagnoses is defined as long COVID (1)
Common physical symptoms reported post-COVID-19 are fatigue, breathlessness, joint pain, muscle aches, and reduced physical capacity, which can be experienced more than 6 months post-infection (2-4). These ongoing symptoms interfere with normal functioning and negatively affect the health-related quality of life (HRQoL) of patients (5). In addition, individuals experiencing prolonged post-COVID-19 symptoms face difficulties resuming or maintaining their physical activity (6). Physical activity is an essential component for successful long-term recovery from any illness, which has profound mental and physical health benefits (7). Although rehabilitation interventions seem to be potentially beneficial to patients, there is a need to expand our understanding of the long-lasting symptoms of COVID and their impact on HRQoL.
2. Objectives
We aimed to assess the association of breathlessness, fatigue, pain, and the level of physical activity with the physical and mental health of hospitalized and non-hospitalized COVID survivors in the post-infection period up to six months.
3. Methods
The data of 315 patients with documented SARS-CoV-2 infection identified between 15 August 2020 and 30 December 2020 were retrieved from the medical records of two hospitals, Imam Hussein and Labbafinezhad. In order to minimize face-to-face contact, an electronic link was sent to COVID-19 survivors from 1 January 2021 to 30 August 2021, enclosing an online questionnaire survey via an Iranian platform (Porsline; https://survey.porsline.ir). The responses to the questionnaires were automatically stored on the platform. In order to accurately complete the questionnaires, a trained interviewer contacted all eligible patients by phone and assisted them in completing the survey. Verbal informed consent was obtained from all participants. The institutional review board approved the study’s procedures, and ethical approval was obtained from the institutional ethics committee of the Institutional Review Board of Shahid Beheshti University of Medical Sciences, Tehran, with the approval code of IR.SBMU.RETECH.REC.1399.398, approving the adequacy of obtaining verbal consent by telephone due to the restrictions caused by the COVID-19 pandemic. This study conforms to the STROBE guideline and reports the required information accordingly (Appendix 1 in the Supplementary File).
A COVID-19 rehabilitation screening tool was developed using a series of standardized, validated questionnaires, including (I) a sociodemographic data questionnaire for recording gender, age, and education, (II) Disease severity, (III) Multi Fatigue Inventory (MFI), (IV) Short-Form Health Survey (SF12) for measuring quality of life, (VI) International Physical Activity Questionnaire (short form) (IPAQ), and (VII) COVID-19 Yorkshire Rehabilitation Scale (C19-YRS), a Post-COVID-19 functional disability and symptom severity screening tool (8).
The C19-YRS seeks new or worsening symptoms and functioning compared with the pre‐COVID‐19 condition. Using a VAS Likert scale, participants were asked to rate their pre- and post-COVID-19 capability of walking/mobility and performing activities of daily living, as well as the severity of symptoms (pain, breathlessness, and fatigue). In order to discover changes in symptoms and functioning, post-COVID-19 VAS scores were subtracted from pre-COVID-19 VAS scores. In order to define COVID-19 disease severity at the acute phase, the following items were considered: hospital admission or oxygen therapy/critical care requirement. Individuals treated in an outpatient clinic were categorized under low severity (S1); hospitalized patients were regarded to have moderate severity (S2), and those admitted to the intensive care unit were considered severely ill (S3).
3.1. HRQoL (SF-12)
The SF-12 was used to measure patients’ physical and mental health. This tool contains 12 items and eight dimensions: sexual performance, physical role, physical pain, general health, energy and vitality, social performance, emotional role, and mental health. The eight dimensions form two subscales of the Physical Component Scale (PCS) and Mental Component Scale (MCS). Scores are calculated according to the SF-12 scoring algorithm proposed by John E. Ware in 1995. All summary scores range from 0 to 100, allowing them to be comparable with SF-36 scores, where higher scores indicate better HRQoL (9). The Iranian version of the tool used in this study has been reported to have acceptable psychometric properties (10)
3.2. Fatigue (MFI-20)
The MFI-20 covers five fatigue-related dimensions: general fatigue, physical fatigue, reduced activity, mental fatigue, and reduced motivation. The scores of the five dimensions range from 4 to 20, with higher scores indicating higher fatigue levels. The psychometric properties of the MFI-20 have been tested in Iranian populations, supporting its validity (11).
