1. Context
Around 234.2 (95% CI, 187.2 - 281.2) million major surgeries are annually performed in the world, including an estimated number of 13 852 308 gastrointestinal (GI) tract surgeries (1, 2). Postoperative pain is the leading cause of patient complaints after surgery. Moderate-severe to severe pain after surgery occurs in 29.7% and 10.9% of cases, respectively (3). Pain, in particular, is a common poorly controllable problem following abdominal surgery (4).
Acute postoperative pain is a key risk factor for chronic postoperative pain; therefore, it should be effectively controlled (5, 6). Despite recent advances in postoperative pain management, opioids are still the mainstay treatment for controlling pain after a variety of medical procedures. The common side effects of these medications include respiratory depression, nausea, vomiting, pruritus, ileus, and constipation (7). Local anesthetics blocking peripheral nerves are becoming popular agents to relieve postoperative pain in patients undergoing various open surgeries and to minimize the need for opioids (8).
Lidocaine is one of the anesthetics used to alleviate acute pain early after surgery. The routes of lidocaine administration include topically, intravenously (IV), local subcutaneously, submucosal infiltration, spraying, nerve blocking, or skin patches. A meta-analysis of randomized controlled trials showed that the use of IV or topical lidocaine decreased the severity of pain following GI endoscopic procedures (9). The benefits of topical analgesia include targeted drug delivery, no need for oral administration, and minimal systemic side effects. Local anesthetics block the transmission of pain signals and are useful for treating acute and chronic nociceptive and neuropathic pain (10).
The US Food and Drug Administration (FDA) has approved lidocaine patches as pain-relieving agents for treating postherpetic neuralgia and persistent neuropathic pain syndrome. Lidocaine patches have been shown to alleviate pain associated with postherpetic neuralgia within 30 min of administration (11). Although lidocaine has been reported to be a beneficial pain-reducing agent in some conditions, such as diabetic peripheral neuropathy, carpal tunnel syndrome, low back pain, and osteoarthritis pain, there is a paucity of data on the effectiveness of lidocaine patches in the treatment of non-postherpetic neuralgia pain (10).
While lidocaine patches seem to be effective in ameliorating postoperative pain following a variety of procedures, such as laparoscopic surgeries, midline incision gynecological surgery, and radical prostatectomy (12-14), their effectiveness is questionable in other conditions (eg, total knee replacement arthroplasty, robotic heart surgery, thoracotomy, and sternotomy) (15-18). Post-operative pain management in GI surgery affects patient recovery time, length of hospitalization, and patient satisfaction (19). There is no conclusive review on the efficacy of lidocaine patches in the management of postoperative pain after GI surgeries. Therefore, this review aimed to explore the pain-reducing efficacy of lidocaine patches in individuals undergoing surgery for GI problems.
2. Evidence Acquisition
2.1. Search Strategy and Data Collection
The literature search was conducted in PubMed, Scopus, and Web of Science databases, as well as in the Google Scholar search engine up to June 2023. Relevant keywords and their combinations used for the literature search were as follows: "[(digestive system surgical procedures [MeSH Terms]) OR abdominal surgery OR gastrointestinal surgical procedures) AND (postoperative pain), AND ((lidocaine [MeSH Terms]) OR lidocaine patch)]."
