1. Background
Survivors of COVID-19, also known as SARS-CoV-2 or severe acute respiratory syndrome coronavirus 2, who experience lingering symptoms or do not achieve a quick or complete recovery are referred to as "long-haulers" or are said to have "long COVID" (1). The duration of long-haul COVID or post-COVID-19 symptoms can vary from 3 to 9 months (2), and symptoms persisting longer than 12 weeks after initial recovery are considered long COVID (3). Persistent clinical parameters, signs, or symptoms that extend beyond two weeks from the onset of COVID-19 are also categorized as long COVID-19 (4, 5).
Long COVID is characterized by a wide range of symptoms, including but not limited to fatigue, shortness of breath, cognitive dysfunction, brain fog, muscle aches, chest pain, anxiety, and loss of smell and taste, with more than 200 symptoms reported (2, 6, 7). The COVID-19 pandemic has imposed a significant global burden on long-term care facilities, particularly affecting the capacity and preparedness of healthcare professionals and systems to care for long haulers. The economic impacts on the GDP can vary by country and are influenced by policies and economic structures (8).
Compounded long COVID symptoms, stemming from multiple systems such as immune, hematological, pulmonary, cardiovascular, gastrointestinal, hepatic, renal, musculoskeletal, nervous, and mental health, pose a significant challenge to healthcare delivery and outcomes (9). A study involving 273,618 participants reported that 57% and 36.65% had persistent symptoms for over six months and between three to six months, respectively, with age and gender influencing the risk of developing long COVID (10).
Recent studies have found that most post-COVID symptoms are similar between vaccinated and unvaccinated individuals (11, 12), with dyspnea, fatigue, and long-term activity impairment being commonly reported among both hospitalized and non-hospitalized COVID patients (13). In a global study of 3,762 patients, 89.1% experienced symptom relapses triggered by exercise, physical or mental stress (6-8), in addition to impaired daily activities and missed work [13].
Emerging evidence indicates that post-COVID syndrome, associated with a hyper-inflammatory host response, is linked to a spectrum of musculoskeletal issues. These include fatigue, arthralgia, myalgia, new-onset back pain, joint swelling indicative of reactive arthritis, fibromyalgia, and the new onset of rheumatic diseases, leading to diminished physical performance and muscle weakness (14-16). On the other hand, respiratory symptoms such as fatigue, dyspnea, cough, malaise, decreased pulmonary function, along with muscle and joint pain, were more prevalent in older individuals with a higher body mass index and among females (7, 17, 18). However, referrals to physiotherapy services were both non-restrictive and comprehensive.
Respiratory exercises are the cornerstone of long COVID rehabilitation. Respiratory physiotherapy for ICU patients with COVID-19 significantly increased ventilator-free days and improved survival at 90 days compared to those not receiving physiotherapy (19). A six-week program of inspiratory muscle training exercises and physical activity interventions early after the acute phase showed positive effects on post-COVID recovery (20).
Therefore, physiotherapy services are crucial after the acute phase, addressing functional ability, work, and quality of life with tailored exercise approaches to ensure a safe and gradual return to daily activities within energy limits and symptom management (21). It is vital for physiotherapists to continuously update their clinical knowledge and skills for managing long COVID through evidence-informed, evolving exercise guidelines to meet the changing needs of patients (21).
This necessity underscores the importance of exploring how physiotherapists have responded to the rehabilitation of individuals with long COVID-19. Additionally, with limited clinical placements and disruptions to hands-on training, the pandemic has forced clinicians, educators, and regulators to adapt to remote and online placements (13). The impact of these adaptations on continuing professional development and rehabilitation competencies acquired for managing long-term COVID has not been extensively studied.
Adequate knowledge and awareness of current clinical guidelines for long COVID are essential for physiotherapists to deliver safe and effective rehabilitation and for students to gain a rich learning experience (21, 22). One study highlighted a discrepancy between respiratory physiotherapists' experience in specific examination and treatment techniques and their perceived importance of those techniques (23). Therefore, exploring the knowledge, attitudes, and experiences (KAP) of clinical physiotherapists, educators, and students regarding long COVID can help identify and address learning gaps or barriers. This exploration may also provide valuable insights into the dynamics of clinical practice and the extent to which knowledge translation has occurred in long-term COVID rehabilitation, offering lessons for the future.