3.3. Level of Physical Activity (Short-form IPAQ)
The short version of IPAQ was used to measure physical activity. The tool includes seven items that evaluate the activities performed in the previous week (walking, moderate- and vigorous-intensity physical activities, and sitting) based on the time spent on each activity. The scoring was according to the amount of energy expenditure estimated as metabolic equivalent (light activity = 3.3, moderate activity = 4, vigorous activity = 8) minutes per week (MET-min/week). The level of physical activity was categorized into three groups as follows: low physical activity (< 600 METs/week), moderate (METs/week between 600 and 3000), and vigorous (>3000 METs/week). The Iranian version of IPAQ has shown acceptable reliability and validity for assessing the level of physical activity (12). The questionnaire’s link was sent online through https://survey.porsline.ir/s/kjLDY9W to collect information.
3.4. Data Analysis
We used descriptive and inferential statistics in parallel with the aims of the study. Descriptive statistics, including frequency, percentage, and mean, were conducted to illustrate the characteristics of the participants and the mean scores of the variables. Bivariate analysis was conducted to investigate the association of demographic data, IPAQ, MFI-20, and VAS scores post-COVID-19 with the PCS and MCS scores. Pearson’s correlation was performed for continuous and categorical variables, and the independent samples t-test and analysis of variance (ANOVA) were used to test between-group differences in terms of the means of PCS and MCS scores. Also, we used Spearman and Pearson correlation to find if there was a correlation between the study variables. Prior to linear regression analyses, normality was assessed for independent variables, and collinearity diagnostics were assessed to confirm the lack of multi-collinearity. In the regression analysis, the correlation between all independent variables was obtained as < 0.80. All variables with significant correlations with the PCS and MCS scores were included in multiple linear regression analysis. Standardized beta values (β values) were presented to reflect the direction and strength of the association between each independent variable and PCS and MCS. According to regression analysis, the changes observed in pre- and post-COVID-19 ratings on VAS were categorized as none, mild (1‐3), moderate (4‐6), and severe (7‐10). A statistical significance level of P≤0.05 was considered in all tests. Analyses were conducted using IBM SPSS 22. There was no missing data since progress to the next questions on the online survey was dependent on completing previous items.
The sample size was calculated using G*Power version 3.1.9.2 for a linear multiple regression model regarding an effect size (f2) of 0.1, the number of tested predictors of 2, the total number of predictors as 9, alpha = 0.05, and study power of 90%. The required sample size was calculated to be n = 130 (13).
4. Results
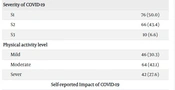
A total of 315 patients with the diagnosis of COVID-19 aged < 65 years were identified. Seventy of these patients were unreachable, and 245 individuals answered their phones. Ten subjects had died within the follow-up time, and 83 declined to participate. Finally, 152 agreed to participate in the study, approximately 50% of whom were treated in the outpatient clinic, and 6.6% were admitted to the ICU. Table 1 shows the demographic characteristics, IPAQ, MFI-20 (total score and scores of its subscales), changes in VAS scores of symptoms (pain, breathlessness, and fatigue), and the mean scores of PCS and MCS subscales. The mean age of the COVID-19 survivors was 40.07 (11.23) years, and 50.7% of the respondents were men. The mean length of hospitalization for hospitalized patients was 5.41 (9.83) days, with a mean duration of 217.80 (62.74) days from the time of positive test by PCR. Also, 80% of the survivors were evaluated at greater than 60 months post symptom onset. Regarding the patients’ medical records at the hospital, 36.2% of them had at least one chronic disease (9% hypertension, 9% diabetes, and 7.4% heart disease).
