1. Background
Urbanization and advancements in transportation have significantly reduced physical activity, leading to a global issue of obesity (1). Over the years, various scales, such as Body Mass Index (BMI), have been used to assess and evaluate physical health and fitness (2-4). Body Mass Index serves as the basis for many current classifications of overweight and is widely used, from global surveillance to individual patient assessment, often performing well in various contexts (5). In recent decades, the relationship between body composition and BMI has gained research interest across fields, with BMI increasingly viewed as an uncertain method for diagnosing obesity (6). Studies examining both BMI and body composition have shown that a substantial number of individuals with a BMI below 30 kg/m² are also classified as obese, indicating misclassification (7). Nonetheless, BMI remains a key metric for assessment and inference in numerous health and clinical studies (8-13), and in some cases, it has been cited as a strong predictor of metabolic syndrome (14). During the coronavirus pandemic, a BMI ≥ 25 was identified as a significant risk factor for contracting the virus (15).
Research findings indicate that comprehensive lifestyle interventions can reduce body fat percentage, though these changes may not be reflected in BMI, suggesting BMI may be insufficient for evaluating intervention success in obesity management (16). Studies by Chung also support BMI's limitations in distinguishing between fat and fat-free body masses (17). Given the limited research on various age and gender groups, particularly among women—a highly vulnerable population (18)—and considering that the reproductive period represents a sensitive nutritional stage for women (19).
2. Objectives
this study was initiated to compare BMI with body composition assessment using Bioelectrical Impedance Analysis (BIA) among women of reproductive age in Damghan, under the coverage of Semnan University of Medical Sciences, Iran.
3. Methods
3.1. Study Design
The present study is a community-based descriptive cross-sectional study.
3.2. Setting/Participants
In this study, 182 eligible women covered by selected urban comprehensive health service centers in Damghan, under the jurisdiction of Semnan University of Medical Sciences, Iran (2017 - 2019), were included. Due to the importance of observing safety during pregnancy and lactation, non-pregnant women aged 30 - 45 years, without a history of underlying diseases or physician-imposed restrictions on physical activity, were selected as the target population and enrolled through a simple random sampling method.
3.3. Sample Size
In a study conducted by Stojković et al. (20), the correlation coefficient between BMI and body fat percentage was determined to be 0.361, while the correlation coefficient between BMI and skeletal muscle percentage was -0.344. Since selecting a smaller r value results in a larger sample size, the researchers opted for a correlation coefficient of r = -0.344. By considering a type I error of 0.05 (z0.975 = 1.96) and a power of 90% (z0.9 = 1.28) and substituting into the following formula (21):
W = 0.36 was obtained, and by substituting W into the following formula:
The minimum sample size for this study was determined to be 85 individuals. Considering this, 182 samples were included in the study using simple random sampling and were subsequently examined.
3.4. Data Collection Method
Informed consent was obtained from all participants. Each participant was individually assessed by two trained evaluators simultaneously. To avoid bias, both participants and evaluators were unaware of the study objectives. A questionnaire was administered through interviews with all participants, and body composition was assessed using the bioelectrical impedance method.
3.4.1. Assessment of Demographic and Social Data
A structured questionnaire was used to collect information on individual and social characteristics. Data for each participant were gathered through interviews and questionnaire completion.
3.4.2. Body Composition Assessment Tool
To assess body composition, including weight, body mass index, skeletal muscle percentage, total body fat, and visceral fat, an Omron BF511 adult bioelectrical impedance scale with an accuracy of 0.1 kilograms was used (22). This device is digital, portable, and non-invasive. Muscles, blood vessels, and bones contain higher water content and easily conduct electricity, while fat tissue has weaker electrical conductivity. The Omron BF511 passes a very weak electrical current (50 kHz and less than 500 µA) through the body to determine fat tissue content. This weak electrical current is not felt when using the Omron BF511 bioelectrical impedance scale.