2. Objectives
The primary goal of this study was to capture the KAP of UAE physiotherapists and student physiotherapists regarding long-term COVID-19 rehabilitation through a cross-sectional survey. The secondary objectives were to identify gaps and offer insights into physiotherapy practices related to long-term COVID-19 rehabilitation.
3. Methods
3.1. Study Design and Setting
A cross-sectional survey was conducted among physiotherapists and physiotherapy students in the UAE from March 2022 to June 2022.
3.2. Survey Development
A systematic literature search did not yield any existing instruments related to long-term COVID-19. Consequently, a survey was developed to capture the social interactions, learning experiences, personal experiences, and behaviors of physiotherapists, utilizing guidelines and briefing reports from the World Physiotherapy Organization (22) and recent evidence on long COVID (2, 7). The questionnaire underwent review by a team of researchers and three clinical physiotherapists specializing in cardiorespiratory therapy with experience in managing long COVID. The survey instrument was then piloted on 10 participants, ranging from students to experienced physiotherapists, to assess barriers, acceptability, and the flow of the questionnaire. The pilot study, conducted online followed by in-depth face-to-face interviews, provided insights into participants' interpretation of the questions and helped refine the wording and clarity for broader application and generalization.
The results from the pilot study were used to review and refine each question, with further input from two experts to resolve any disagreements through discussion. The final survey comprised 52 questions, with expert agreement exceeding 90% for each item to ensure validity (Appendix 1). Participants responded to questions using a yes/no/not sure, agree/disagree/not sure format or by selecting all options that apply. Additionally, 5-point and 4-point Likert scales were used to measure attitudes and experiences concerning long COVID-19. The survey was administered online in English using Google Forms, with a restriction of 'one response per user' to prevent multiple submissions from a single participant.
3.3. Survey Participants
Physiotherapists and physiotherapy students in the UAE participated in the online survey between March and July 2022. Participants were blinded to the study hypothesis, and the survey was carefully worded in a neutral manner to avoid potential bias by avoiding leading questions.
Inclusion Criteria: The survey targeted both male and female physiotherapists aged between 18 and 60 years. This broad age range was chosen to encompass a wide spectrum of clinical experiences regarding long-term rehabilitation and to represent a diverse cross-section of the physiotherapy population. To gather data, the research team reached out to practicing physiotherapists in the UAE, the Emirates Physiotherapy Society, and various hospitals and clinics throughout the country. Additionally, students and alumni were contacted through the physiotherapy departments of three universities offering physiotherapy programs in the UAE.
3.4. Exclusion Criteria
Other healthcare professionals and physiotherapists located outside the UAE were ineligible to participate. The research team disseminated the online survey link via email and through social and private networks. Non-respondents to the initial invitation received two follow-up reminders spaced two weeks apart.
3.5. Ethics
The Gulf Medical University Institutional Review Board approved the study (Ref. No. IRB/COHS/STD/01/Jan-2022). Participation was anonymous and voluntary, with the completion and submission of the online survey serving as informed consent, as detailed in the questionnaire's introduction.
3.6. Data Analysis
The data were analyzed using IBM SPSS version 26.0, and graphs were created with Excel. Descriptive statistics, such as frequencies, percentages, and graphs, were utilized to present the findings. The chi-square test was applied to assess differences in categorical variables, including qualification levels, gender, and age groups, with a significance threshold set at 0.05. The analyst was blinded to the identities of the survey groups to reduce bias in data interpretation. Cronbach’s alpha was calculated to verify internal consistency.
4. Results
4.1. Response Rate
Out of 466 individuals who accessed the survey link, 434 completed the survey, yielding a response rate of 93.13%.
4.2. Participant Characteristics
The majority of the survey respondents were female (66.8%) and male (32.2%), primarily from the Mediterranean and Middle East (49.3%) and Asia (36.9%). The age distribution was as follows: 18 - 29 years (52.1%), 30-39 years (31.1%), and 40-49 years (14.1%). Most participants held a Bachelor's degree (42.9%), with 41.5% having less than 3 years of professional clinical experience and 52.8% possessing four to 15 years of experience. The most common workplace settings were private hospitals (31.1%), followed by public hospitals (20.55%) and academia-clinical settings (23%). The professional specializations reported were musculoskeletal (37.1%), neuro-physiotherapy (19.6%), and cardio-respiratory (12.7%). A significant majority of respondents were vaccinated against COVID-19 (95.6%).