| Characteristics | No. (%) |
|---|---|
| Demographic/Individual Characteristic | |
| Gender | |
| Male | 77 (50.7) |
| Female | 75 (49.3) |
| Age categories | |
| Young (18 - 35) | 61 (40.1) |
| Middle age (36 - 65) | 91 (59.9) |
| Age | 40.07 (11.23) |
| Clinical Characteristics (Inpatients) | |
| Length of stay in hospital Mean (SD) | 5.41 (9.83) |
| Day since symptom onset Mean (SD) | 217.80 (62.33) |
| Severity of COVID-19 | |
| S1 | 76 (50.0) |
| S2 | 66 (43.4) |
| S3 | 10 (6.6) |
| Physical activity level | |
| Mild | 46 (30.3) |
| Moderate | 64 (42.1) |
| Sever | 42 (27.6) |
| Self-reported Impact of COVID-19 | |
| Reported post-discharge problems | 70 (46.1) |
| Changes in breathlessness during daily activities | 47 (30.9) |
| Changes in feeling of pain | 72 (47.4) |
| Changes in feeling fatigue | 61 (40.1) |
| Quality of Life and Fatigue | |
| PCS | 41.79 (7.34) |
| MCS | 44.09 (8.50) |
| Fatigue (total) | 53.23 (16.65) |
| General fatigue | 11.89 (4.30) |
| Physical fatigue | 11.24 (4.46) |
| Reduced activity | 10.18 (3.94) |
| Reduced motivation | 10.80 (3.63) |
| Mental fatigue | 9.12 (3.33) |
a Values are presented as mean ± SD.
The results of the C19-YRS scale showed that around 46.1% of the survivors reported persistent post-COVID-19 symptoms. In this regard, comparing VAS changes pre- and post-COVID-19 showed that 47.4 % of survivors had greater perceived pain, 30% perceived greater breathlessness post-COVID-19, and 40.1% reported becoming fatigued sooner compared to the pre-COVID-19 period. Furthermore, 38.8% and 44.1% of the COVID-19 survivors perceived more problems in accomplishing their daily living activities and difficulties in mobility/walking compared to the pre-infection time, respectively. Almost 70.4% of the survivors reported a low to moderate level of physical activity, measured by IPAQ, during the post-COVID-19 period. The mean MCS score (44.09 ± 8.50) was higher than the PCS score (41.79 ± 7.34), measured by the SF-12. The total mean fatigue score, measured by MFI-20, was equal to 53.23 ±16.65.
Bivariate analysis showed that demographics and COVID-19 physical symptoms were associated with the PCS and MCS scores of HRQoL. Individuals admitted to the ICU showed lower PCS scores compared to non-hospitalized patients. Also, individuals perceiving greater changes in pain and breathlessness in the post-COVID-19 time obtained lower PCS scores. The PCS and MCS scores were negatively associated with the score obtained from MFI-20 (Table 2).
| Characteristics | MSC | Statistics | PSC | Statistics |
|---|---|---|---|---|
| Gender | ||||
| Male | 43.21 | t = - 1.195 | 42.8540.70 | t = 1.817 |
| Female | 44.85 | |||
| Age | r = 0.093 | r = - 194* | ||
| Physical activity level | ||||
| Mild | 42.98 | 41.47 | ||
| Moderate | 44.28 | F = 0.521 | 43.15 | F = 2.349 |
| Sever | 44.76 | 40.06 | ||
| Length of hospitalization | r = - 0.060 | r = - 0.199* | ||
| Days since symptom onset | r = 0.097 | r = - 0.142 | ||
| COVID-19 severity | ||||
| S1 | 43.79 | F = 0.215 | 43.36 c | F = 5.849** |
| S2 | 44.46 | 40.87 | ||
| S3 | 42.22 | 35.88 c | ||
| Changes in breathlessness during daily activities | ||||
| No change | 43.98 | F = 0.712 | 42.54 d | F = 2.564* |
| Mild | 45.18 | 41.08 | ||
| Moderate | 40.53 | 39.87 | ||
| Sever | 43.48 | 34.15 d | ||
| Changes in pain | F = 3.275* | |||
| No change | 44.93 | 43.25 e | ||
| Mild | 42.09 | 41.06 | ||
| Moderate | 44.18 | 37.70 e | ||
| Sever | 47.63 | 40.37 | ||
| Fatigue total | r = - 0.287*** | r = - 0.224** | ||
| General fatigue | r = - 0.260** | r = - 0.190* | ||
| Physical fatigue | r = - 0.172* | r = - 0.234** | ||
| Reduced activity | r = - 0.250** | r = - 0.171* | ||
| Reduced motivation | r = - 0.228** | r = - 0.229** | ||
| Mental fatigue | r = - 0.324*** | r = - 0.107 |
a * P≤0.05, ** P < 0.01, ***P < 0.001
b Values are presented as mean ± SD.