In other words, to assess body composition, the device must be calibrated for electrical impedance based on each participant's height, age, and gender. Fluid shifts from the upper body to the lower body occur during the day, causing the legs and lower regions to swell in the afternoon and evening, resulting in different fluid balances between the upper and lower body in the morning and evening. To reduce the impact of irregular fluid distribution on measurement results, the Omron BF511 has separate electrodes for both hands and feet. The Omron BF511 is capable of calculating weight, Body Mass Index, body fat percentage, skeletal muscle mass, and resting body metabolism.
Each participant was assessed in the presence of two interviewers for approximately 15 minutes. During the body composition assessment, female participants wore lightweight clothing without shoes, keys, mobile phones, or other items. Since the Omron BF511 device needs to be individually calibrated for each participant, data related to height, age, gender, and the average length of 10 steps (in normal walking) taken by each participant were recorded and entered into the device. Participant height was measured using a standard wall-mounted meter in urban comprehensive service centers. In this study, the bioelectrical impedance of the BF511 scale, manufactured in China, was used.
3.5. Statistical Methods
The data obtained were analyzed and evaluated based on the standard values provided by the tool manufacturer and using SPSS-27 software. In this study, to compare the effectiveness of "body mass index" in the accurate classification of individuals, additional indices such as total body fat percentage, visceral fat percentage, and skeletal muscle percentage were also considered. Descriptive statistics were used in this analysis. Furthermore, since the study aimed to evaluate the agreement between two evaluators (the BMI criterion and anthropometric indices), the kappa agreement coefficient was applied (23).
4. Results
In this cross-sectional descriptive, population-based study, 182 women with a mean age (standard deviation) of 37.26 (5.33) years, mean weight of 70.09 (11.13) kilograms, and mean height of 159.76 (6.14) centimeters were examined. Among the participants, the mean body mass index (BMI) was 27.47 (4.37), skeletal muscle mass was 24.98 (3.04) percent, visceral fat was 6.93 (2.13) percent, and body fat was 40.06 (6.52) percent. Based on the BMI index, 56 women (30.8%) were classified as having a normal status, 74 women (40.7%) as overweight, 51 women (28%) as obese, and only 1 woman (0.5%) as underweight. In contrast, based on the body fat index, only 25 individuals (13.7%) were classified in the normal or underweight group, with the remaining individuals categorized as overweight and obese (Table 1).
| Variables | Total Body Fat | Total | Incorrect Classification | Correct Classification | |||
|---|---|---|---|---|---|---|---|
| Low | Normal | High | Very High | ||||
| Thin | 0 | 1 | 0 | 0 | 1 | 100 | 0 |
| Normal | 1 | 18 | 30 | 7 | 56 | 68 | 32 |
| Overweight | 1 | 3 | 20 | 50 | 74 | 32 | 68 |
| Fat | 0 | 1 | 0 | 50 | 51 | 2 | 98 |
| Total | 2 | 23 | 50 | 107 | 182 | 52 | 48 |
a Values are expressed as (%).
The kappa agreement coefficient was 25% (P-value < 0.001), indicating poor agreement between these two indices for classifying individuals. The performance of the body mass index compared to the visceral fat index was also weak, misclassifying 68% of individuals and placing 107 individuals (59%) with normal visceral fat in the overweight and obese categories (Table 2).
| Variables | Visceral Fat | Total | Incorrect Classification | Correct Classification | ||
|---|---|---|---|---|---|---|
| Normal | High | Very High | ||||
| Thin | 1 | 0 | 0 | 1 | 100 | 0 |
| Normal | 56 | 0 | 0 | 56 | 66 | 34 |
| Overweight | 72 | 2 | 0 | 74 | 89 | 11 |
| Fat | 35 | 16 | 0 | 51 | 100 | 0 |
| Total | 164 | 18 | 0 | 182 | 68 | 32 |
a Values are expressed as (%).