Regarding caseloads, 65% of the participants managed a mix of inpatient and outpatient cases, 21% were outpatient-only, and 14% worked in home care and community sports centers. Additionally, 15% worked in long-term care and 17% in intensive care units.
4.3. Knowledge Domain
4.3.1. Survey of Participants' Knowledge of Physiotherapy Management for Acute COVID-19 and COVID-19-Related Medical Complications
A survey of the participants' knowledge of physiotherapy management for acute COVID-19 and COVID-19-related medical complications showed that 61.1% responded "Yes," indicating they believe in distinct management approaches for these conditions. Meanwhile, 21% were "Not sure," and 18% answered "No." Participants with a Master's or doctoral degree showed the highest level of agreement at 67.5%, in contrast to diploma holders at 36.4%. Participants with bachelor, master, and doctoral-level education were more likely to express a positive belief in differentiating management strategies for acute COVID-19 and its complications compared to those pursuing education and diploma holders, who could not distinguish between management strategies (X2 = 18.442, P = 0.018).
4.3.2. Long COVID Symptoms, Duration, and Risks
Concerning symptoms, 68.3% of participants reported being able to distinguish between long-term COVID-19 symptoms and complications from acute COVID-19, while 18.7% were unsure, and 13% reported they could not. When it comes to differentiating between the respiratory symptoms of acute COVID-19, such as dyspnea, cough, ARDS, and hemoptysis, and those associated with long COVID-19, such as chronic cough and abnormal radiographic findings, 60.1% of respondents recognized a difference, 6.5% did not, and 33.4% were unsure.
In identifying cardiac manifestations unique to acute COVID-19, like myocardial injury, myocarditis, cardiomyopathy, and cardiac dysrhythmias, as distinct from post-COVID-19 syndrome symptoms, which may include atypical chest pain, chest tightness, palpitations, and tachycardia, 58.8% of participants agreed, 6.2% disagreed, and 35.0% were unsure.
On the topic of long COVID-19 duration, 90.1% concurred that symptoms extending beyond 12 weeks are indicative of long COVID-19, whereas 9.9% did not, suggesting a broader range of 2 weeks to 6 months could also signal long COVID-19.
Regarding the risk of developing long COVID-19after a positive COVID-19 test, opinions were mixed: 38.8% of respondents believed that anyone who tests positive could develop long COVID, whereas 36.2% disagreed. A majority consider long COVID as a sequel to the acute infection, though 27.4% remained uncertain.
4.3.3. Risk of Developing Long COVID After Testing Positive for COVID-19
Survey responses varied significantly by educational level regarding the risk of developing long COVID after testing positive for the virus. Those with doctoral and master's levels of education were more likely to agree (57.5% and 44.7%, respectively), whereas 49.4% of currently enrolled students disagreed, and 27.3% of diploma holders reported being uncertain, X2 = 22.39, P < 0.05.
4.3.4. Brain Fog as a Long COVID Symptom in the Elderly, Severity, Long COVID Symptoms, and Population at Risk
There was a significant difference in the agreement among participants regarding brain fog, a symptom frequently reported in the elderly, with 80% of those holding a doctoral degree, 62.7% of currently enrolled students, and 41.2% with a master's degree acknowledging its prevalence. This was followed by 47.3% of bachelor's degree holders and 36.4% of those with a diploma (X2 = 30.70, P < 0.05).
In discussing the development of long COVID-19 symptoms, 67.9% (n = 295) of participants agreed that patients who had more severe COVID-19 illnesses were at the highest risk. Meanwhile, 65.21% (n = 283) disagreed, suggesting that patients with existing comorbidities were at greater risk, and 60.83% (n = 264) believed older patients were more susceptible. Further results indicated that 36.64% (n = 159) of participants considered young adults at risk, 26.73% (n = 117) identified females, 22.11% (n = 96) pointed to males, and 6.68% (n = 29) were unsure of the most at-risk group.
Regarding the development of the most severe long COVID-19 symptoms, 76.96% (n = 334) concurred that severely ill and hospitalized patients and 76.04% (n = 330) believed that patients with comorbidities such as asthma and diabetes, were most likely to experience severe symptoms. Additionally, 61.6% (n = 265) attributed a higher risk to older patients, while 26.04% (n = 113) specifically mentioned gender, with females perceived as more at risk, and 23.50% (n = 102) believed men were more likely to develop severe long COVID-19 symptoms.