c COVID-19 severity: A significant difference between non-hospitalized and ICU-admitted patients.
d Changes in breathlessness: Significant difference between the categories of no change and great changes (7-10).
e Changes in pain: Significant difference between the categories of no change and moderate changes (4-6).
Table 3 demonstrates the results of linear multiple regression analysis to estimate the effects of predictors on the PCS and MCS scores of SF-12. The results of multiple linear regression analysis indicated that only fatigue (measured by MFI-20) was negatively associated with PCS and MCS scores, with a low strength coefficient value of β = - 0.218 for PCS and a moderate strength coefficient value of β = - 0.305 for MCS. The model explained 15.3% and 10.6% of the variance observed in PCS (F = 2.84) and MCS (F = 1.88), respectively.
| Variables | MCS | PCS |
|---|---|---|
| Age | 0.110 | - 0.084 |
| Gender | 0.034 | - 0.108 |
| Length of hospitalization | 0.068 | - 0.044 |
| Days since hospital admission | 0.031 | - 0.047 |
| Covid-19 severity | - 0.027 | - 0.047 |
| Fatigue | - 0.305** | - 0.218* |
| Level of activity | - 0.021 | - 0.133 |
| Changes in breathlessness in daily activities | 0.037 | - 0.073 |
| Changes in pain perception | - 0.036 | - 0.088 |
| Model Goodness of Fit | ||
| B constant | 47.845*** | 57.039*** |
| F-value | 1.880* | 2.846** |
| R | 0.326 | 0.391 |
| R2 (%) | 10.6 | 15.3 |
Abbreviations; PCS, Physical Component Scale; MCS, Mental Component Scale.
a Note: * P < 0.05; ** P < 0.01; ***P < 0.001.
Table 4 shows the association between the study’s independent variables. The total score and the scores of the mental and physical subscales of MFI-20 were negatively associated with the level of physical activity (measured by IPAQ). The mental fatigue subscale of MFI-20 was only associated with COVID-19 severity, while the physical fatigue subscale was positively associated with not only COVID-19 severity but also changes in pain and breathlessness perception post-COVID-19. In addition, COVID-19 severity was positively associated with changes in the perception of pain and breathlessness and the total score of MFI-20.