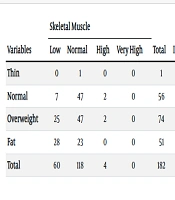
The agreement level obtained by the kappa coefficient between BMI and visceral fat percentage was -0.031, indicating a lack of agreement between these two variables (P-value = 0.004). When comparing BMI with skeletal muscle percentage, the error rate was 73%, with the highest error rate among individuals classified as normal. Only 40% of individuals with a normal skeletal muscle percentage were correctly placed in the normal BMI category (Table 3). The calculated kappa coefficient for these two indices was 0.075, which is very weak (P-value = 0.001).
| Variables | Skeletal Muscle | Total | Incorrect Classification | Correct Classification | |||
|---|---|---|---|---|---|---|---|
| Low | Normal | High | Very High | ||||
| Thin | 0 | 1 | 0 | 0 | 1 | 100 | 0 |
| Normal | 7 | 47 | 2 | 0 | 56 | 60 | 40 |
| Overweight | 25 | 47 | 2 | 0 | 74 | 50 | 50 |
| Fat | 28 | 23 | 0 | 0 | 51 | 0 | 100 |
| Total | 60 | 118 | 4 | 0 | 182 | 73 | 27 |
a Values are expressed as (%).
5. Discussion
The findings of this cross-sectional descriptive study on calculating BMI based on body fat percentage among participants revealed that BMI is unable to accurately identify cases of underweight. Additionally, BMI correctly identified only 32% of normal cases, 68% of overweight individuals, and 98% of obese women, while misclassifying 52% of all cases. Furthermore, this study indicates that calculating BMI based on the visceral fat index is even more concerning, as it failed to correctly classify 68% of cases. Considering body fat index classifications in comparison with BMI classifications, the highest misclassification rate was observed in the underweight and normal groups. Among the 56 participants classified as "normal BMI," only 18 had a normal body fat index, while 37 (66%) had a "high or very high" body fat index. Additionally, findings showed that BMI classification based on skeletal muscle percentage was not highly accurate, with BMI misclassification occurring in 73% of cases.
Studies by Westerterp indicate that exercise leads to healthier body composition, reflected by reduced body fat, especially in overweight and obese individuals, with minimal or no long-term effect on weight (24). This finding underscores the challenge of assessing changes in each of the anthropometric and body composition parameters. Aires et al. found that over time, both normal-weight and overweight/obese participants experienced an increase in BMI (2). However, interpreting changes in anthropometric and body composition parameters remains difficult, and despite these uncertainties, BMI continues to underpin many health assessments. For example, studies have demonstrated a significant relationship between waist circumference and BMI among women (25), which, based on this research, warrants reevaluation. Additionally, in a study conducted by Pflanz et al. on 15,643 biobank samples, regional associations between central obesity and subcortical gray matter nuclei were observed (26). This finding has been referenced and applied, yet in many studies of this nature, changes in body composition have not been the primary focus. The findings of this research introduce new questions regarding the interpretation of such studies.
For many years, BMI has been central to numerous judgments and decisions across various fields, especially in health and disease (8-13). Body Mass Index is widely accepted as a scale for assessing underweight, overweight, obesity, and malnutrition (27). However, BMI has not always been a reliable indicator for individual health assessment, and anthropometric indices may be more effective in this regard (20). Evidence from this research highlights the need for increased scientific rigor and reflection among health-related decision-makers. It suggests that BMI may not be a suitable indicator for assessing physical health or an accurate measure for evaluating the success of health management interventions. Nevertheless, further studies on other population groups and diverse communities are essential.
5.1. Limitations
Although this study used accurate measurement tools and data collection was conducted simultaneously by two individuals, there are limitations. The study focused solely on women aged 30 to 45, and the selection of participants from selected comprehensive health service centers also presents a limitation.
5.2. Suggestions
Future studies should include individuals from other age and gender groups. It is recommended to conduct research in larger populations with broader sample sizes. Extensive studies across various communities could help establish patterns based on physiological, ethnic, and other social health differences. Further research should investigate socio-economic factors influencing the relationship between body composition and weight changes in different populations and explore the potential benefits of incorporating body composition assessments into routine health evaluations and interventions.