4.4. Experience Domain
4.4.1. Frequency and Timing of Cases Encountered and Symptoms of COVID-19
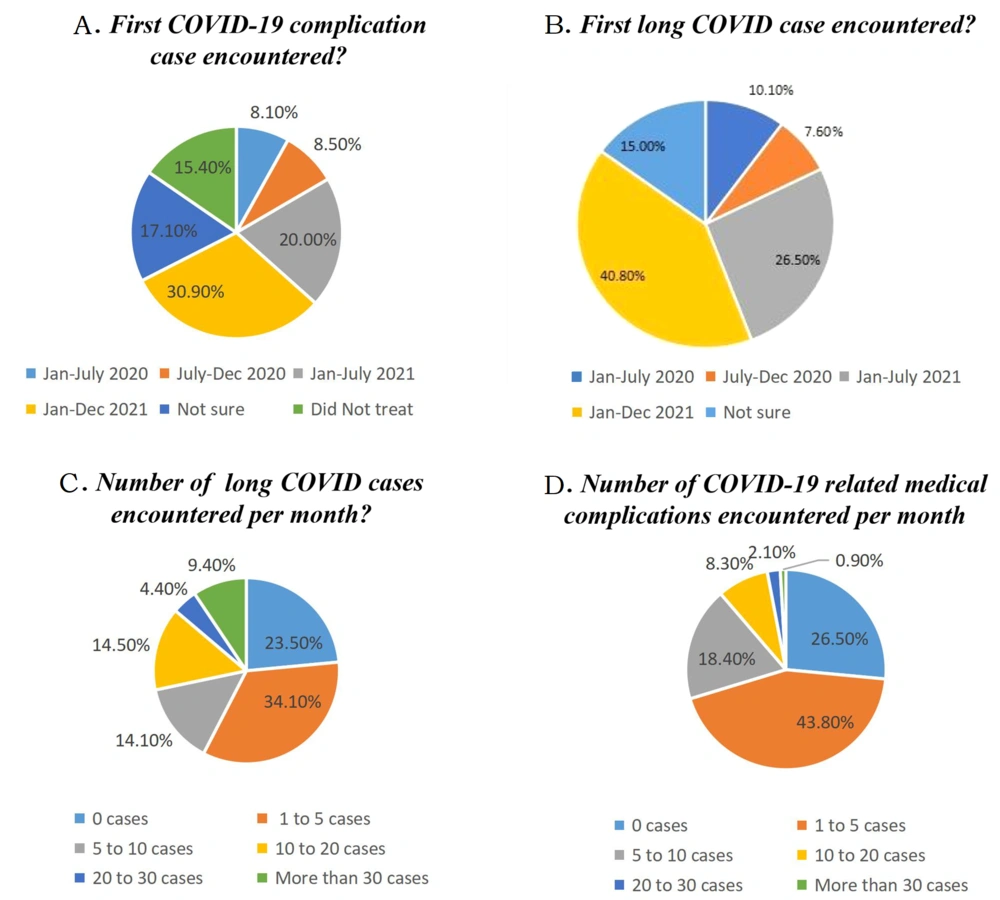
Our survey indicated that the respiratory system (48.8%) was the most commonly affected system in long-term COVID patients, followed by the musculoskeletal (28.3%) and neurological systems (13.4%) among those referred to physiotherapy services. To gain insights into the experiences of the physiotherapy community with managing long-term COVID-19 and COVID-19 complications alongside regular medical care, their initial encounters were documented. The first instances of COVID complications and long COVID treatment spanned from January to July 2020, with the majority reporting 1 - 5 cases in both categories per month (Figure 1A - D).
4.4.2. Most Common COVID-19 Complications Treated by Physiotherapy Services
Pneumonia emerged as the most prevalent complication, affecting 79.26% of participants (n = 344). Other notable complications included ARDS (63.36%), neurological injury (52.07%), acute cardiac injury (18.89%), and acute liver injury (12.90%), with additional issues such as fatigue, general weakness, muscle weakness, motor impairment, and foot drop reported by 0.2%.
4.4.3. Most Common Populations Referred to Physiotherapy with Long COVID
The survey responses revealed that 75.12% (n = 326) of participants encountered severely ill and hospitalized patients, and 71.66% (n = 311) treated patients with comorbidities. This was followed by older patients (58.29%), females (16.89%), males (26.72%), and young patients (26%).