2.2. Inclusion Criteria and Data Extraction
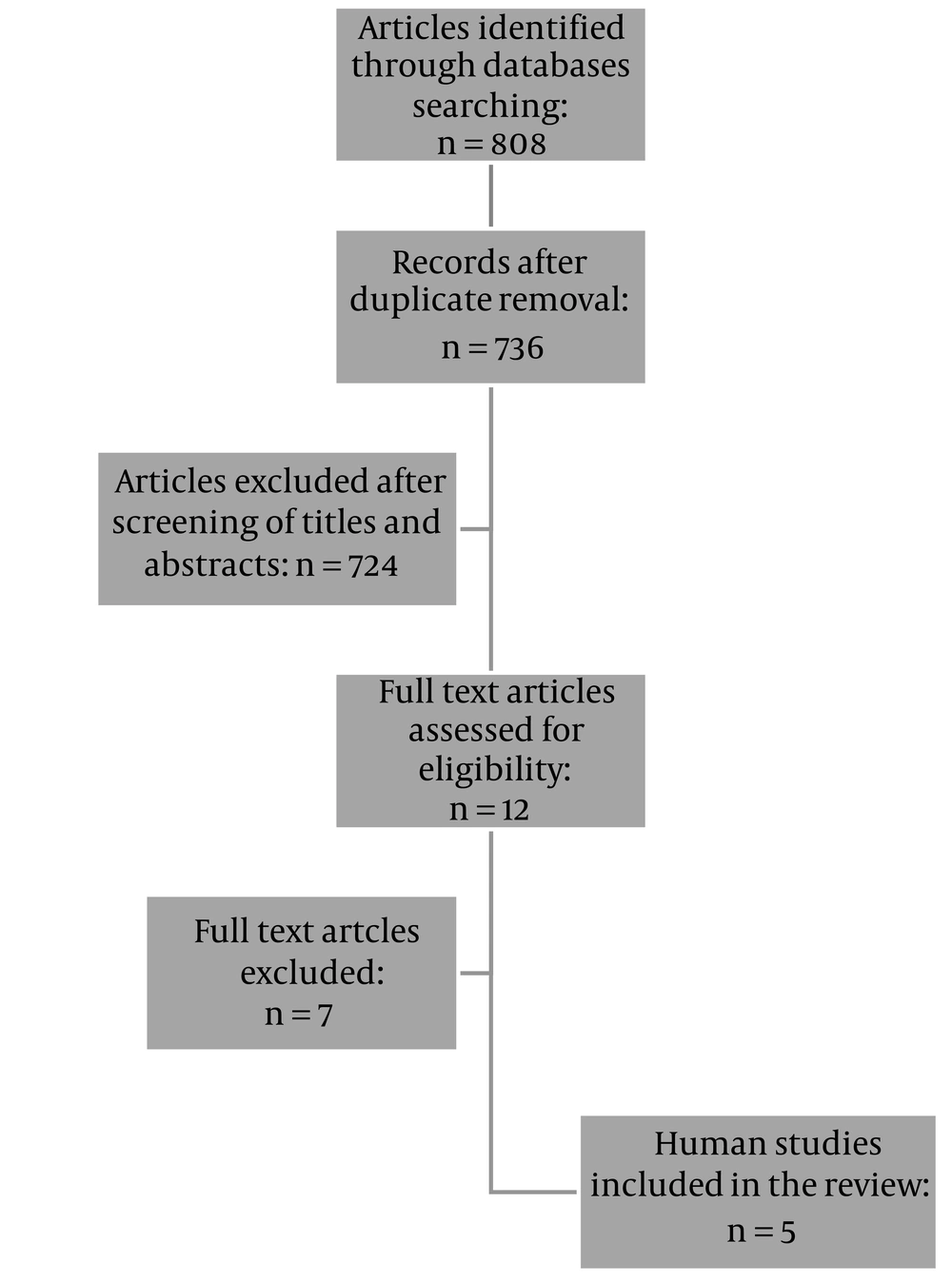
We included clinical trials that investigated the effects of lidocaine patches in individuals undergoing GI surgeries. Duplicates (n = 72) were then excluded, leaving a total of 736 articles for further assessment. After reviewing the titles and abstracts of the remaining articles and removing irrelevant studies (n = 697) and those conducted on patients undergoing non-GI surgeries (n = 27), 12 studies were chosen for full-text review. Finally, an additional 7 studies that used injectable, intraperitoneal, or local lidocaine were excluded; thus, 5 studies were included in the final review (Figure 1). Independent data extraction was conducted by 2 authors (MB and FAS). The following data were extracted from the eligible studies: the first author's name, year of publication, study location, study population, number of participants in study groups, interventions, other analgesic medications used to relieve pain, and outcomes.