| Variables | Gender | Age | Physical Activity Level | Days in Hospital | Days Since Symptom Onset | COVID-19 Severity | Changes in Breathlessness | Feeling Pain | General Fatigue | Physical Fatigue | Reduced Activity | Reduced Motivation | Mental Fatigue | Total Fatigue |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | 1 | |||||||||||||
| Age | 0.074 | 1 | ||||||||||||
| Physical activity level | 0.103 | -0.008 | 1 | |||||||||||
| Length of hospitalization | 0.254** | 0.329** | - 0.059 | 1 | ||||||||||
| Days since symptom onset | 0.291** | 0.230** | 0.141 | 0.241** | 1 | |||||||||
| COVID-19 severity | 0.248** | 0.462** | - 0.039 | 0.592** | 0.252** | 1 | ||||||||
| Changes in breathlessness | 0.083 | 0.162* | - 0.156 | 0.204* | 0.067 | 0.307** | 1 | |||||||
| Changes in pain | 0.002 | 0.146 | 0.018 | 0.143 | 0.102 | 0.307** | 0.450** | 1 | ||||||
| General fatigue | - 0.138 | 0.077 | - 0.211** | 0.107 | - 0.012 | 0.230** | 0.221** | 0.401** | 1 | |||||
| Physical fatigue | - 0.144 | 0.198* | -0.255** | 0.091 | - 0.049 | 0.221** | 0.217** | 0.350** | 0.823** | 1 | ||||
| Reduced activity | -0.095 | 0.074 | -0.263** | 0.158 | - 0.015 | 0.223** | 0.059 | 0.185* | 0.637** | 0.647** | 1 | |||
| Reduced motivation | -0.117 | 0.078 | -0.272** | 0.113 | - 0.088 | 0.198* | 0.112 | 0.114 | 0.646** | 0.660** | 0.498** | 1 | ||
| Mental fatigue | - 0.055 | 0.058 | - 0.267** | 0.132 | - 0.135 | 0.177* | 0.011 | 0.061 | 0.600** | 0.613** | 0.613** | 0.651** | 1 | |
| Total fatigue | -0.133 | 0.119 | - 0.298** | 0.140 | - 0.066 | 0.250** | 0.156 | 0.278** | 0.890** | 0.900** | 0.806** | 0.810** | 0.807** | 1 |
a Note: * P < 0.05; ** P < 0.01.
5. Discussion
The results of the present study revealed that more extreme fatigue was associated with poor physical and mental health at 6 months post-COVID-19. In addition, worsening pain and dyspnea and lower levels of physical activity were related to greater fatigue perception. All persistent symptoms were associated with COVID-19 severity at the acute phase of the disease. Around 40% of the patients in the present study perceived greater fatigue in the post-COVID-19 period. Fatigue is one of the most frequently reported post-COVID-19 symptoms in both hospitalized and non-hospitalized COVID survivors (14, 15). Persistent fatigue (lasting for 6 months or longer) is considered chronic fatigue, which is a pathological condition (16). Fatigue is not only the feeling of constant extreme tiredness but also is associated with a range of adverse effects, such as a lack of energy, motivation, and concentration for daily physical and mental activities, thereby negatively impacting physical and mental health (17) Individuals feeling more levels of fatigue are more likely to have work absenteeism, decreased physical activity, and increased non-specific physical problems (18) The association between post-COVID-19 fatigue and mental health problems can be bidirectional. Many COVID-19 survivors (38.8%) complain of their inability to accomplish their daily activities as before contracting the coronavirus infection, so they may lose control of parts of their lives, thereby leading them to feel lonely and isolated. This vicious cycle places patients in a distressing position and eventually makes them vulnerable to mental health problems (18). Approximately 23% of individuals with fatigue report concomitant psychological problems (19), and people with anxiety and depression report higher fatigue levels than the general population (20, 21). Townsend et al. found a strong association between post-COVID-19 fatigue and anxiety symptoms (22). The prevalence of several psychological symptoms, such as depression, anxiety, and post-traumatic distress syndrome (PTSD), has been reported to be high in recovered individuals following contracting COVID-19. (23). The stress perceived during the COVID-19 pandemic, including during the implementation of quarantine and social distancing and isolation regulations, might be another strong risk factor for long-term fatigue (24). Although psychological symptoms and fatigue have clinical interactions, they are distinct phenomena, and post-COVID-19 fatigue cannot be explained by psychological problems (25). It has been suggested that patients with chronic fatigue and mental health problems can benefit from cognitive behavior therapy (26), which can also be admitted via the Internet and smartphones (26).