4.4.4. Long COVID Symptoms and Systems Referred for Physiotherapy
A significant portion of participants (65%) reported treating patients with long COVID symptoms persisting for three months, while 24.42% were uncertain, and 11% disagreed. The most frequently encountered long COVID symptoms in physiotherapy settings are listed in Table 1.
| Long COVID-19 Symptoms | Very Frequently | Somewhat Frequently | Less Frequent | Not at All |
|---|---|---|---|---|
| Fatigue | 76 | 19.8 | 1.6 | 2.5 |
| Shortness of breath | 56.2 | 36.2 | 5.5 | 2.1 |
| Cognitive dysfunction | 34.6 | 31.8 | 22.6 | 11.1 |
| Muscle weakness | 51.8 | 35.7 | 9.9 | 2.5 |
| Joint pain | 43.8 | 37.3 | 14.7 | 4.1 |
| Pain in the limbs | 38.5 | 38.0 | 19.4 | 4.1 |
| Chest pain | 34.8 | 38.2 | 21.2 | 5.8 |
| Cough | 38.0 | 32.5 | 22.8 | 6.7 |
| Palpitations | 15.4 | 34.3 | 36.6 | 13.6 |
| Headache and attention disorder | 22.1 | 30.2 | 32.0 | 15.7 |
| Hearing loss or tinnitus | 10.4 | 18.2 | 41.7 | 29.7 |
| Autonomic dysregulation and heartache during exercise | 13.1 | 24.9 | 34.8 | 27.2 |
Long COVID-19 Symptoms Most Encountered by Survey Respondents During Physiotherapy Practice a
4.4.5. Instruments Used in Respiratory Care
Pulse oximeters (41.2%) were highly used, and other devices used for respiratory management for long COVID management were outlined in Table 2.
| Respiratory Devices | Very Good | Sufficient | Rather Sufficient | Insufficient |
|---|---|---|---|---|
| Pulse Oximeter for O2 saturation in blood | 41.2 | 33.2 | 18.4 | 7.1 |
| PEP (positive expiratory pressure such as Flutter, Acapella) devices to improve collateral ventilation | 30.4 | 32.7 | 24.4 | 12.4 |
| Respiratory muscle training devices such as respirometer | 30.0 | 28.3 | 26.3 | 15.4 |
| Device for mucus mobilization such as flutter or Acapella | 21.7 | 30.9 | 28.8 | 18.7 |
| Device for measuring respiratory capacity such as respirometry or spirometry | 26.3 | 27.2 | 27.6 | 18.9 |
| A device for measuring the maximum expiratory force, such as a peak flow meter | 22.1 | 29.3 | 27.6 | 21.0 |
| A device for measuring the maximum inspiratory force, such as a respiratory pressure meter | 22.6 | 29.7 | 26.0 | 21.7 |
Physiotherapist's Rating of the Subjects’ Experiences with Respiratory Devices a
4.4.6. Experience in Physiotherapeutic Screening Procedures for Long COVID-19 Patients to Recommend Physical Activity
Among the respondents, 41.47% utilized detailed patient histories to screen for post-exertional symptoms, while 40.78% were unsure of the screening method, 29.95% monitored heart rate, 26.27% did not perform any screening, 8.53% employed the DePaul Post-Exertional Malaise Questionnaire, and 7.14% used a Two-day cardiopulmonary exercise test.
To prevent symptom exacerbation in patients with long COVID, 63.21% of participants preferred graded exercise therapy, 37.79% opted for symptom-titrated physical activity, 31.8% utilized pacing and activity management, 29.95% recommended fixed activity prescriptions, and 12.9% were uncertain.
In terms of screening for autonomic nervous system dysfunction before prescribing physical activity interventions for individuals with long COVID, 42.63% (n = 185) of participants were uncertain, 35.03% (n = 152) monitored heart rate and blood pressure, 33.41% (n = 145) looked for signs of orthostatic intolerance, 29.95% (n=130) noted symptoms like palpitations and tachycardia, 29.03% (n = 126) did not screen for autonomic dysfunction, 14.29% (n = 62) used the Physical Activity Readiness Questionnaire, and 11.29% (n = 49) conducted a Physical Activity Readiness Medical Examination.
4.4.7. Experience in Diagnostic Laboratory Tests, Assessment, Functional Tools, and Education in the Rehabilitation of Long COVID-19
Physiotherapists deemed tests for rheumatoid factor, C-reactive protein, ESR, and ferritin very important (44.2% and 44.0%, respectively) for rehabilitating long COVID patients, while D-dimer and fibrinogen tests were considered somewhat important (38.9%). Other laboratory tests, such as those for vitamin deficiencies, myocardial injury, and tests to differentiate symptoms of cardiac versus pulmonary origin, were also utilized.