3. Results
Elhafz et al. conducted a randomized clinical trial (RCT) to assess the efficacy of lidocaine patches in reducing postoperative pain in patients undergoing laparoscopic colorectal surgery (20). In the recent study, patients with allergies to lidocaine, respiratory problems, cardiac dysfunction, arrhythmias, inflammatory bowel disease, and liver or kidney diseases, as well as those using antiarrhythmic drugs and long-term users of analgesics and corticosteroids, were excluded. A total of 30 participants were divided into 3 groups. One group received intravenous saline (group 1, n = 9), another group received intravenous lidocaine after anesthesia (group 2, n = 9), and the last group was treated with 3 patches of 5% lidocaine (group 3, n = 9). The Visual Analog Scale (VAS) was used to determine pain severity at rest and during coughing. Mean VAS scores during the first 72 h at rest and during coughing were significantly lower in groups 2 (intravenous lidocaine) and 3 (lidocaine patches) compared to group 1 (control; P < 0.05 for all comparisons). However, there was no significant difference between groups 2 and 3, and pain intensity did not significantly differ between the study groups at 72 h after surgery. In addition, the need for morphine was significantly lower in the groups receiving lidocaine than in the placebo group (P < 0.05; Table 1).
| Year | |||||
|---|---|---|---|---|---|
| 2012 | 2021 | 2018 | 2013 | 2009 | |
| Author | Elhafz et al. (20) | Kim et al. (21) | Lee et al. (22) | Bischoff et al. (23) | Saber et al.(24) |
| Location | Egypt | Korea | Korea | Denmark | USA |
| Participants and sample size | Patients undergoing elective colorectal surgery, n = 30 | Patients undergoing laparoscopic cholecystectomy, n = 63 | Patients undergoing laparoscopic appendectomy, n = 40 | Patients with persistent inguinal post-herniorrhaphy pain, n = 21 | Patients undergoing laparoscopic ventral hernia repair, n = 30 |
| Intervention | One group received intravenous saline (group 1), another group received intravenous lidocaine infusion post-anesthesia (group 2), and the last group received three 5% lidocaine patches. | One group received 5% lidocaine patches + dressing retention tapes on both shoulders, and the control group received only the dressing retention tape. | Participants received either 5% lidocaine patches or placebo patches on each side of the umbilical trocar. | In a crossover study, men with PIPP received either 5% lidocaine or placebo patches for 14 days with a 14-day wash-out period. | One group received a lidocaine patch on the anterior abdominal wall (group A), and the second group did not receive the patch (group B). |
| Other analgesic medications used to relieve pain | For anesthesia: Fentanyl and Propofol; For intubation: cisatracurium; For maintenance: Isoflurane, In recovery room: Fentanyl, Morphine | ||||
| For anesthesia induction: Propofol, Remifentanil, and Rocuronium; For maintenance: Remifentanil and Sevoflurane; 10 min prior to the end of surgery: Paracetamol, Neostigmine and Glycopyrrolate; Post-operative: Fentanyl, Ketorolac, and Nefopam; After discharge: Acetaminophen/tramadol | For anesthesia: Propofol and Fentanyl or thiopental sodium; For intubation: Vecuronium bromide; For maintenance: Sevoflurane and Vecuronium bromide | ||||
| Acetaminophen, NSAIDs, gabapentin, opioids. | Acetaminophen, hydrocodone, or morphine. | ||||
| Results | The means of pain scores in the first 72 h at rest and during coughing were significantly lower in groups 2 and 3 compared to group 1, with no significant differences between groups 2 and 3. In addition, the need for morphine use was significantly lower in the groups receiving lidocaine than in the placebo group. | ||||