The findings of the present study also indicated greater fatigue, worsened pain, exaggerated breathlessness, and low physical activity during the post-COVID-19 period in hospitalized and ICU-admitted patients compared to non-hospitalized patients. An association has already been reported between COVID-19 disease severity at the acute phase and the severity of post-COVID-19 symptoms (2). Nevertheless, Towsend et al. identified no association between COVID-19 severity and fatigue (14). This discrepancy could be due to the longer time interval between symptom onset and follow-up in our study (>20 weeks, mean of 6 months) compared to Towsend’s study (mean of 10 weeks). Long COVID-19 is defined as the persistence of symptoms beyond 12 weeks after disease presentation (1). Therefore, it can be noted that hospitalized COVID-19 survivors may experience greater fatigue compared to non-hospitalized survivors in the long run. In addition, our results revealed that fatigue severity was associated with the perception of more severe pain and breathlessness. Also, fatigue severity, but not demographic factors and the level of physical activity, was associated with physical and mental health, emphasizing the impact of fatigue on HRQoL.
In order to decrease fatigue, special attention should be paid to other post-COVID-19 symptoms. Accordingly, the findings of the present study indicated that the aggravation of pain and breathlessness perceived during the post-COVID-19 period was associated with greater physical fatigue. In line with our findings, post-COVID-19, breathlessness and fatigue have been observed to be correlated with each other (27). People feeling breathlessness may tend to limit their activities of daily living, thereby resulting in a vicious cycle contributing to greater physical fatigue and reduced HRQoL. Accordingly, the results of the present study revealed more profound fatigue among individuals with lower levels of physical activity. Fatigue by itself may justify the lack of exercise or physical activity (28), immobility, and a sedentary lifestyle, which can, in turn, lead to persistent fatigue. Physical exercise is believed to decrease fatigue and promote HRQoL, regardless of the exercise type.
Based on the findings of the present study, almost half (47%) of COVID-19 survivors reported worsened or new pain and one-third (30%) reported worsened breathlessness. Consistently, Sahin et al. found that 50% of their patients reported greater post-COVID-19 pain (29), and Huang et al. reported a prevalence of 30% for breathlessness in COVID-19 patients at 6 months post-infection (4). Since not all COVID-19 patients with lung damage perceive breathlessness post-infection, other factors can have a contributing role (30). Both breathlessness and pain are among the symptoms that involve the sensory and affective dimensions, which are measured subjectively (30). Biological, psychological, and social factors can have an impact on the perception of breathlessness and pain (30). In this regard, pain and breathlessness should be treated using comprehensive rehabilitation, including respiratory muscle training, stress and anxiety reduction measures, education, and behavioral interventions.
Finally, our findings suggested that people experiencing post-COVID-19 symptoms should be monitored for a period greater than 6 months and receive rehabilitation interventions to alleviate these symptoms, especially fatigue, and help patients safely pursue their daily physical activities. Moreover, self-management strategies should be implemented to reduce fatigue, and aid recovered patients in confronting barriers to a better quality of life.
5.1. Limitations
The present study has some limitations. First, a significant number of patients declined to participate, possibly increasing the risk of selection bias as the patients included might have had either milder persistent symptoms and better HRQoL, as well as better physical and mental health conditions, or even more severe post-COVID-19 symptoms, motivating them to participate in the study. Second, the patients were asked to report their pre-COVID-19 physical symptoms. Thus, our findings could have been influenced by recall bias. Finally, cultural and social variations might have differently influenced the value of the aspects related to HRQOL participants’ HRQoL. Because of the aforementioned, the results of this correlational study should be interpreted cautiously.
5.2. Conclusions
Fatigue was a relatively frequent phenomenon in the post-COVID-19 period and was associated with both physical and mental health dimensions of HRQoL. Fatigue also predicted greater perceived pain and breathlessness and lower physical activity post-coronavirus infection. Therefore, continuous monitoring of symptoms in these individuals is required to offer them proper rehabilitation interventions. Understanding the post-COVID-19 symptoms related to poor HRQoL may provide insights into how to develop effective health interventions for coronavirus survivors. More research is needed to investigate possible therapeutic options to reduce fatigue and guide patients during the COVID-19 recovery period. Longitudinal studies are highly recommended to determine the long-term impacts of persistent fatigue on different aspects of well-being in life and at work. In addition, research is required to address the causes of long-lasting fatigue, and special attention should be paid to the rehabilitation needs of patients with long-lasting fatigue.