The General Functional Status and Quality of Life Tools and the Post-COVID-19 Functional Status Scale (PCFS) were highly valued (51.6% and 41.7% respectively). The Fatigue Severity Scale, Insomnia Severity Index (ISI), and tools for neurological conditions were rated very important by 38.2% to 39.2% of participants, and tools for psychiatric conditions were deemed somewhat important by 29% of respondents.
Exercise capacity tests (71.9%), balance and risk of falling scales (54.6%), and blood pressure assessments (45.4%) were highlighted as crucial functional testing tools for the rehabilitation of long-term COVID-19. The most advocated lifestyle modifications included aerobic exercise (83%), a healthy diet (71.9%), and strength training (56.5%).
4.4.8. Tele-rehabilitation for Long COVID
Our survey reveals that 73.5% of participants have not utilized telerehabilitation for managing long COVID, whereas 16.29% have employed it, and 9.21% remain uncertain. Among those who have experienced telerehabilitation, Zoom was the most frequently used platform, with Google Meet, webinars, Edomo, and GoToMeeting also being popular choices.
4.4.9. Attitudes Toward Long COVID Rehabilitation
The majority agree that breathing exercises, strength training, and aerobic exercises can be effectively conducted via telerehabilitation; however, 24.2% are uncertain about the efficacy of aerobic exercises, and 21.9% question the feasibility of strength exercises through this medium.
4.4.10. Tele-rehabilitation Versus Face-to-Face Physiotherapy Sessions
About 37.6% of respondents consider telerehabilitation sessions beneficial for providing physical therapy to long-term COVID patients, while roughly 30% disagree, and 35% are undecided. Regarding effectiveness, 45.4% of participants do not believe telerehabilitation is as effective as face-to-face sessions for long COVID patients, 27.0% agree that it is, and 27.6% are unsure.
4.4.11. Need for Continuing Professional Education
A significant majority of respondents (84.30%, n = 366) see the value in an academic module focused on long COVID rehabilitation, and 67.5% (n = 293) anticipate an increase in long COVID cases. Concerning further education, 87.3% (n = 381) expressed a desire for more information on long-term COVID-19 rehabilitation, and 87.8% (n = 381) showed interest in specialized training.
As for staying informed, 46.1% (n = 200) of the participants feel well-informed about the physiotherapeutic rehabilitation for long COVID, whereas 30.6% (n = 133) do not feel adequately updated or informed, and 23.3% (n = 101) are uncertain.
5. Discussion
Recurrent waves of SARS-CoV-2 and a low level of awareness about Long COVID-19 present a significant public health risk (24). The care for Long COVID necessitates a multidisciplinary approach that spans clinical, physical, mental, and social support, highlighting the importance of Knowledge, Attitudes, and Practices (KAP) studies for future preparedness (7, 24, 25). Reevaluating KAP domains is crucial for addressing current and future health challenges and for developing a resilient healthcare system.
To our knowledge, this study is the inaugural investigation into the KAP of clinical physiotherapists and physiotherapy students with respect to Long-term COVID rehabilitation. To ensure validity, the survey underwent expert review, a pilot phase, and employed cognitive interviewing techniques such as probing and prompting questions. To minimize guessing, we provided additional "not sure" options and "others, please specify" as open-ended responses and varied the types of questions. Expert agreement for each survey item exceeded 90%, affirming the survey's validity. The Cronbach's Alpha value for the survey was α = 0.89, with a 95% confidence interval of (0.88 - 0.91), after excluding ordinal questions with fewer than three answer choices.
Our findings regarding knowledge indicate that the majority of respondents possess a solid understanding of long-term COVID-19 as a sequel to COVID-19 infection, its timeline, and its most common symptoms. These results are consistent with studies by Duncan et al. (2020) (26) and Hayes et al. (2021) (27), which also observed the frequent occurrence of fatigue, respiratory symptoms, and pain among Long COVID cases in studies among allied health professional directors and the general community.
It is encouraging that up to 61.1% of respondents provided knowledgeable feedback about distinguishing between 'acute COVID-19 management and COVID-19 related medical complications' and long-term COVID-19 symptoms. Nonetheless, it remains essential to continue educating the physiotherapy community about the potential long-term effects of COVID-19 to ensure every rehabilitation provider in the team can make informed decisions. The observed knowledge gap might stem from the interchangeable use of the terms Long COVID and post-COVID-19 syndrome at the time the study was conducted.