| The overall incidence of shoulder pain was significantly lower in the lidocaine patch group than in the control group. The severity of shoulder pain at 24 h and 48 h after surgery was also significantly lower in the lidocaine patch group compared to the control group. The total dose of remifentanil needed did not significantly change in the lidocaine patch group compared to the control group. | A non-significant reduction was reported in the postoperative pain score in both abdominal and shoulder areas in the lidocaine group. The patients treated with 5% lidocaine patches needed lower amounts of pethidine than those treated with placebo patches. | No significant difference was observed in pain intensity between the groups. | Group A had a significant reduction in the pain score only at the time of discharge compared to the second group. Group A required a non-significant lower need for analgesic use than group B. | ||
Studies’ Characteristics
In another RCT, Kim et al. investigated the analgesic effects of 5% lidocaine patches on shoulder pain after laparoscopic cholecystectomy (21). The patients were excluded if they had histories of infections, surgery, traumas, chronic pain involving shoulders, allergies to local anesthetics, chronic abuse of opioids, and liver or kidney diseases. A total of 63 female patients were randomly allocated to one of the following 2 groups: lidocaine patches (applying 5% lidocaine patches + dressing retention tapes on both shoulders, n = 31) and control (dressing retention tapes only, n = 32). The intensity of abdominal and shoulder pain was measured using the Numeric Rating Scale (NRS) at the baseline and 30-min, 6-h, 24-h, and 48-h postoperative. The overall incidence of shoulder pain was significantly lower in the lidocaine patch group than in the control group (42% vs 78%; P = 0.005), and the severity of shoulder pain at 24 and 48 h after surgery was also significantly lower in the lidocaine patch group compared to the control group (P = 0.01 and 0.015, respectively). However, the total dose of remifentanil needed did not significantly differ between the lidocaine patch and control groups (P = 0.055; Table 1).
Lee et al., in their RCT, evaluated the pain-reducing effectiveness of lidocaine patches in patients undergoing laparoscopic appendectomy (22). Exclusion criteria included receiving topical anesthetics or nonsteroidal anti-inflammatory drugs, regularly taking analgesics, and having a history of chronic pain or neurological impairments. In this study, 40 participants were randomized to receive either 5% lidocaine patches or a placebo, which were placed on each side of the umbilical trocar. The VAS was used to assess pain intensity at 0, 6, 12, 18, 24, 30, 36, and 48 h after surgery. A non-significant reduction was reported in both abdominal and shoulder pain in lidocaine-treated patients at all intervals assessed. In addition, the patients treated with 5% lidocaine patches needed lower doses of pethidine than those treated with a placebo (P < 0.001; Table 1).
In another RCT, Bischoff et al. investigated the efficacy of lidocaine patches in alleviating persistent inguinal post-herniorrhaphy pain (PIPP) (23). Exclusion criteria were allergy to local anesthetics, skin problems at the application site, heart, liver, or kidney diseases, recurrent hernia, drug or alcohol abuse, neuronal and mental problems, and bilateral groin pain. In this crossover study, 21 men with PIPP received either 5% lidocaine patches or a placebo for 14 days with a 14-day wash-out period. Pain intensity was assessed using the NRS at rest, during movements, and during palpation of the groin. No significant difference was observed in pain intensity between the groups (P = 0.33; Table 1).
Saber et al. conducted an RCT to investigate the effects of 5% lidocaine patches on postoperative pain following laparoscopic ventral hernia repair (LVHR; n = 30) (24). Pain severity was recorded at discharge, as well as 2 weeks and 2 months after the surgery, using the Verbal Rating Score (VRS), indicating a significant difference between the lidocaine patch and control groups only at the time of discharge (P = 0.0067). The group receiving 5% lidocaine patches needed less use of analgesics than the control group, but this difference was statistically insignificant (Table 1).