Including a broad range of participants highlighted how responses varied across age groups and revealed a gap in the attitudes and experiences of younger participants. Those actively pursuing education displayed a notable gap in distinguishing between the management of acute COVID-19 and its medical complications, potentially due to a lack of clinical exposure and updates. Consequently, inter-group comparisons were not performed.
In this study, 19.2% of participants were students currently pursuing their education, with a significant proportion, up to 25% of students, indicating 'not sure' when asked to differentiate between conditions, in contrast to those with qualified levels. This uncertainty can also be attributed to gaps in the curriculum regarding COVID-19 and long COVID physiotherapy. This gap was particularly evident in areas such as identifying the risk of developing long COVID and monitoring symptoms, where students, especially those with supervised practice, mostly expressed uncertainty. A study highlighted a discrepancy between the experience of respiratory physiotherapists in specific examination and treatment techniques and their assessment of these techniques' importance (23).
A high percentage of physiotherapists reported encountering acute COVID-19 complications and long COVID cases, with one to five cases during their practice. Overall, 76.50% of survey respondents encountered long COVID cases, compared to 72.50% who reported COVID-19-related organ failure complications in regular practice. This underscores the emerging nature of long COVID cases with multi-system involvement and the necessity for resilient, comprehensive rehabilitation alongside physiotherapy care systems to address long-term COVID and its complications.
The findings align with other studies (7), showing that participants agree that individuals who experienced more severe COVID-19 illness were at a higher risk of developing long COVID. Recent studies suggest that the risk of developing long-term COVID-19 symptoms extends not only to individuals with severe COVID-19 illness but also to females and young adults (10). In contrast, our survey found that over half of the participants believed that older patients and those with co-existing comorbidities were at greater risk. Understanding the prevalence and identifying populations with multiple risk factors for long-term COVID-19 can enable physiotherapists to determine the most suitable exercise approaches for rehabilitation.
It has been reported that more severe COVID-19 illnesses exhibit significantly more long-term COVID-19 features overall, including cognitive difficulties (9). In our study, a considerable number of participants believed that patients with more severe illnesses, and over half indicated that patients with comorbidities, such as asthma and diabetes are more likely to suffer from long COVID.
Studies have reported mixed results, highlighting the complexity of various risk factors for long COVID (28). The most common long COVID cases referred to physiotherapy involved patients with a history of severe COVID-19 illness and hospitalization, followed by patients with comorbidities, as indicated by survey participants in this study.
To facilitate functional recovery in patients suffering from long-term COVID-19, it is crucial to articulate the systemic effects of long-term COVID-19, its symptoms, and the rehabilitation needs. The most frequently encountered symptoms were fatigue, shortness of breath, muscle weakness, and joint pain, with the respiratory system, musculoskeletal system, and neurological system being the most affected. The majority of participants reported symptoms recognized by the CDC for long-term COVID-19, while only a few mentioned brain fog and memory loss. This suggests limitations in referrals for physiotherapy services (29).
The survey highlighted the significance of various assessment tools for evaluating and monitoring post-COVID symptoms and long COVID rehabilitation. Fewer than half of the respondents deemed specific diagnostic laboratory tests important for long-term COVID patients, suggesting these tests are typically not recommended for post-COVID conditions unless symptoms persist for 12 weeks or more.
Recent evidence points to elevated levels of d-dimer and C-reactive protein being common among long COVID patients (21), yet a majority of survey participants viewed C-reactive protein, ESR, and inflammatory markers as essential diagnostic tools for long COVID. However, only 30.6% considered D-dimer and fibrinogen tests for coagulation disorders as important (21, 28), indicating that physiotherapists depend on laboratory data for exercise prescription and rehabilitation planning. The correlation between these biomarkers and exercise necessitates further research.
Participants in this study emphasized the value of tests such as the 6-minute walk test, 1-minute sit-to-stand test, 2-minute step test, and 10 Meter Walk Test (10MWT) for assessing exercise capacity. This aligns with recent findings that highlight exercise capacity deficits in patients with long COVID-19 (30).