4. Discussion
This narrative review provides an overview of the pain-relieving effects of lidocaine patches in patients undergoing GI surgical procedures. Overall, only 3 out of the 5 studies reviewed reported that lidocaine patches significantly reduced pain compared to control drugs and placebos (20, 21, 24). Another study reported a reduction in pain intensity in lidocaine patch receivers, but this finding was statistically insignificant (22). All studies included in this review were randomized controlled clinical trials, 3 of which employed a double-blind design (21-23), and 1 study had a cross-over methodology. In these studies, both acute and chronic types of pain were evaluated, and all of them reported a significant or marginally significant decrease in the need for opioids in the lidocaine patch group.
In 4 of the studies, patients underwent laparoscopic surgery, a procedure associated with abdominal and shoulder pain (20-22, 24). Abdominal pain results from port ulcers, surgery-induced tissue damage, and pneumoperitoneum, while shoulder pain after laparoscopic surgery is believed to be due to the stretching of the subdiaphragmatic fibers of the phrenic nerve as a result of the increased concavity of the diaphragm, which is induced by the pneumoperitoneum and the consequent loss of visceral surface tension (12). Only 2 of the studies reported that lidocaine patches were effective in reducing both abdominal and shoulder pain following laparoscopic surgery (21, 22).
The results of the studies evaluating the usefulness of lidocaine patches in alleviating postoperative pain are inconclusive. A meta-analysis study reported that lidocaine patches might not be effective in managing postoperative pain (25), while another systematic review noted that lidocaine patches effectively reduced acute pain after elective surgeries (26). The number of studies included in these reviews was relatively small, and some of these studies had small sample sizes and did not employ appropriate blinding strategies. The meta-analysis of 16 randomized controlled trials by Wu et al. showed that lidocaine patches had beneficial effects on postoperative pain and reduced opioid use without any significant increase in patient satisfaction (27). The present review does not have the limitations of Wu et al.’s study regarding homogeneity in the dose and time of applying lidocaine patches, as well as the type of surgery. Each dermal lidocaine patch contains 700 mg of the active substance (ie, lidocaine). According to the standard protocol, up to 3 patches can be applied to cover the affected area for up to 12 h during a 24-h period. Lidocaine can block sodium channels on nociceptors but not on large myelinated Aβ fibers, a phenomenon that occurs in targeted peripheral analgesia. Thus, despite the existence of analgesic effects, the patient may not feel numbness at the site of the application of lidocaine patches (18).
The most common side effect is mild dose-dependent transient skin irritation at the application site. The amount of drug absorption correlates with skin thickness, surface area, and local vascularity at the site of application, as well as with the duration of patch application (28). These factors can explain the differences observed in the results of various studies.
It is noteworthy that lidocaine patches deliver lidocaine to the intact skin around the wound instead of directly to the wound, resulting in different outcomes compared with when the wound is directly infiltrated (29). Besides, lidocaine diffuses from patches to the epidermis and then to the deeper parts of the skin instead of spreading under the epidermis or even under the dermis as it occurs during wound infiltration (30, 31). As mentioned, lidocaine diffused out of patches has minimal systemic absorption, which can limit its analgesic effects. Other reasons justifying variabilities in the findings of these studies can be different scales used to assess pain intensity, relatively small sample sizes, and different control groups (eg, placebo, active drug, etc). Although pain severity assessment tools are generally valid and reliable, the type of instrument used for this goal can affect the results as well. The degree of agreement and sensitivity of the 2 scales of VAS and NRS in evaluating acute pain after surgery are almost equal and higher than those of the VRS. The 4-point VRS seems to underestimate pain severity compared to VAS at different times during surgery (32). Finally, the type and site of pain, as well as the patient’s condition during pain assessment (eg, on movement, during coughing, or at rest), can explain different findings in studies. Thus, it seems too premature to draw a definite conclusion on the pain-reducing efficacy of lidocaine patches in patients undergoing surgeries.
The main strength of this review is that we have included randomized controlled clinical trials evaluating both acute and chronic pain. However, some papers could have been missed, which may limit our results.
4.1. Conclusions
Considering the potential efficacy of lidocaine patches in reducing pain and the need for opioid use following abdominal surgeries, it seems necessary to conduct studies with larger sample sizes to clarify this issue.