The evaluation indicated that although many participants considered their experience in respiratory rehabilitation sufficient, 30.2% reported their experience as insufficient, and 15.9% had no experience at all. The limited use of respiratory devices, other than pulse oximeters, flutter or Acapella devices, and spirometry, underscores the need for further research into the effectiveness of various devices for respiratory rehabilitation and the necessity for more training in this domain.
It's recommended to exercise caution when prescribing physical activity due to the diverse range of symptoms and clinical courses observed among patients and not to rely solely on guidelines for chronic fatigue syndrome and Myalgic Encephalomyelitis (21). Most respondents recognized that screening is crucial for customizing interventions to meet individual needs and to minimize the risk of exacerbating symptoms before recommending any physical activity as an intervention for people living with long-term COVID-19.
One study revealed that 74.6% of 3,762 individuals with long COVID across 56 countries reported an exacerbation of post-exertional symptoms (PEE) (21). Our survey findings show that approximately 41% of responses indicated the use of medical history for screening for post-exertional exacerbation (PEE), while 41% and 26% indicated ‘uncertainty’ and ‘do not screen,’ respectively, in the screening process, highlighting a significant gap in knowledge and practice.
Post-exertional symptom exacerbation refers to the sudden onset or worsening of symptoms following cognitive, physical, emotional, or social activity, even those previously tolerated (21).
Participants in the survey reported that graded exercise therapy can be safely utilized to prevent symptom exacerbation in patients with long-term COVID-19. The effectiveness of graded exercise therapy for long COVID remains a subject of ongoing research and debate. While tailored graded exercise therapy may be beneficial for gradually improving exercise tolerance and overall functioning in long-term COVID patients, there are cautions against its use due to the potential for symptom exacerbation and individual variability in symptom presentation and progression.
Individuals with long COVID may experience exercise intolerance due to autonomic dysfunction, leading to symptoms such as breathlessness, palpitations, fatigue, chest pain, or feeling faint (21). Screening for autonomic nervous system dysfunction is essential before recommending physical activity as an intervention for individuals with long-term COVID-19, yet our results indicate a significant knowledge gap in this screening process.
In a COVID rehabilitation program, patients should adopt a conservative approach to gradually reintegrate daily activities, prioritizing safety and adapting to their energy levels and symptom limitations. Exercise should prevent excessive fatigue or symptom worsening, both during and after the session. Respondents highlighted a positive approach with the goal of reducing long COVID symptoms.
The COVID-19 pandemic has significantly impacted healthcare delivery, leading to an increased use of telerehabilitation, which includes clinical rehabilitation services focusing on assessment, diagnosis, and treatment (31). However, a smaller portion of our study's participants reported using telerehabilitation for long COVID, while a majority acknowledged the necessity and feasibility of delivering exercise sessions through platforms like Zoom and recognized the need for additional training for anticipated clinical encounters in the future. Our study identified a potential barrier to implementing long COVID-19 rehabilitation programs: A gap in knowledge transfer and training. Most participants acknowledged the need to update academic curricula to address the pandemic and long COVID-19 rehabilitation, echoing the findings of Barbara et al. (2021) (23).
5.1. Limitations
The study had several limitations, including a) online data collection without the opportunity for researcher clarification on responses, b) a lengthy 52-item questionnaire, c) the exclusive use of the English language, d) the reliance on respondents' availability to complete online surveys, e) a mixed sample of students, faculty, and clinical physiotherapists, f) questions about the quality of their responses, such as truthfulness or level of attention, and inaccuracies, and h) yes/no questions, which might not provide comprehensive knowledge. The wide age range of participants might have resulted in an over-representation of less engaged answers among younger participants and affected age-related willingness to participate in the survey. Inter-group and KAP component-specific reliability analyses were not conducted, though age and highest qualifications were used as categorical variables to identify differences.
Cross-sectional surveys generally cannot establish cause-and-effect relationships and are susceptible to bias. Nonetheless, a valid pre-survey process and authenticated survey results ensure representation of the physiotherapy community.
5.2. Clinical Implications
Our findings indicate that academic institutions and professional bodies should act as first responders to develop innovative educational modules and training programs tailored to professionals and individuals recovering from long-term COVID-19.
5.3. Conclusions
Our survey uncovered significant gaps in knowledge and skill transfer regarding long COVID among physiotherapists and physiotherapy students. Additionally, participants reported limited experience in respiratory therapy and the specific screening tools used for rehabilitation. The expressed need for future training programs and educational modules underscores the importance of training on long-term COVID-19 rehabilitation.